Introduction
Chronic obstructive pulmonary disease (COPD) is currently one of the respiratory diseases that consumes the largest amounts of health care resources and generates high rates of morbidity mortality.1-5 Because this chronic, incapacitating process carries a heavy psychological and social burden, its management should be approached from the perspective of a biopsychosocial model of health care.6-8
Traditionally, the impact of COPD has been evaluated with objective methods (changes in clinical course, spirometry, PaO2, CO2 retention, etc.), which were considered more reliable and readily quantifiable. Methods based on the subjective perception of illness were neglected, as they were classified as less reliable and less easily quantifiable.
Given the discrepancies we found between subjective and functional measures in patients with COPD, the low variation in functional parameters after treatment or rehabilitation programs, and the improvements in subjective indexes and activity measures, the study of quality of life in these patients has recently attracted interest.9-13 Health-related quality of life is considered a multidimensional concept that takes all areas of the individual into account and makes it possible to better know and treat patients with chronic diseases.8,14-19 This concept can be quantified with specific instruments that usually take the form of a questionnaire. Many such instruments are currently available; their validity has been recognized and they have been adapted for use internationally. Some have been translated into Spanish and validated for settings in Spain; this makes it unnecessary, in many cases, to develop new measurement instruments which moreover may make it impossible to compare results obtained with different tools.1,20,26-29
These instruments are classified into two main groups on the basis of their function and objectives: generic (applicable to general detection and screening studies, and to the evaluation of treatments or interventions) and specific (which evaluate the effects of a specific disease, quality of life dimension or population group).
The aims of the present study were to analyze the relationship between an objective health measure based on respiratory parameters (recent spirometry) and subjective measures of patients´ self-perceived quality of life obtained with a generic questionnaire (Nottingham Health Profile) and an instrument designed specifically for respiratory diseases (St. George´s Respiratory (Questionnaire). A further objective was to evaluate the correlation between these 2 instruments for evaluating quality of life.
Material and methods
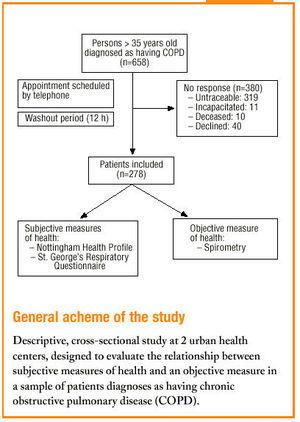
This descriptive cross-sectional study was done in 2 urban health centers (the Palma-Palmilla Health Center and El Palo Health Center, located in the Malaga Health District, Malaga province, southern Spain) with ongoing programs for chronic diseases, and a specific subprogram for COPD.
Study population
The criteria for inclusion were age older than 35 years and prior diagnosis of COPD by professionals at either of the two participating health centers. The diagnosis of COPD was confirmed in the patient´s record as the inclusion of COPD in the patient´s list of problems or as the presence of information on clinical or functional (spirometric) criteria as part of the patient´s long-term management. Exclusion criteria were: a) age less than 35 years, since asthma can occur in any age group (mean age 29.6 years) whereas COPD is usually manifested in older patients; b) airway obstruction with a specific diagnosis of asthma, bronchoectasias or cystic fibrosis, which are explicitly excluded in the Sociedad Española de Patología Respiratoria (SEPAR) and American Thoracic Society (ATS) definitions of COPD22, and c) noneligibility for coverage by Basic Health Zone services at the time of the study despite fulfillment of the above inclusion criteria.
The total population of patients who satisfied all inclusion criteria was 658; the number of patients who actually participated was 278. Reasons for nonparticipation are summarized in Table 1.
Data collection
Study units were defined according to the basic health zone from the list of patients served by each center. Patients with respiratory disease were initially selected for inclusion if they were so identified in the center´s database by a specific code. Some of the variables were recorded from information in the patient´s record, which also provided the phone number used to contact each patient. An appointment was arranged by telephone (minimum of 5 tries); the patients were given information about the nature and aims of the study, and were told that participation was voluntary and that all data would be kept confidential. They were asked to refrain, if their clinical condition permitted, from taking any bronchodilating medication for 12 h before the interview (washout). They were also asked to bring their current medication to the interview. In the course of a personal interview (mean duration 30 min) with each participant the data sheet was completed, questionnaires were administered, and spirometric measurements were obtained.
The sample units were based on patient lists that were up to date as of 15 December 1998. The data were recorded between 18 January and 11 June 1999.
The variables analyzed in this study were as follows: sociodemographic variables: age, sex, body mass index, marital status, education, employment status; personal history: smoking habit (nonsmoker, active smoker, former smoker, packs per year); concomitant diseases: psychopathological, bone and joint, hypertension, dyslipidemia, diabetes, cardiovascular; prior diagnosis of COPD: clinical, spirometric, both; quality of life: Nottingham Health Profile, St. George´s Respiratory Questionnaire.
Instruments used to measure subjective perception of health: quality of life questionnaires
Two questionnaires were used: a generic (Nottingham Health Profile, NHP) and a specific instrument (St. George´s Respiratory Questionnaire, SGRQ).21,26-30
Nottingham Health Profile, Spanish version.21,26-28 This generic questionnaire measures health status and centers on distress. It is intended for use with patients rather than the general population. Content: 38 items in six dimensions: energy, pain, emotional reactions, sleep, social isolation and physical mobility. It is complemented by a second part consisting of seven questions about health-related limitations in seven daily life activities. Administration: self-administered, personal interview, or phone interview. In the present study this questionnaire was administered by personal interview because of the characteristics of the study population (high illiteracy rate, elderly patients). The mean time needed per participant to complete the questionnaire was 10 min. Scoring: Each dimension is scored separately. Positive responses in each dimension are multiplied by an appropriate loading factor, added and scaled on a range from 0 (best possible status) to 100 (worst possible status). Population-based reference standards are available for the general population of Great Britain (for subjects 20 years of age and older) and for Barcelona (40 years and older). Validity: comparative studies for the general population and for patients have found a high degree of validity. Reliability: internal consistency is high but lower than 0.9 for all dimensions. Test-retest validity is also high for all dimensions. Sensitivity to change: evaluated in several observational studies.
St. George´s Respiratory Questionnaire, Spanish version.21,29,30 This is a specific questionnaire for patients with respiratory disease. Content: 50 items (76 levels) in three scales. Symptoms: frequency and severity of respiratory symptoms. Activity: questions and statements about limitations in activity due to dyspnea. Impact: studies psychological and social function alterations caused by respiratory disease. Scoring: Scores are obtained for each scale and for the global result. The scale of scores ranges from 0 (no alteration in quality of life) to 100 (maximum alteration). Administration: self-administered and personal interview. In the present study this questionnaire was administered by personal interview. The mean time needed per participant to complete the questionnaire was 10 min. Validity: content validity is high. Construct validity: high for patients with COPD, with a high correlation between dyspnea and a moderate correlation for FEV1, PaCO2 and PaO2 values. High correlation with the SF-36 Questionnaire and the NHP. Reliability: internal consistency for all scales is higher than 0.7, making it possible to use the scores in group comparisons. Internal consistency for the global score is greater than 0.9. Test-retest validity is currently being evaluated. Sensitivity to change: currently being evaluated.
Objective measure of health: spirometry23-25
Spirometric values were obtained at the time of the interview by one of the interviewers, who had received appropriate training. A portable Pony Graphic apparatus was used to obtain static and dynamic measures of pulmonary function, in accordance with the device´s operating conditions (temperature range 5-24 ºC, maximum relative humidity 90%, avoid use in smoky or dusty areas, do not locate near heat sources). Appropriate maintenance measures were also used throughout the study (sterilization of the turbine every 15 sessions). The standardized values were those published for adults by the ECCS-83. The apparatus complies with all SEPAR23 and ATS-9424 requirements for reproducibility (variability for the greatest 2 of 3 acceptable values for FEV1 and FVC<5% or 150 mL), end of test values (no change in volume for 1 s after 6 s of recording) and accumulation time (maximum time 15 s for FVC and 30 s for VC). Measurements were recorded with the patient seated and wearing a nasal clip; at least 3 measurements per patient were obtained to achieve less than 5% variability, and patients were actively urged to expel as much air as they could until the flow rate approached zero or fell below 25 mL/s.
The spirometric variables were considered as:
Quantitative variables: forced vital capacity (FVC), expressed as a percentage; forced expiratory volume in the first second (FEV1), expressed as a percentage of the theoretical maximum value; peak expiratory flow rate (PEF), in L/s; FEV1/FVC ratio, expressed as a percentage; forced expiratory flow in the midexpiratory phase I (FEF25-75%), expressed as a percentage; Vmax25% in L/s; Vmax50% in L/s; and Vmax75% in L/s.
Qualitative variables: categorized according to the SEPAR classification as: mild, moderate or severe pattern of obstruction; and mild, moderate or severe pattern of restriction.
Statistical analysis
Descriptive statistics were used for all variables. For quantitative variables the mean and median were calculated to evaluate main tendency, and the standard deviation was calculated to evaluate dispersion. For qualitative variables we calculated absolute and relative frequencies of each category. 95% confidence intervals were calculated for the mean and the proportion. Spearman´s coefficient (r) was calculated to analyze the correlation between the results obtained with the 2 questionnaires. To evaluate the relationship between the questionnaire results and FEV1 values (mean values expressed as a percentage of the theoretical value) we used the nonparametric Kruskal-Wallis test with Spearman´s correlation coefficient. All analyses were done with the Statistical Package for Social Sciences (SPSS/PC, version 8.0).
Results
Characteristics of the study population
Of the 278 patients who participated in the study. 88% were men. Mean age was 66.9 years (95% CI 65.8-67.9 years). Mean body mass index was 28.4 (95% CI 27.8-28.9).
Most of the patients (87%) were married, 7% were widows or widowers, 4% were unmarried and 2% were separated. The educational level was generally low: 46.7% of the patients could not read or write, 15.7% could read or write but lacked reading comprehension skills, 30.7% had attended primary school, 4.4% had attended secondary school, and 2.2% had attended university. Most of the participants (77.1%) were retired, 6.1% were employed, 4% were unemployed and 12% had never done paid work or were on temporary leave. Of all patients, 76.3% were ex-smokers who had consumed a mean of 53.2 packs/year (median 52, SD 32.4). Of those who had ever smoked, 55.8% continued to do so (mean consumption 61 packs/year, median 57, 95% CI 55.9-66.8 packs/year). Most patients had at least one concomitant disease or disorder; the most prevalent was hypertension (51.8%), followed by cardiovascular disease (34.2%), bone and joint disorders (33.2%), diabetes (25.2%), hypercholesterolemia (21.9%), hypertriglyceridemia (18%), psychopathological disorder (15.8%) and dyslipidemia (15.1%). According to information from the patient record, the diagnosis COPD was based on clinical criteria in 37.4% of the patients, and on clinical plus spirometric criteria in 62.6%.
Description of the objective health measure: spirometry
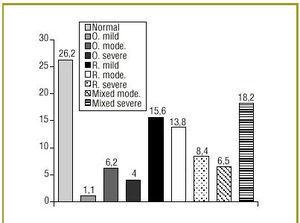
Spirometric measurements obtained at the time of interview were as follows (mean percentage of the theoretical values): FEV1 62.32 (SD 21.98), FEV1/FVC 84.05 (SD 15.89), FVC 73.53 (SD 19.14). All values are shown in Table 2. The automatic diagnosis function of the spirometer, which uses standard values for adults from the ECCS-83, produced the following distribution of spirometric values: 26.2% normal, 11.3% obstructive, 36.5% restrictive, 24.7% mixed. Figure 1 plots these patterns against severity (mild, moderate or severe) according to SEPAR criteria.
Fig 1:Spirometry values at the time of the study, expressed as percentage of participants.Spirometric patterns: O mild: mild obstructive; O mode:moderate obstructive; O severe: severe obstructive;R mild: mild restrictive; R mode: moderate restrictive;R severe: severe restrictive; Mixed mode:moderate mixed; Mixed severe: severe mixed.
Description of subjective measures of health: NHP and SGRQ
The mean scores on the NHP for self-perceived health were highest in the areas that measured sleep (41.9), energy (40) and mobility (36.7). The current health status of our patients caused problems mainly at the workplace (65.9%), with sexual activity (55.2%), housework (36.7%), hobbies (27.7%) and social life (22.7%). Fewer patients reported difficulties with their family life (14%) and holidays (11.2%). The mean total score on the SGRQ (40.9) was higher (indicating worse self-perceived health) than on the NHP (36.7). Quality of life in patients with COPD was most clearly affected in the activity dimension (53.8 points). Table 3 shows the mean scores for each dimension of the NHP and the SGRQ.
Correlation between the NHP and the SGRQ
The correlation between the results each questionnaire yielded, as evaluated with Spearman´s coefficient, ranged from 0.127 to 0.661. In the NHP the areas that evaluated energy and mobility, and the global score, correlated best with the total SGRQ score (0.622-0.657).
The activity dimension of the SGRQ also correlated well with the energy and mobility scores on the NHP (0.647 and 0.661, respectively). The impact dimension of the SGRQ correlated well with the energy and mobility subscales and with total score on the NHP (0.558, 0.552 and 0.532, respectively). The remaining subscales correlated weakly, with correlation coefficients below 0.400. The symptom dimension of the SGRQ showed the poorest correlation with the NHP, with a correlation coefficient below 0.350.
Relationship between objective and subjective measures of health
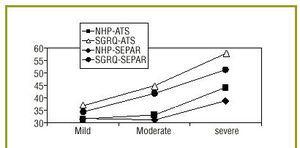
The FEV1 values were categorized according to SEPAR12 and ATS35 criteria, and compared with quality of life as evaluated with the NHP and the SGRQ. As FEV1 decreased, the scores on both questionnaires increased. The correlation between the different dimensions of the SGRQ and the FEV1 categories determined by the ATS ranged from 0.29 for impact to 0.33 for activity. These correlation coefficients were the same when the comparison was based on SEPAR criteria. When we compared total scores on the 2 questionnaires with objective values of respiratory function, the correlation was greater for the SGRQ (r 0.32) regardless of which classification of FEV1 was used. However, different correlation coefficients were found between total score on the NHP and FEV1 as categorized with one or the other system (SEPAR r 0.08, ATS r 0.12) (Table 4). Figure 2 shows the relationship between mean total scores on both questionnaires and mean FEV1 values for the two systems. As FEV1 decreased, the questionnaire scores increased in a more or less linear fashion (indicating decreasing quality of life). The SGRQ produced higher mean scores than the NHP.
Fig 2:Changes in total score on quality of life questionnaires (NHP, Nottingham Health Profile; SGRQ, St. George´s Respiratory Qu estionniare) with different categories of FEV1 according to SEPAR and ATS criteria.
Discussion
The group of patients analyzed in this study constitutes a subgroup within the population of individuals diagnosed as having COPD who were selected from the target population with restrictive selection criteria in order to obtain a well-defined study unit suitable for the aims of our research. The main reason for nonparticipation was our inability to locate some patients because of a change in phone number that was not recorded in the patient´s record.
The sociodemographic characteristics of our patients were similar to those in other studies in Spain.9,44,45 Mean age was 66.9 years and most of our participants were men, findings that corroborates the fact that COPD is manifested in older patients and is more frequent in men.31,32
Chronic obstructive pulmonary disease has been found to be more frequent in the less favored social classes because of the greater numbers of risk factors for the disease.33 The level of education among our patients was low: 62% of the participants were functionally illiterate, a circumstance that may pose obstacles to health education and the use of health care resources.
Smoking is considered one of the most important initial features likely to lead to the identification of chronic moderate airway obstruction.34 Several studies have demonstrated a relationship between cigarette smoking and the onset of COPD or the intensity of respiratory symptoms.35,37 In a prospective study, Badgett, et al.36 identified smoking 70 packs/year or more as a finding that specifically suggested COPD. Patients in the present study who were ex-smokers had consumed a mean of 53.2 packs/year; however, in current smokers the mean number of packs per year had increased to 61. As in all disease processes, a diagnosis of COPD requires an accurate clinical record and physical examination. But to evaluate airway obstruction, tests of pulmonary function are undoubtedly necessary. Such measurements are needed to diagnose the problem, assess its severity and assess the response to treatment. Spirometric evidence of an obstructive pattern of alteration in pulmonary function is indispensable to confirm the diagnosis.4
Of our patients, 62.6% had a prior diagnosis of COPD based on clinical and spirometric findings, according to information obtained from their medical record. In most cases we were not able to trace the spirometric values that led to the diagnosis, as they were not found in the record. These patients may have been diagnosed in a specialized center by respiratory disease specialists, in a hospital emergency service, by spirometric tests done as part of a preoperative work-up or in order to evaluate the patient´s capacity to work, or simply, the results might have been lost.
Of the results of the spirometric tests done at the time of the interview for this study, one of the main findings was that mean values expressed as a percentage of the theoretical value of FEV1 were below 65%, whereas the FEV1/FVC ratio was higher than 70%, a value that does not indicate airway obstruction. Several factors might have influenced the spirometric results. Firstly, in 37% of our patients the diagnosis of COPD was based on clinical criteria only, and obstructive changes do not necessarily appear at the onset of the disease. Secondly, many patients had not complied with the washout period before the interview. In addition, many factors that decrease lung capacity can lead to values that indicate restriction rather than obstruction, by altering the lung parenchyma (pneumonia, resection), the pleura (effusion, fibrosis), the rib cage (deformations, surgery) or the respiratory musculature (especially likely in our patients because of their age). Some of our patients may have been diagnosed as having COPD at a time when they had reversible obstruction due to an episode of worsening asthma, when the lack of follow-up spirometric studies made a correct diagnosis unlikely. Recent studies have shown the importance of follow-up of the decreases in FEV1 for the early identification of these patients (the decrease in FEV1 is less than 30 mL/year in healthy persons, but ranges from 60 to 90 mL/year in persons with COPD).
It was difficult to compare our findings for quality of life with those of other studies done in Spain, because few studies have been published to date on the quality of life in patients with COPD, and because different questionnaires have been used for each study. Moreover, although there appears to be some consensus that FEV1 should be used to evaluate the impact of the disease objectively, there is no consensus regarding the cut-off value for classifying the severity of the disease (i.e., whether the SEPAR, ATS or European Respiratory Society (ERS) recommendations are the most appropriate). This makes comparisons across studies of the same type of patient difficult. Nonetheless, in our study we found no discrepancies between the results obtained with the SEPAR and the ATS criteria.
Scores were elevated (indicating a worse health status) in both the NHP and the SGRQ in the present study. The scores were higher than those reported for the general population,26 although lower than in studies of patients with COPD who had severe airway obstruction.38
In a study of 321 patients with COPD by Ferrer, et al,9 who investigated quality of life with the same questionnaires as we used in the present study, lower scores were found on all dimensions of the SGRQ despite the use of the ATS criteria for percent reductions in FEV1 (which are stricter than the SEPAR criteria) to evaluate severity of the disease. Mean total scores on the NHP for patients with each stage of the disease were also lower than in the present study, meaning that our patients reported greater declines in quality of life. Our results contradict the widely-held opinion that patients with an FEV1 of 50% or less of the theoretical value experience minimal decreases in quality of life35.
The mean total scores obtained with the 2 questionnaires correlated well (r 0.622). The strongest correlations were found for the energy and movement dimensions of the NHP and the activity dimension of the SGRQ. In these areas both questionnaires examine the patient´s physical capacity, which may be influenced by the bone and joint disorders that frequently occur in older persons (33.2% of our patients had such disorders). However, the areas of the SGRQ that specifically investigate respiratory symptoms and the impact of the disease correlated less well with the other dimensions investigated by the NHP, such as pain, emotional reactions, sleep and social isolation. These findings are similar to the results obtained by Harper, et al39 in their comparison of two generic questionnaires, the SF-36 and the EQ, and 2 specific instruments, the (the SGRQ and the CRQ), in 156 patients with COPD. The similarities between these studies support the validity --for the purpose of evaluating changes in health status-- of all the instruments they compared. However, sensitivity was greater for the questionnaires designed specifically for patients with respiratory disease.
Our findings are in agreement with those of a number of studies that have shown that quality of life measures are weakly related with pulmonary function and exercise parameters, with correlation coefficients ranging from 0.1 to 0.5. These coefficients do not differ much from those found for the correlation between traditional measures such as FVC or FEV1 and exercise (for example). However, earlier studies such as those of Pringatano, et al,40 McSweeney, et al41 and Alonso, et al42 failed to find significant associations between FEV1 and the results obtained with other questionnaires, although these authors used generic instruments much less sensitive than the SGRQ. Okubadejo, et al43 reported a linear relationship between PaO2 values and the results of the SGRQ and the CRQ. More recent studies such as that by Hajiro, et al46 reported a direct correlation (r 0.31-0.48) between activity on the SGRQ and FEV1. Monso, et al38 found a significant correlation between FEV1 and the energy, mobility and social isolation dimensions of the NHP. Guell, et al47 noted a weak correlation (r 0.2-0.38) between different dimensions of the CRQ and pulmonary function. A study by Ferrer, et al9 reported a weak to moderate correlation between dimensions of the SGRQ and different categories of FEV1 (0.27-0.51). The highest coefficient was found for the activity dimension, the smallest for disease symptoms. The correlation between total score on the NHP and different categories of FEV1 was weaker (r 0.25) than that found for total score on the SGRQ and pulmonary function (r 0.45).
The tendency found in the study by Ferrer et al9 is consistent with our findings, although the correlation coefficients we obtained were smaller. We believe this difference may be due to the characteristics of our sample, which was composed of «patients who were seen for COPD» at primary health care centers, and who represented a variety of different stages of evolution of the disease. Most studies we reviewed involved patients from hospital settings in whom the existence of airway obstruction as documented by spirometry was a criterion for inclusion; moreover, many such patients had advanced stages of the disease. On the other hand, what we set out to investigate in the present study was the actual situation of primary health care for COPD.
We believe it is important to reach a consensus as to the diagnosis, staging and treatment of patients with COPD, and that new instruments should be developed for clinical practice to evaluate the health-related quality of life in these patients in view of the usefulness of such studies for therapeutic and diagnostic strategies.
Acknowledgments
We express our appreciation to Dr. Jordi Alonso of the Department of Epidemiology and Public Health, Municipal Institute of Medical Research (IMIM) in Barcelona, for his help in obtaining the quality of life questionnaires. We also thank the staff of the El Palo and Palma-Palmilla Health Centers in the Malaga Health District and the patients of these centers who made this study possible.
Correspondence: Francisca Leiva Fernández. C/ Pergolesi 25. 29016 Málaga. España. E-mail: fleiva@hch.sas.cica.es Presented at the XIX Congress of the Spanish Society of Family and Community Medicine. Spanish Society of Family and Community Medicine Prize and talk at the WONCA Congress, Vienna 2000. Manuscript accepted 2 July 2001