Percutaneous mitral commissurotomy (PMC) has been accepted as an alternative to surgical mitral commissurotomy in the treatment of patients with symptomatic rheumatic mitral stenosis. PMC produces good immediate hemodynamic and clinical improvement in most patients with mitral stenosis and the safety and immediate efficacy have been widely demonstrated for > 10 years. However, the consequences of its widespread use are less well known, because large published series report mainly mid-term follow-up 1-4.
The aim of the present study was to describe and analyze long-term clinical and echocardiographic follow-up, in which clinical events are detailed according to the quality of the immediate results.
Material and methods
From January 1993 to December 1994, a consecutive series of 70 patients with mitral stenosis (mean age 38 ± 11) underwent PMC at the Interventional Cardiology Department of the National Institute of Cardiology Ignacio Chávez in Mexico City.
Indications for PMC included New York Heart Association (NYHA) functional class III or IV, and/or echocardiographic findings indicating a moderate to severe mitral stenosis and presence of no more than mild mitral regurgitation (MR). The usual contraindications to the procedure were previously detailed 4-6.
Technique
All procedures were performed via antegrade transvenous approach with the Inoue balloon according to the stepwise technique, under echocardiographic guidance. Balloon size was selected according to body surface area (26 mm if < 1.5 m 2, 28 mm if 1.5 to 1.7 m 2, and 30 mm if > 1.7 m 2). Left ventriculography was performed before and after the last balloon inflation.
Preprocedural and postprocedural assessments
Clinical status was determined by NYHA classification. All patients underwent and Echo-Doppler and transesophageal study before PMC. Evaluation included Wilkins scoring, mitral valve area (MVA) calculation (pressure half-time method), and mitral regurgitation (graded as none, mild, moderate, or severe by color Doppler semiquantitative method). The degree of MR was assessed according to Sellers' classification on left ventriculography in a 30° right anterior oblique view. If a > 1 grade discrepancy in MR grading existed between left ventriculography and Doppler, both studies were reviewed, and a consensus was reached finally.
Follow-up
Clinical follow-up was performed at 1-year intervals since 1993. Clinical evaluation was performed by direct or telephone interview with the patient. The interviewer was masked to the echocardiographic score and immediate outcome of PMC. Follow-up was concluded in January 2005 in 52 of 61 patients (85 %) with a successful procedure, and the median duration was 105 ± 10 months.
Definitions
Good immediate results were defined by a composite end point that associated a mitral valve area > 1.5 cm 2 and regurgitation moderate or less. Clinical improvement after PMC was considered as NYHA class ≤ 2.
End points of follow-up were cardiac death, mitral valve replacement (MVR), repeat PMC, and clinical evaluation according to the New York Heart Association (NYHA) functional classification of congestive heart failure. Restenosis was defined as loss of 50 % of initial gain and MVA < 1.5 cm 2. Survival status was censored at the time of surgery or repeat dilatation.
Statistical analysis
Continuous variables are presented as mean (± SD). Categorical data were expressed as percentages. A value of P < .05 was considered significant. Discrete data were compared by χ 2 analysis and comparisons before and after PMC were made by using paired Student's 2 tailed t test. Event-free survival rate for several single and composite end points was estimated with the use of Kaplan-Meier analysis.
Results
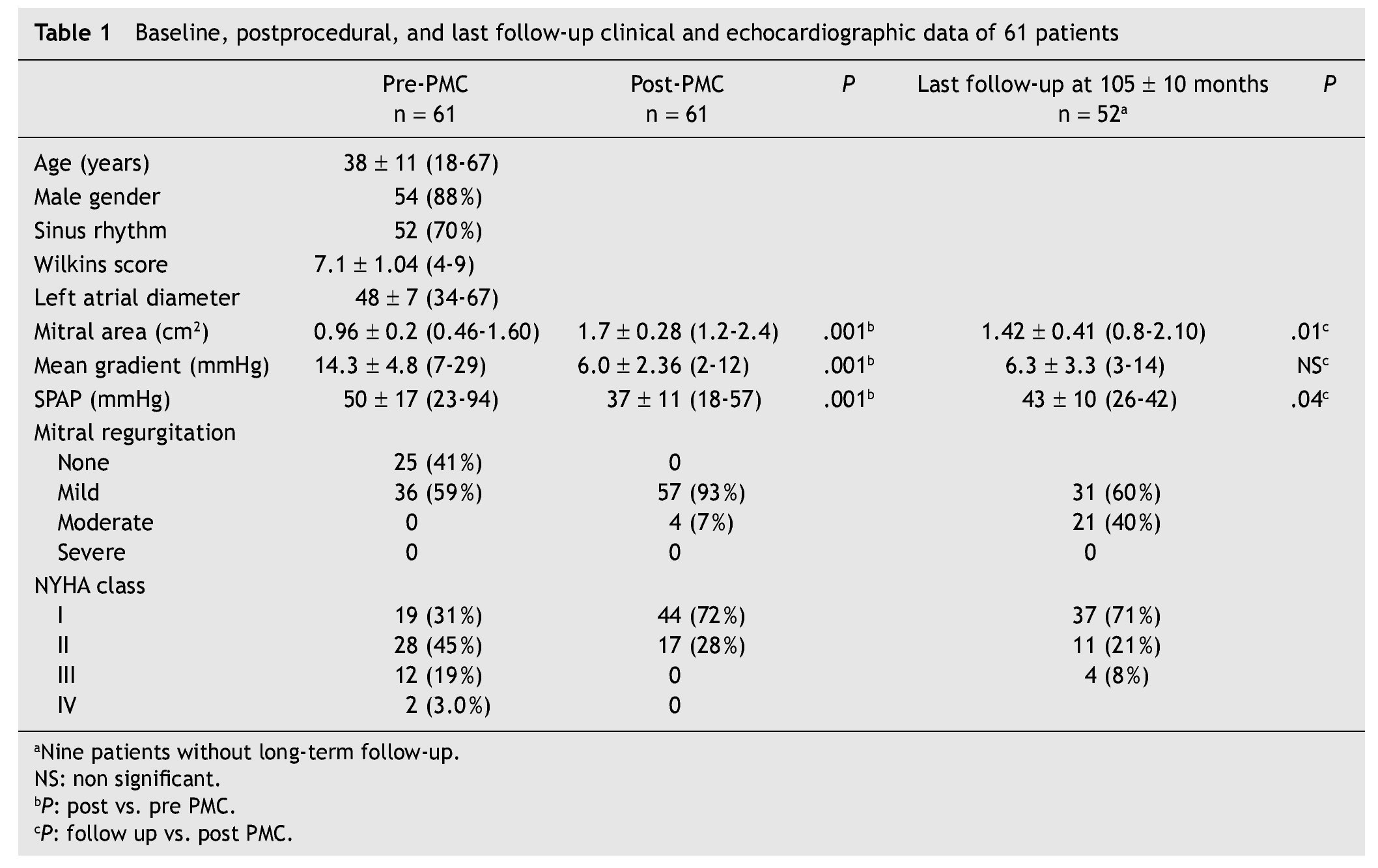
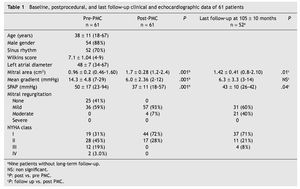
Baseline characteristics and initial results are displayed in table 1. The Inoue balloon diameter was 27.4 ± 2.1 mm. Global results were summarized as good results in 61 (87 %), insufficient opening in 6 (9 %). Severe mitral regurgitation was observed in 3 (4 %) cases and required in-hospital mitral surgery. Two patients showed an atrial septal defect with a Qp/Qs flow ratio of > 1.5:1, which closed spontaneously as demonstrated at 4-year follow-up. No other adverse events occurred.
After PMC, the mean valve area increased from 0.96 ± 0.2 to 1.7 ± 0.28 cm 2 (P < .001) and mean gradient decreased from 14.3 ± 4.8 to 6.0 ± 2.36 mmHg (P < .01). Mitral regurgitation was mild in 44 (72 %) patients and moderate in 4 (7 %) patients. The late MVA was 1.42 ± 0.41 cm 2 and the mean gradient was 6.3 ± 3.3 mmHg (table 1).
Late results
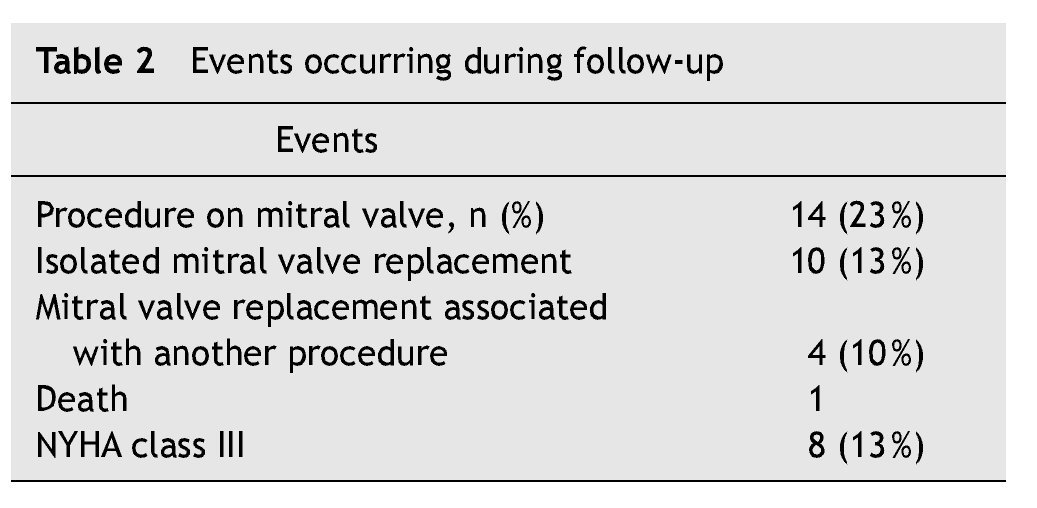
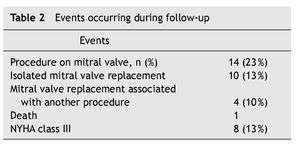
Follow-up events were: (1) death in 1 patient due to a non cardiac cause; (2) mitral replacement in 14 (22 %), 2 patients underwent surgery indicated by mitral regurgitation prosthetic endocarditis in 2, and restenosis in 10. In four patients. it was necessary to replace the aortic valve due to stenosis (table 2).
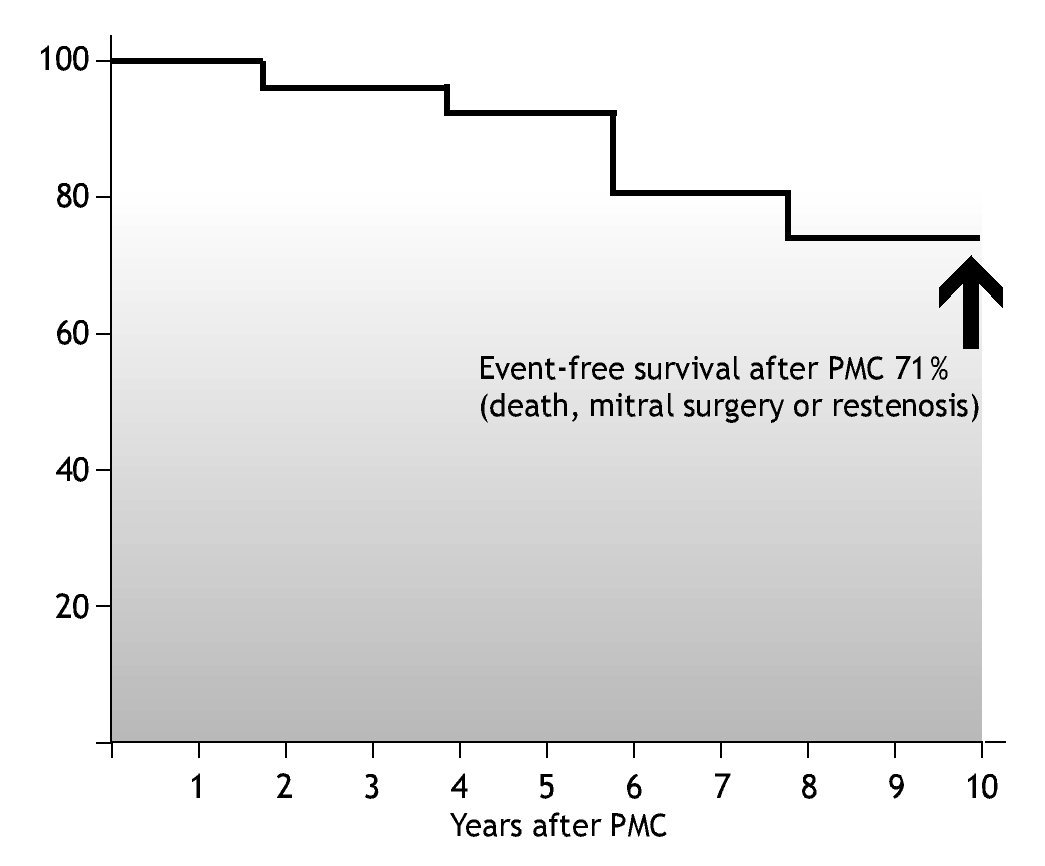
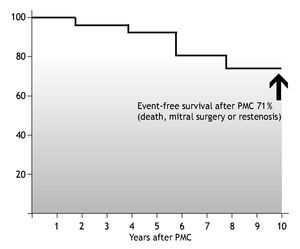
In the 52 patients with follow-up, 10-year actuarial rate was 71 % (37 patients) for survival with no need of surgery or repeated dilatation (fig. 1). In 47 (77 %) patients with ecochardiographic follow-up, restenosis was observed in 24 (50 %) who met the restenosis definition (MVA < 1.5 cm 2) but only 14 were in functional class ≥ 3 and were treated with surgery. Several variables (age, sex, cardiac rhythm, Wilkins score, postprocedural MVA, MR and mean transmitral gradient) were tested as potential predictors of event-free survival or restenosis. None variable were statistical associated probably for small number of patients.
Figure 1 Kaplan-Meier event rate curve showing the cumulative incidence of any major adverse event in the 52 patients at 10 years.
Discussion
Percutaneous commissurotomy techniques have developed significantly since the early attempts of catheter valvuloplasty were pioneered at our institution in the 1950s by Rubio, Limón and Soní 7. Today, PMC for mitral stenosis is considered the method of choice in selected patients for several reasons. First, PMC is a nonsurgical method with results similar to those of surgical intervention but without the unnecessary risks and complications of general anesthesia and an extracorporeal circulation pump. Second, both acute and long term results of randomized trials comparing PMC vs. surgical commissurotomy are comparable and depict similar restenosis rates 4-14.
The overall success rate has been 95 % in several studies, and the "hospital" (30-day) mortality rate was 4.5 %. The early death rate is similar to that observed by other investigators (from 1 % to 9 %) and in the multicenter NHLBI Registry 15.
Our study demonstrates that PMC for MS was successfully completed in 87 % of patients in whom it was attempted. The actuarial 10-year survival was 98 %; the event-free survival was 71 % in the 52 patients that completed follow up. Most of the patients were functionally improved initially; this improvement was largely maintained on further follow-up.
In several studies Wilkins score was the best periprocedural predictor of mitral opening, but the procedural result (mitral area and regurgitation) was the most important independent predictor of major event-free survival. Other independent predictors of major adverse cardiac events were atrial fibrillation, pulmonary artery wedge pressure (PAWP) greater than 18 mmHg and moderate to severe tricuspid insufficiency 11-24.
Our report involves PMC in a population of mostly middle-aged men with a low Wilkins score, this fact explains the favorable results, with a low incidence of complications. Some increases in regurgitation were observed at follow-up, but severe MR was a rather unexpected complication. In our study, we found a 46 % with moderate MR, without clinical impairment at 10 years. Clinical implications of stable moderate regurgitation require further investigation in long-term studies. Recently, Kim et al 25 reported long-term prognostic factors of significant MR after PMC. Echocardiographic and clinical follow-up data were analyzed in 380 patients that underwent PMC with the Inoue balloon. The 8-year event-free survival rate was significantly lower in patients with significant MR than in those without (47 ± 8 % versus 83 ± 3 %, P < .001) and was significantly higher in patients with commissural versus noncommissural MR (63 ± 11 % versus 29 ± 11 %, P < .001). Of the 47 patients with significant MR, who were followed for 74 ± 29 months, 19 patients (40 %) underwent mitral valve replacement, and 28 patients (60 %) received medical treatment only.
Restenosis is an ambiguous definition that includes a mixture of poor results, very early area loss, true restenosis and disease progression. Its definition can be made on a clinical basis or in terms of mitral area. In several studies, the rest-enosis rate after PMC has ranged from 3 to 50 % at 1 to 3 years. Our study demonstrated 24 (50 %) patients with echocardiographic restenosis but only 25 % with clinical deterioration.
Several studies are available regarding long-term follow-up of PMC, the long- term event-free survival was between 75 % and 97 % and depended on the length of follow-up. In our study, the event-free survival was of 71 % at 10 years.
Other studies have reported 4- and 5-year results after PMC. Cohen et al 20 and coworkers reported follow-up data on 145 patients for a period averaging 36 ± 20 months. The actuarial 5-year survival was 76 %, and actuarial event-free survival was 51 %, which is lower than that seen in the present study.
In the preliminary report from the NHLBI Registry, at a mean follow-up of 3.2 years, at 4 years the actuarial survival was 84 % and the actuarial event-free survival was 60 % 15.
Multivariate predictors of mortality included NYHA class IV, higher echocardiographic score, higher postprocedural PA systolic pressure, and higher left ventricular end diastolic pressure 19-41.
Our study has some limitations. First, it concerned a single center cohort study, although patients were representative of a population that underwent PMC contemporaneously. Second, information concerning long-term follow up was available in only 52 patients (85 %).
Our data show that the 10-year results of PMC are good in selected subgroups of patients. These findings of favorable mid-term results strengthen the previous conclusions that PMC should be the procedure of first choice in selected patients in centers with experience and skill in performing this procedure.
Conclusions
PMC is a safe and effective procedure for patients with mitral stenosis. This single-center series confirms the long-term efficacy of PMC in a large population comprising a variety of patient subsets. Patients with a good score obtain better initial and long-term results. Continuing good results can be expected in patients with favorable characteristics.
*Corresponding author.
Correo electrónico: maulm@yahoo.com (M. López Meneses).
Recibido el 31 de octubre de 2007;
aceptado el 19 de septiembre de 2008.