To evaluate the impact of computerized clinical practice guidelines on the management, diagnosis, treatment, control, and follow-up of the main cardiovascular risk factors: hypertension, hypercholesterolaemia, and type 2 diabetes mellitus.
DesignPre-post controlled study.
SettingCatalonia, autonomous community located in north-eastern Spain.
ParticipantsIndividuals aged 35–74 years assigned to general practitioners of the Catalan Health Institute.
InterventionThe intervention group consisted of individuals whose general practitioners had accessed the computerized clinical practice guidelines at least twice a day, while the control group consisted of individuals whose general practitioner had never accessed the computerized clinical practice guidelines platform.
Main outcomesThe Chi-squared test was used to detect significant differences in the follow-up, control, and treatment variables for all three disorders (hypertension, hypercholesterolaemia, and type 2 diabetes mellitus) between individuals assigned to users and non-users of the computerized clinical practice guidelines, respectively.
ResultsA total of 189,067 patients were included in this study, with a mean age of 56 years (standard deviation 12), and 55.5% of whom were women. Significant differences were observed in hypertension management, treatment and control; type 2 diabetes mellitus management, treatment and diagnoses, and the management and control of hypercholesterolaemia in both sexes.
ConclusionsComputerized clinical practice guidelines are an effective tool for the control and follow-up of patients diagnosed with hypertension, type 2 diabetes mellitus, and hypercholesterolaemia. The usefulness of computerized clinical practice guidelines to diagnose and adequately treat individuals with these disorders remains unclear.
Evaluar el impacto de las guías de práctica clínica electrónicas en el manejo, diagnóstico, tratamiento, control y seguimiento de los factores de riesgo cardiovascular mayores: hipertensión, hipercolesterolemia, diabetes mellitus tipo 2.
DiseñoEstudio pre-post controlado.
EmplazamientoCataluña, comunidad autónoma situada al noreste de España.
ParticipantesIndividuos de 35-74 años asignados a médicos de familia del Institut Català de la Salut.
IntervenciónEl grupo de intervención estaba formado por pacientes asignados a médicos de familia que accedían al menos 2 veces al día a las guías de práctica clínica electrónicas. El grupo de control estaba formado por las personas asignadas a médicos de familia que nunca habían accedido.
Medidas de resultadoSe realizaron pruebas de ji al cuadrado para detectar diferencias significativas en el seguimiento, control y tratamiento de la hipertensión, hipercolesterolemia y diabetes mellitus tipo 2 entre los individuos asignados al grupo de usuarios y los no usuarios de las guías.
ResultadosSe incluyeron 189.067 individuos, con una edad media de 56 años (desviación estándar 12), de los cuales el 55,5% eran mujeres. Se encontraron diferencias estadísticamente significativas en el manejo, tratamiento y control de la hipertensión; en el manejo, tratamiento y diagnóstico de la diabetes mellitus tipo 2, y en el manejo y control de la hipercolesterolemia en ambos sexos.
ConclusionesLas guías de práctica clínica electrónicas son una herramienta efectiva para el control y seguimiento de los pacientes con hipertensión, hipercolesterolemia y diabetes mellitus tipo 2. La utilidad de las guías de práctica clínica electrónicas en el diagnóstico y adecuación del tratamiento sigue en discusión.
The socialization of evidence-based medicine as the scientific basis for decision making in the field of health technology has promoted the availability of several clinical practice guidelines (CPG). These tools synthesize information about certain pathologies and provide action patterns based on the results of randomized clinical trials or on the consensus of prestigious professionals.1 CPG can facilitate decision-making based on the best available evidence and can decrease unjustified variability in clinical practice. Indeed, they are used at health institutions to improve the quality and effectiveness of health care.2,3
However, in recent years health professionals have not systematically applied the recommendations provided by CPG,4 mainly because of difficulties in accessing the content, out-of-date information, lack of time to consult, unfriendly format, insufficient adaptation to the healthcare environment, and general resistance to change among health professionals.5–9
A strategy that may help to reduce these barriers is to integrate CPG into health providers’ electronic medical records.5 This is the approach used by the Catalan Institute of Health. Since 2004, primary care centers have implemented electronic health records, which are collected and managed using the ECAP software. This resource has recently been complemented with a complex system that integrates an electronic version of CPG (eCPG) developed by the Catalan Institute of Health, transforming the CPG into computerized algorithms in order to facilitate decision making.
The eCPG for hypercholesterolemia (HCOL) was incorporated to ECAP in 2010, while those for hypertension (HTN) and type 2 diabetes mellitus (T2DM) were incorporated in 2011. These eCPG are directly activated from the ECAP and use: (1) structured information about the patient (age, sex, diagnoses, and active prescription), and (2) information about the frequency and results of the explorations. Finally, the software analyzes the control and creates recommendations about the most adequate treatment and management. The eCPG also incorporates safety issues such as interactive alerts regarding drugs contra-indications and interactions.
The eCPG meets key requirements proposed by several authors to guarantee its successful integration into electronic medical records (easy access, reminders to guide the actions of health care professionals, useful feedback to inform healthcare professionals about the appropriateness of their actions). However, the real effect of eCPG on the clinical results of the attended population has not been evaluated in detail.10–16
The objective of the present study was to evaluate the impact of integrating eCPGs for the management, diagnosis, treatment, control and follow-up of three key cardiovascular risk factors (HTN, T2DM and HCOL).
MethodsSettingThis study was performed in Catalonia (Spain), an autonomous community with 7.5 million inhabitants. The Catalan Institute of Health (ICS) is the main health services provider, with 6 million users, and a network of 329 primary care centers with 5848 general practitioners (GP).
Study designWe conducted a before-after controlled study to ascertain the impact of eCPG implementation. The study protocol, and the prevalence and control of cardiovascular risk factors have been described elsewhere.17,18
The study population consisted of all individuals aged 35–74 years who were assigned to the ICS GPs. The intervention group consisted of individuals whose GPs accessed the eCPG environment at least twice a day between June 2010 and December 2012 (eCPG users). The control group consisted of individuals whose GPs had never entered the eCPG environment during this period.
The study protocol was approved by the Ethics Committee of the Institut d’Investigació en Atenció Primària Jordi Gol (authorization # P09/28).
Data for the period before eCPG implementation were collected in 2008–2009 for all three eCPGs. To study the effect of the eCPG on HCOL, we collected data between June 2010 and December 2012; to study the effect of eCPG on HTN and T2DM, we collected data between October 2011 and December 2012.
Variables measuredWe compared the numbers of individuals who met the next criteria before and after the intervention (number after implementation minus number before):
- -
HTN: (1) New diagnoses: individuals with a diagnosis of HTN. (2) New treatments: individuals with a diagnosis of HTN and who were treated. (3) Improvement in control of HTN: individuals with a diagnosis of HTN but whose blood pressure (BP) was under control (systolic BP <140mmHg and diastolic BP <90mmHg). (4) Improvement in control of HTN in secondary prevention: individuals with a history of myocardial infarction, stroke or lower extremity peripheral arteriopathy with a diagnosis of HTN but whose BP was under control (systolic BP <140mmHg and diastolic BP <90mmHg). (5) Individuals with a diagnosis of HTN who had had a BP determination in the previous 12 months.
- -
T2DM: (1) New diagnoses: individuals with a diagnosis of T2DM. (2) New treatments: individuals with a diagnosis of T2DM and who were treated. (3) Improvement in control of T2DM: individuals with a diagnosis of T2DM but whose glycated hemoglobin was under control (<7.5%). (4) Improvement in control of BP in patients with T2DM: individuals with T2DM and whose BP was under control (systolic BP <140mmHg and diastolic BP <90mmHg). (5) Improvement in control of HCOL in individuals with T2DM and no history of cardiovascular disease: individuals with a diagnosis of T2DM without a history of myocardial infarction, stroke or lower extremity peripheral arteriopathy, and whose low density liporprotein (LDL) cholesterol was under control (<130mg/dl). (6) Improvement in control of HCOL in individuals with T2DM in secondary prevention or with proteinuria: individuals with a diagnosis of T2DM and a history of myocardial infarction, stroke, lower extremity peripheral arteriopathy or proteinuria, and whose LDL cholesterol was under control (<100mg/dl). Finally, among individuals with a diagnosis of T2DM, we compared (pre- vs. post-implementation) the numbers of those who had undergone (7) determination of glycated hemoglobin, (8) electrocardiography, or (9) the eye fundus test during the previous 12 months.
- -
HCOL: (1) New diagnoses: individuals with a diagnosis of HCOL. (2) New treatments: individuals with a diagnosis of HCOL and elevated coronary risk who were treated. (3) Improvement in control of HCOL in primary prevention (individuals on treatment): number of individuals without a history of myocardial infarction, stroke or lower extremity peripheral arteriopathy who were on drug treatment and whose LDL cholesterol was under control (<130mg/dl). (4) Improvement in control of HCOL in secondary prevention: individuals with a history of myocardial infarction, stroke or lower extremity peripheral arteriopathy whose LDL cholesterol was under control (<100mg/dl). (5) Among individuals in secondary prevention or who were on lipid-lowering treatment, we compared (pre- vs. post-implementation) the number of individuals who had undergone determination of LDL cholesterol in the previous 12 months.
We also considered registry variables directly associated with the use of eCPG (e.g. coronary risk registry, T2DM risk, proteinuria or secondary prevention of cardiovascular disease).
Variables were collected according to a standardized methodology described elsewhere.17 The information source was the ECAP database.
Statistical analysisContinuous variables are presented as the mean and standard deviation (SD), and the median and interquartile range for non-normally distributed variables. Categorical variables are presented as proportions. All analyses were stratified by sex.
We used the Chi-squared test to detect significant differences in follow-up, control and treatment variables for all three disorders (HTN, T2DM and HCOL) between individuals assigned to GPs eCPG users and non-eCPG users. All analyses were carried out using the R Statistical Package (R Foundation for Statistical Computing, Vienna, Austria; Version 3.2.0).
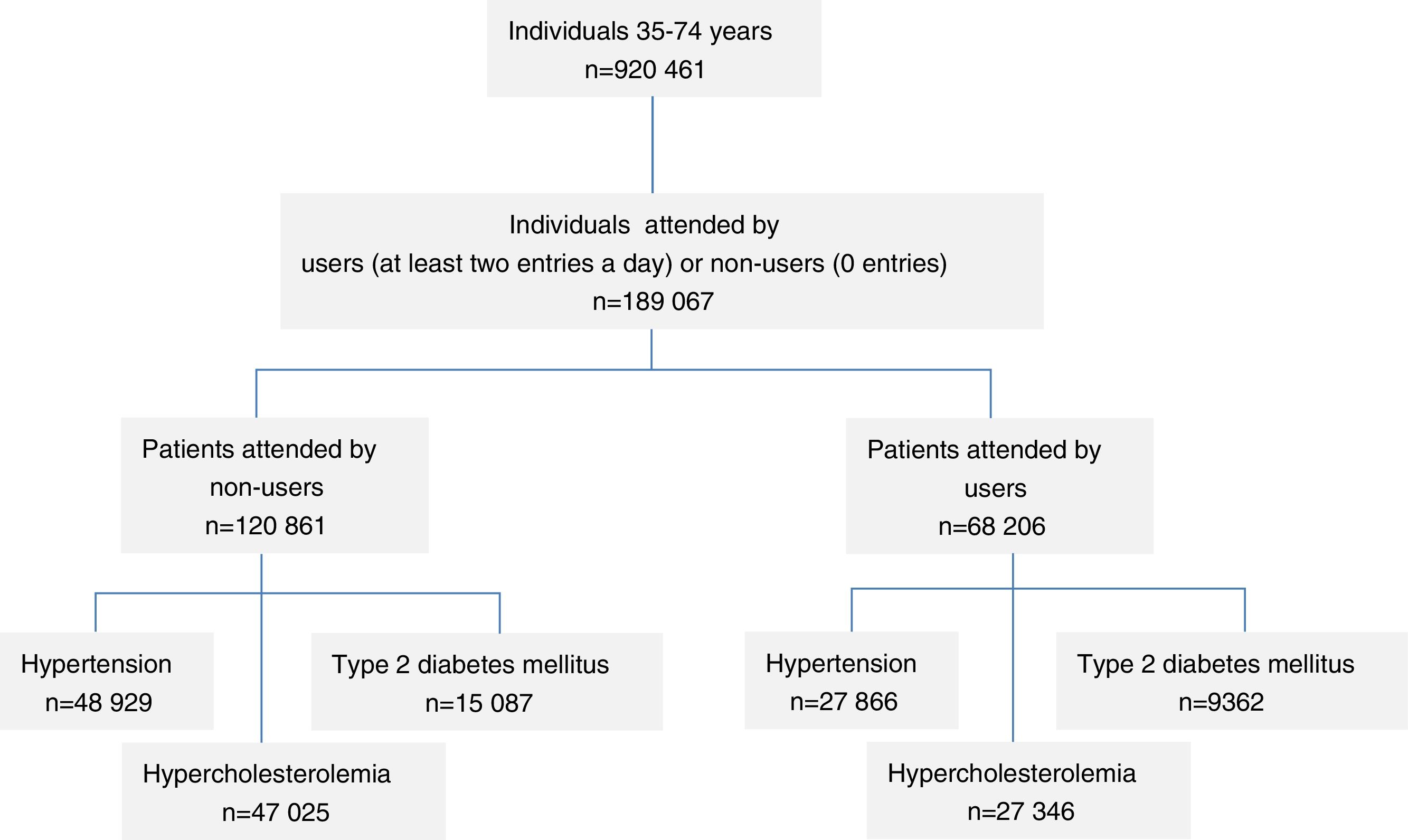
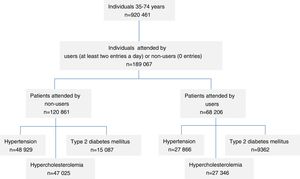
General layout of the studio: Study scheme: Pre-post controlled study. Participants were 35- to 74-year olds assigned to general practitioners of the Catalan Health Institute. The intervention group consisted of individuals whose general practitioners had accessed the electronic clinical practice guidelines at least twice a day, while the control group consisted of individuals whose general practitioners had never entered the electronic clinical practice guidelines environment.
Results189,067 individuals were included, with a mean age of 56 years (SD: 12) and 55.5% women. The intervention group consisted of individuals who were attended by one of 229 GPs eCPG users (5.1% of all ICS GPs), and the control group consisted of individuals who were attended by one of 517 GPs non-eCPG users.
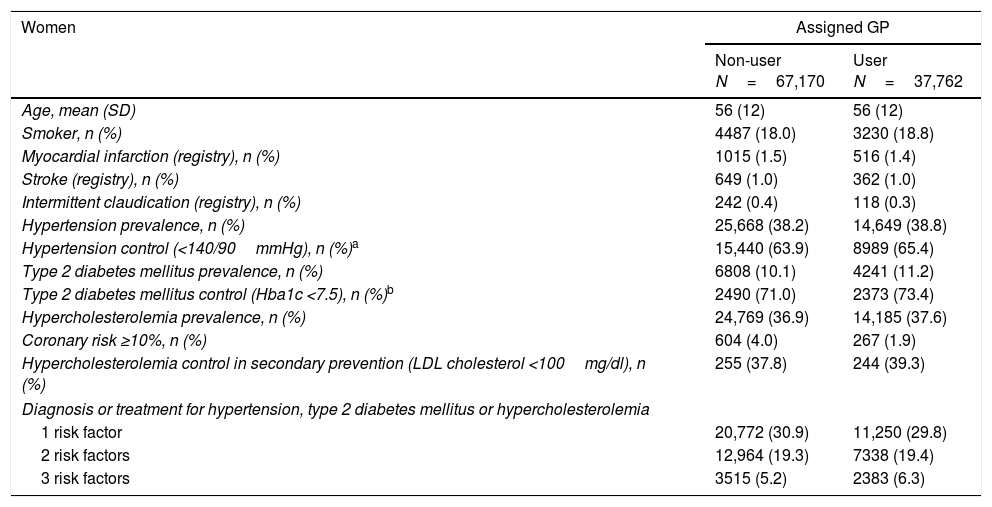
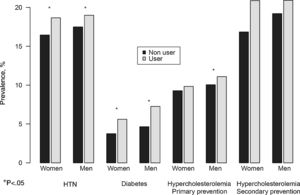
Participants’ baseline characteristics are shown in Table 1. The profile of patients assigned to each group was similar in terms of sociodemographic characteristics, disease prevalence, and control of cardiovascular risk factors. Exceptionally, there was a higher proportion of participants with high cardiovascular risk in the non-eCPG users group (4% vs. 1.9% in women and 14% vs. 12.4% in men). In addition, the prevalence of smokers was slightly lower in the eCPG users group. Control of HTN and T2DM was somewhat higher in the eCPG users group in both sexes, and that of HCOL was higher in secondary prevention in women. The characteristics of this cohort following intervention are provided in Supplementary Table 1.
Characteristics of the participants in the cohort prior to eCPG implementation (2008–2009) according to whether the GP was an eCPG user or non-user.
| Women | Assigned GP | |
|---|---|---|
| Non-user N=67,170 | User N=37,762 | |
| Age, mean (SD) | 56 (12) | 56 (12) |
| Smoker, n (%) | 4487 (18.0) | 3230 (18.8) |
| Myocardial infarction (registry), n (%) | 1015 (1.5) | 516 (1.4) |
| Stroke (registry), n (%) | 649 (1.0) | 362 (1.0) |
| Intermittent claudication (registry), n (%) | 242 (0.4) | 118 (0.3) |
| Hypertension prevalence, n (%) | 25,668 (38.2) | 14,649 (38.8) |
| Hypertension control (<140/90mmHg), n (%)a | 15,440 (63.9) | 8989 (65.4) |
| Type 2 diabetes mellitus prevalence, n (%) | 6808 (10.1) | 4241 (11.2) |
| Type 2 diabetes mellitus control (Hba1c <7.5), n (%)b | 2490 (71.0) | 2373 (73.4) |
| Hypercholesterolemia prevalence, n (%) | 24,769 (36.9) | 14,185 (37.6) |
| Coronary risk ≥10%, n (%) | 604 (4.0) | 267 (1.9) |
| Hypercholesterolemia control in secondary prevention (LDL cholesterol <100mg/dl), n (%) | 255 (37.8) | 244 (39.3) |
| Diagnosis or treatment for hypertension, type 2 diabetes mellitus or hypercholesterolemia | ||
| 1 risk factor | 20,772 (30.9) | 11,250 (29.8) |
| 2 risk factors | 12,964 (19.3) | 7338 (19.4) |
| 3 risk factors | 3515 (5.2) | 2383 (6.3) |
| Men | Non-user N=53,691 | User N=30,444 |
|---|---|---|
| Age, mean (SD) | 56 (12) | 56 (12) |
| Smoker, n (%) | 6709 (36.0) | 4543 (33.7) |
| Myocardial infarction (registry), n (%) | 2973 (5.5) | 1755 (5.8) |
| Stroke (registry), n (%) | 990 (1.8) | 558 (1.8) |
| Intermittent claudication (registry), n (%) | 705 (1.3) | 425 (1.4) |
| Hypertension prevalence, n (%) | 23,261 (43.3) | 13,217 (43.4) |
| Hypertension control (<140/90mmHg), n (%)a | 12,870 (58.8%) | 7547 (60.8%) |
| Type 2 diabetes mellitus prevalence, n (%) | 8279 (15.4) | 5121 (16.8) |
| Type 2 diabetes mellitus control (Hba1c <7.5), n (%)b | 3170 (70.4%) | 3164 (72.9%) |
| Hypercholesterolemia prevalence, n (%) | 22,256 (41.5) | 13,161 (43.2) |
| Coronary risk ≥10%, n (%) | 1877 (14.6) | 1486 (12.4) |
| Hypercholesterolemia control in secondary prevention (LDL cholesterol <100mg/dl), n (%) | 909 (51.6%) | 965 (52.1%) |
| Diagnosis or treatment for hypertension, type 2 diabetes mellitus or hypercholesterolemia | ||
| 1 risk factor | 18,023 (33.6) | 9368 (30.8) |
| 2 risk factors | 11,903 (22.2) | 6966 (22.9) |
| 3 risk factors | 3989 (7.4) | 2733 (9.0) |
GP, general practitioner; LDL, low-density lipoprotein; SD, standard deviation.
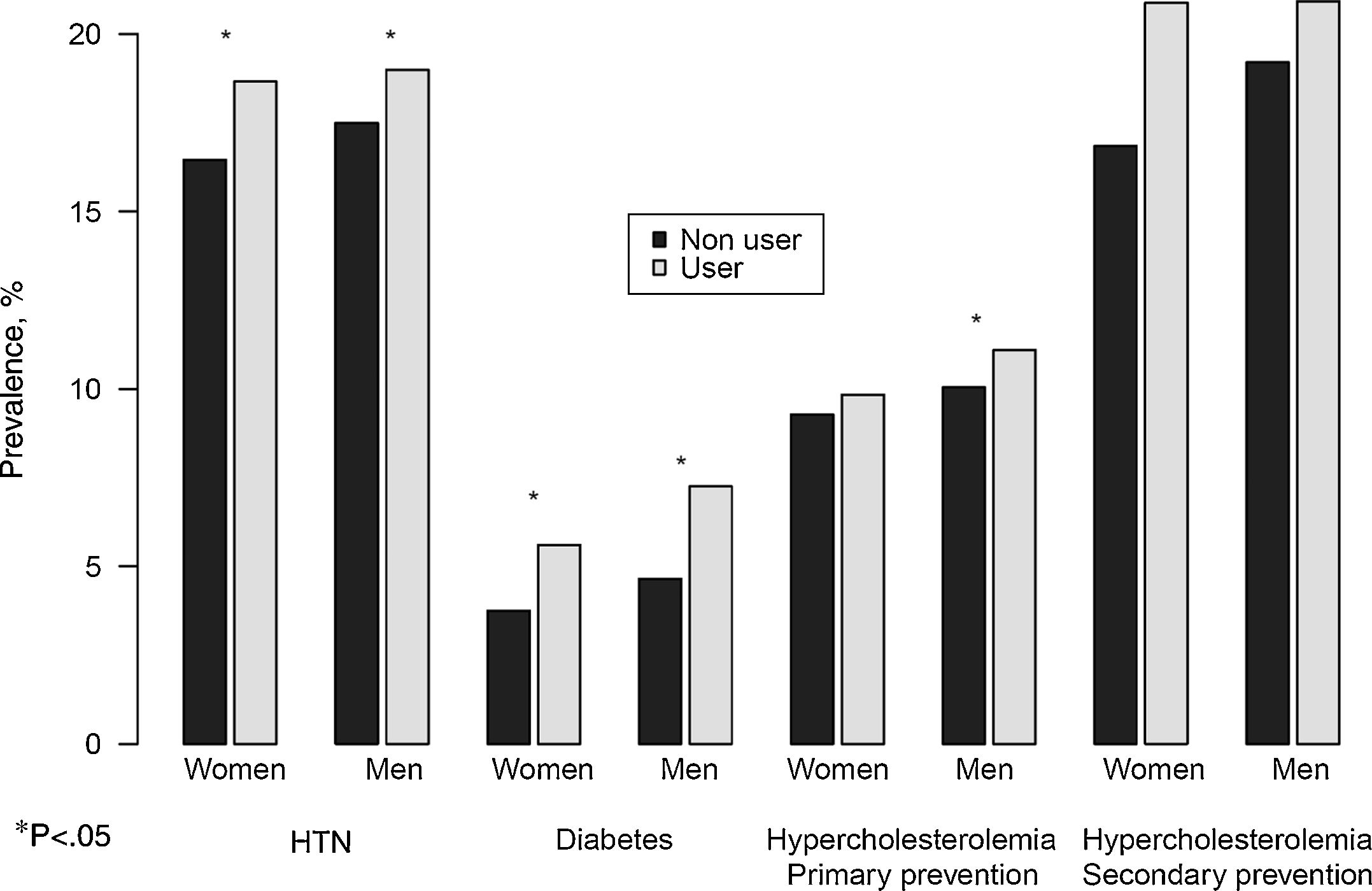
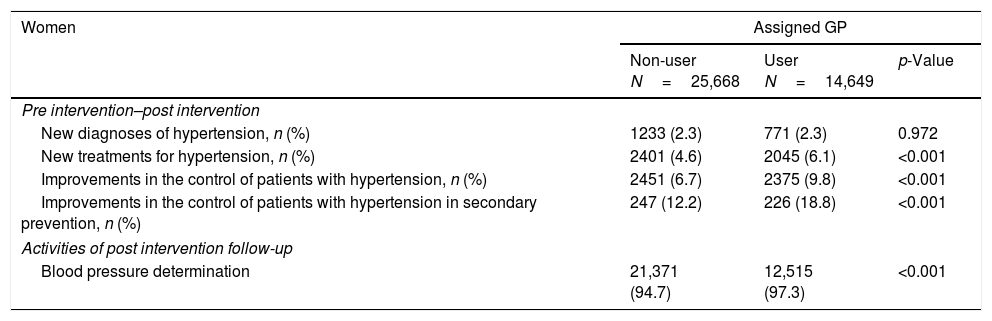
In individuals with HTN (Table 2 and Fig. 1) we observed significant differences in all variables analyzed in favor of the eCPG users group, except for the number of new HTN diagnoses in women. The greatest differences were observed in the control of HTN in individuals in secondary prevention (6.6 and 5.8 percentage point difference in women and in men, respectively).
Pre-post changes in patients diagnosed with hypertension according to whether the GP was an eCPG user or non-user.
| Women | Assigned GP | ||
|---|---|---|---|
| Non-user N=25,668 | User N=14,649 | p-Value | |
| Pre intervention–post intervention | |||
| New diagnoses of hypertension, n (%) | 1233 (2.3) | 771 (2.3) | 0.972 |
| New treatments for hypertension, n (%) | 2401 (4.6) | 2045 (6.1) | <0.001 |
| Improvements in the control of patients with hypertension, n (%) | 2451 (6.7) | 2375 (9.8) | <0.001 |
| Improvements in the control of patients with hypertension in secondary prevention, n (%) | 247 (12.2) | 226 (18.8) | <0.001 |
| Activities of post intervention follow-up | |||
| Blood pressure determination | 21,371 (94.7) | 12,515 (97.3) | <0.001 |
| Men | Non-user N=23,261 | User N=13,217 | p-Value |
|---|---|---|---|
| Pre intervention–post intervention | |||
| New diagnoses of hypertension, n (%) | 1290 (3.1) | 881 (3.4) | 0.010 |
| New treatments for hypertension, n (%) | 2361 (5.7) | 2006 (7.7) | <0.001 |
| Improvements in the control of patients with hypertension, n (%) | 2325 (7.9) | 2305 (11.8) | <0.001 |
| Improvements in the control of patients with hypertension in secondary prevention, n (%) | 536 (12.0) | 524 (17.8) | <0.001 |
| Activities of post intervention follow-up | |||
| Blood pressure determination | 19,531 (94.4) | 11,775 (97.0) | <0.001 |
GP, general practitioner.
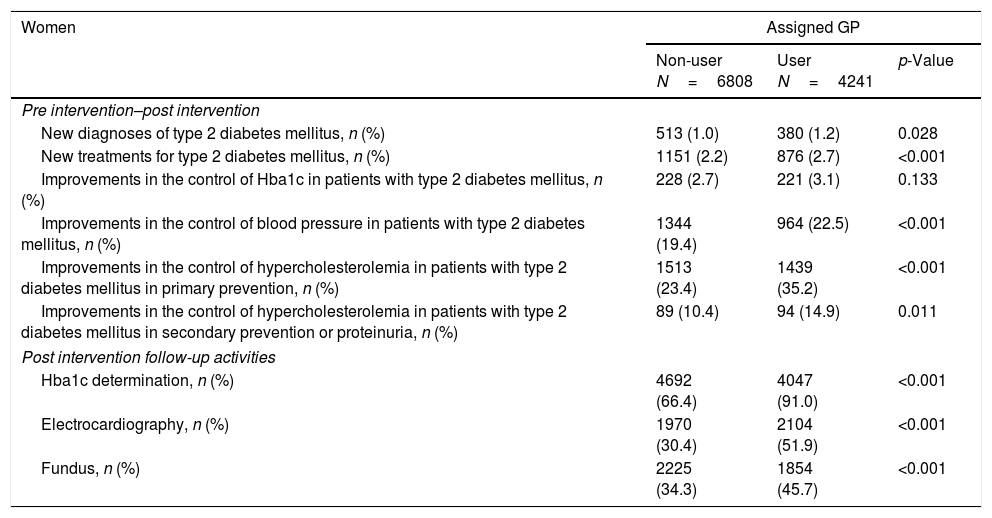
In T2DM, we observed significant differences in all variables analyzed in favor of the group of eCPG users except for the control of glycated hemoglobin in women (Table 3 and Fig. 1). Regarding outcome variables, the greatest differences were observed in the control of hypercholesterolemia in individuals with T2DM in primary prevention (11.8 and 11.5 percentage point difference in women and men, respectively). In addition, we observed significant differences between eCPG users and non-users in the performance of follow-up activities, such as glycated hemoglobin determination, the electrocardiography and the fundus.
Pre-post changes in patients diagnosed with type 2 diabetes mellitus according to whether the GP was an eCPG user or non-user.
| Women | Assigned GP | ||
|---|---|---|---|
| Non-user N=6808 | User N=4241 | p-Value | |
| Pre intervention–post intervention | |||
| New diagnoses of type 2 diabetes mellitus, n (%) | 513 (1.0) | 380 (1.2) | 0.028 |
| New treatments for type 2 diabetes mellitus, n (%) | 1151 (2.2) | 876 (2.7) | <0.001 |
| Improvements in the control of Hba1c in patients with type 2 diabetes mellitus, n (%) | 228 (2.7) | 221 (3.1) | 0.133 |
| Improvements in the control of blood pressure in patients with type 2 diabetes mellitus, n (%) | 1344 (19.4) | 964 (22.5) | <0.001 |
| Improvements in the control of hypercholesterolemia in patients with type 2 diabetes mellitus in primary prevention, n (%) | 1513 (23.4) | 1439 (35.2) | <0.001 |
| Improvements in the control of hypercholesterolemia in patients with type 2 diabetes mellitus in secondary prevention or proteinuria, n (%) | 89 (10.4) | 94 (14.9) | 0.011 |
| Post intervention follow-up activities | |||
| Hba1c determination, n (%) | 4692 (66.4) | 4047 (91.0) | <0.001 |
| Electrocardiography, n (%) | 1970 (30.4) | 2104 (51.9) | <0.001 |
| Fundus, n (%) | 2225 (34.3) | 1854 (45.7) | <0.001 |
| Men | Non-user N=8279 | User N=5121 | p-Value |
|---|---|---|---|
| Pre intervention–post intervention | |||
| New diagnoses of type 2 diabetes mellitus, n (%) | 584 (1.4) | 429 (1.7) | 0.014 |
| New treatments for type 2 diabetes mellitus, n (%) | 1294 (3.2) | 1082 (4.2) | <0.001 |
| Improvements in the control of Hba1c in patients with type 2 diabetes mellitus, n (%) | 346 (4.0) | 386 (4.8) | 0.010 |
| Improvements in the control of blood pressure in patients with type 2 diabetes mellitus, n (%) | 1683 (19.7) | 1236 (22.3) | <0.001 |
| Improvements in the control of hypercholesterolemia in patients with type 2 diabetes mellitus in primary prevention, n (%) | 1743 (21.5) | 1758 (33.0) | <0.001 |
| Improvements in the control of hypercholesterolemia in patients with type 2 diabetes mellitus in secondary prevention or proteinuria, n (%) | 353 (17.3) | 401 (26.4) | <0.001 |
| Post intervention follow-up activities | |||
| Hba1c determination, n (%) | 5841 (66.2) | 5239 (90.8) | <0.001 |
| Electrocardiography, n (%) | 2551 (30.7) | 2870 (52.7) | <0.001 |
| Fundus, n (%) | 2787 (33.6) | 2514 (46.2) | <0.001 |
GP, general practitioner.
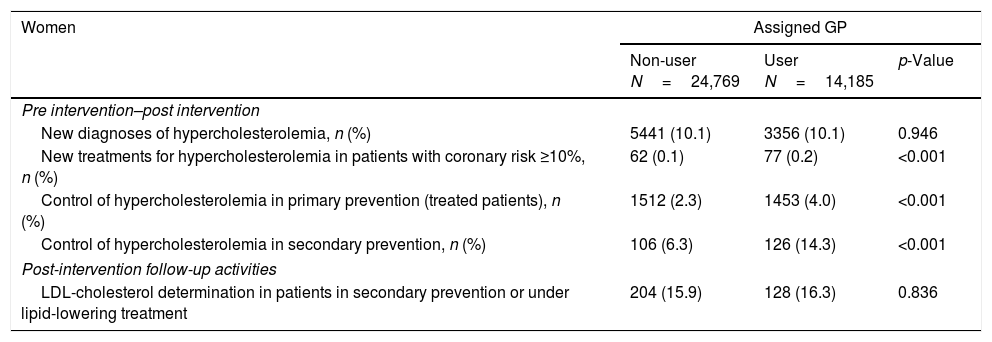
We did not observe any marked differences in the number of new diagnoses or new treatments among individuals with HCOL (Table 4 and Fig. 1). In contrast, the percentage of individuals who achieved good control was higher in patients assigned to eCPG users, both in primary prevention (1.6 and 1.9 percentage point difference in women and men, respectively), and particularly in secondary prevention (8.0 and 7.7 percentage point difference in women and men, respectively).
Pre-post changes in patients diagnosed with hypercholesterolemia according to whether the GP was an eCPG user or non-user.
| Women | Assigned GP | ||
|---|---|---|---|
| Non-user N=24,769 | User N=14,185 | p-Value | |
| Pre intervention–post intervention | |||
| New diagnoses of hypercholesterolemia, n (%) | 5441 (10.1) | 3356 (10.1) | 0.946 |
| New treatments for hypercholesterolemia in patients with coronary risk ≥10%, n (%) | 62 (0.1) | 77 (0.2) | <0.001 |
| Control of hypercholesterolemia in primary prevention (treated patients), n (%) | 1512 (2.3) | 1453 (4.0) | <0.001 |
| Control of hypercholesterolemia in secondary prevention, n (%) | 106 (6.3) | 126 (14.3) | <0.001 |
| Post-intervention follow-up activities | |||
| LDL-cholesterol determination in patients in secondary prevention or under lipid-lowering treatment | 204 (15.9) | 128 (16.3) | 0.836 |
| Men | Non-user N=22,256 | User N=13,161 | p-Value |
|---|---|---|---|
| Pre intervention–post intervention | |||
| New diagnoses of hypercholesterolemia, n (%) | 4440 (10.3) | 2627 (10.0) | 0.321 |
| New treatments for hypercholesterolemia in patients with coronary risk ≥10%, n (%) | 320 (0.8) | 345 (1.4) | <0.001 |
| Control of hypercholesterolemia in primary prevention (treated patients), n (%) | 1292 (2.5) | 1288 (4.4) | <0.001 |
| Control of hypercholesterolemia in secondary prevention, n (%) | 329 (8.5) | 366 (16.2) | <0.001 |
| Post-intervention follow-up activities | |||
| LDL-cholesterol determination in patients in secondary prevention or under lipid-lowering treatment | 567 (17.7) | 373 (16.3) | 0.191 |
GP, general practitioner.
We did not observe any remarkable differences in the registry of coronary risk, diabetes risk and proteinuria, but on the registry of cardiovascular secondary prevention (1.5 and 4.7 percentage point difference in women and in men, respectively), where we observed almost the same prevalence of coronary heart disease as at baseline (Supplementary Table 2).
DiscussionThis study shows that patients attended by eCPG users had better control and follow-up of cardiovascular risk factors than those attended by eCPG non-users. The frequent use of eCPG for HTN monitoring has substantially improved BP follow-up and control in all patients, particularly those in secondary prevention. The eCPG for HCOL also improved control of cholesterol levels, which were also improved in secondary prevention. In diabetic patients, we did not observe changes in control after 1-year of follow-up, although we did observe an improvement in the number of control analyses, electrocardiography and fundus performed. Thus, eCPG is useful for reminding the physician of and promoting relevant actions for the follow-up of these cardiovascular risk factors.
Use of CPGThe users group only captured 5% of all GPs in the ICS, indicating the low rate of use of this type of decision support tool. These low rates are consistent with the results of previous studies,5,7,9,13 and may be due to various factors: health professionals’ access to the eCPG decision support environment is voluntary; health professionals often resist change; there is broad knowledge of management strategies for the diseases selected for this study (HTN, T2DM and HCOL), due to their high prevalence,7,8,13,19 such that most GPs did not feel a need to use this system to manage these diseases.
Despite the low rate of use, eCPG are particularly useful for the management, control and follow-up of multimorbid patients. It seems likely that the integration of interactive alerts regarding poor control and/or follow-up on a screen containing details of all of the patient's pathologies would be key to obtaining the best results in patients attended by eCPG users. Previously, Niès et al. concluded that automatic alerts were more effective than decision support systems,19 possibly because they require voluntary activation and are not widely known; these observations are consistent with our results regarding treatment and diagnosis. Certainly, we did not find significant differences between eCPG users and nonusers. Our results agree with other studies that have shown that eCPG are useful for improving patient follow-up but have lower short-term impact on clinical variables.12,20–24 Our study complies with the quality requirements for eCPG described by Roshanov et al.: the system should be integrated into medical records, should obtain data directly from these medical records, should be tested in a pilot study, and eCPG users should receive training on how to use the system. Indeed, in our study more than half of the variables measured showed significant improvements in eCPG users than in nonusers.
Impact of eCPGThe results of this study suggest that the main added value of eCPG is the use of a pop-up alert system to highlight poor control, lack of proper follow-up, and a comprehensive approach to multimorbid patients.
Regarding treatment, the limited impact of eCPG may be due to the already broad knowledge that GPs have about the pathologies and risk factors studied. Regarding our results, there is room for improvement in the use of eCPGs whenever these tools are integrated into a single work and registry environment, with automatic pop-up alerts that are easily identifiable and limited to relevant issues, and are delivered via easy-to-use, intuitive support systems. Key elements to increase the use of these tools include the GP scheme used to incentivise GPs, pending activities reminders, feed-back on GPs’ actions, continuous updating of contents, and GP ongoing training for GPs.3,10,14,25
eCPGs facilitate a comprehensive approach to patients. Multimorbid patients in secondary prevention achieve better control and follow-up, which likely improves long-term outcomes. However, longer follow-up would be required to ascertain the true long-term impact.
Characteristics and limitationsThis study has been conducted under real clinical practice conditions, which increases its external validity, although caution is needed before generalizing the results. Since we have focussed on eCPG users and nonusers, the majority of professionals have not been included in this study. Nonetheless, the large sample size analyzed and the strategy used for participant selection increases the study's representativeness in terms of the population attended in primary health care settings.18
Our study has various limitations. First, the quasi-experimental design means that we cannot definitively attribute the observed differences to the implementation of eCPGs. The GPs that decided to use the eCPGs were likely different to those who did not use these tools, although there were minimal differences between the two cohorts before implementation of the eCPG. Unfortunately, we did not have data regarding GPs characteristics of each group (e.g. users and non-users). Second, the ICS has developed a progressive incentive scheme for professionals, and also offers feedback systems to improve assistance and pharmaceutical quality. These recommendations, which include the pathologies analyzed in this study, may have minimized the impact of the eCPG. Finally, a longer follow-up period would be required to evaluate the true impact on health outcomes.
We conclude that eCPGs are an effective tool for controlling and conducting follow-up on patients diagnosed with HTN, T2DM and HCOL. The utility of eCPG to adequately diagnose and treat individuals with these pathologies is still unclear.
Funding supportThis project was supported by a grant from the Agència d’Informació, Avaluació i Qualitat en Salut (grant number: 483/13/2009). Dr. Grau was funded by grants from Health Institute Carlos III-FEDER, Spain (Miguel Servet CP12/03287).
Clinical practice guidelines can facilitate decision-making based on the best available evidence and can decrease unjustified variability in clinical practice.
A strategy that may help to increase the application of clinical practice guidelines in primary care is to integrate these tools into health providers’ electronic medical records
What does this study adds?Patients attended by electronic clinical practice guidelines users had better control and follow-up of cardiovascular risk factors than those attended by eCPG non-users.
Electronic clinical practice guidelines are useful for reminding the physician of and promoting relevant actions for the follow-up of these cardiovascular risk factors.
None declared.
Members of the @GPC-ICS Group: Ester Amado, Arantxa Catalán-Ramos, Ramon Ciurana, Eva Comin, Alicia Consola, Xavier Cos, Josep Davins, Alicia Franzi, Eva Frigola, María Grau, Manuel Iglesias-Rodal, Manel Mata, Angels Pons, José Luis del Val García, Jose Mª Verdu.
We appreciate the revision of the English text by Gavin Lucas.