To determine the prevalence of insomnia in a sample of Portuguese adolescents and assess its repercussions on HRQoL, daytime sleepiness and depressive symptomatology.
DesignWe carried out a cross-sectional school-based study evaluating students from Viseu.
LocationStudents from twenty-six public secondary schools in the county of Viseu, Portugal.
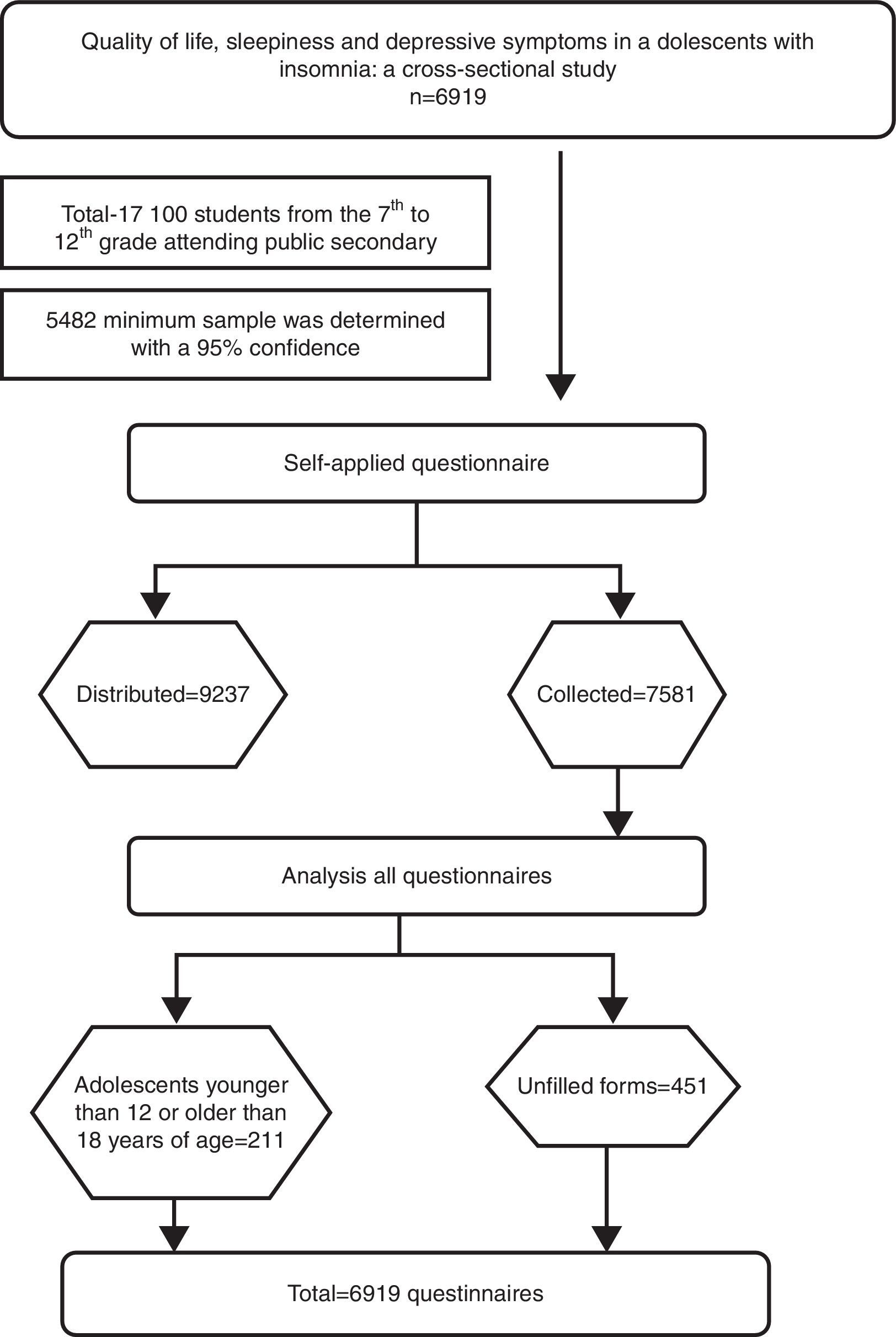
ParticipantsOf 9237 questionnaires distributed, 7581 were collected (82.1%). We excluded from analysis all questionnaires from adolescents younger than 12 or older than 18 years of age (211) and unfilled forms (451). The sample comprised 6919 adolescents, the 7th to 12th grade, from 26 public secondary schools.
InterventionsNone.
MeasurementsData gathering was done using a self-applied questionnaire. Insomnia was defined based on the Diagnostic and Statistical Manual of Mental Disorders – IV criteria. HRQoL was evaluated with the Quality of Life Health Survey SF-36, depressive symptomatology with BDI-II and daytime sleepiness with the Epworth Sleepiness Scale.
ResultsPrevalence of insomnia was 8.3% and the prevalence of adolescents with symptoms of insomnia without daytime impairment (disturbed sleepers) was 13.1%. HRQoL was significantly reduced among adolescents with insomnia compared to normal sleepers (p<0.001) and even when compared to disturbed sleepers (p<0.001). There was an increase in daytime sleepiness from normal sleepers to disturbed sleepers and to adolescents with insomnia (p<0.001). There was also an increase in the prevalence and severity of depressive symptoms (p<0.001).
ConclusionsOur results show that insomnia is associated with a significantly lower health related quality of life among adolescents.
Determinar prevalencia de insomnio en una muestra de adolescentes portugueses y evaluar sus repercusiones en la calidad de vida relacionada con la salud (CVRS), somnolencia diurna y sintomatología depresiva.
DiseñoEstudio transversal evaluar a los estudiantes de Viseu.
EmplazamientoEstudiantes de 26 escuelas secundarias públicas en condado de Viseu, Portugal.
ParticipantesDe 9.237 cuestionarios distribuidos, se recogieron 7.581 (82,1%). Se excluyeron del análisis todos los cuestionarios de adolescentes menores de 12 o mayores de 18 años de edad (211) y las formas sin relleno (451). La muestra fue de 6.919 adolescentes, del 7.° al 12.° grado, de 26 escuelas secundarias públicas.
IntervencionesNo se aplicó ninguna intervención.
MedicionesLa recolección de datos se realizó mediante un cuestionario autoaplicado. El insomnio se define sobre la base de los criterios del Manual diagnóstico y estadístico de los trastornos mentales, cuarta edición. La CVRS se evaluó con la calidad de vida de la Encuesta de Salud (SF-36), la sintomatología depresiva con BDI-II y la somnolencia durante el día con Epworth.
ResultadosLa prevalencia de insomnio fue del 8,3% y de síntomas de insomnio sin deterioro durante el día (durmientes perturbados) fue del 13,1%. La CVRS se redujo significativamente entre los adolescentes con insomnio en comparación con los durmientes normales (p<0,001) e incluso cuando se compara con durmientes perturbados (p<0,001). Hay un aumento en la somnolencia diurna de durmientes normales comparados con los durmientes perturbados y los adolescentes con insomnio (p<0,001). También hubo un aumento en la prevalencia y la gravedad de los síntomas depresivos (p<0,001).
ConclusionesNuestros resultados muestran que el insomnio se asocia a una CVRS significativamente más baja entre los adolescentes.
Insomnia is well known as the major sleep disorder among adolescents1,2 and its consequences have been shown to affect several aspects of adolescents’ health and daily performance.2,3 Moreover, behavioral patterns established during adolescence have the potential to affect the development of adulthood lifestyles.4,5
Several studies have exposed the link between insomnia and physical repercussions ranging from lack of energy and fatigue, to headache, abdominal and back pain, obesity and poor health in general.2,6–8 The behavioral, emotional and psychiatric burden of insomnia is perhaps even more unmistakable, with a rising body of evidence associating insomnia to depression, anxiety, suicidal thoughts and attempts, poor academic performance, poor perceived health and substance abuse.2,9–12 Daytime sleepiness is a more ambiguous consequence of insomnia. Nevertheless, it has been shown to be increased in adolescents with disturbed sleep and to result in poorer humor and diminished functioning in daily activities and learning.13–15
There is still little research on the influence of insomnia in adolescent's Health Related Quality of Life (HRQoL) and results are inconsistent. Palermo et al.16 found that increased insomnia symptoms were associated with poorer HRQoL outcomes. Roberts et al.10 found no effect of insomnia on somatic and psychological functioning (perceived health, health limitation and impact of illness; perceived mental health and life satisfaction) whereas the same author Roberts et al.8 reported that insomnia increased the risk of poor somatic and psychological functioning. One study explored this issue in an older population (a sample of college students, mean age 20.39 years) and concluded that students with chronic insomnia had lower quality of life.5 Furthermore, the theoretical pathways linking insomnia and HRQoL need clarification. A negative relationship between adolescents’ sleep patterns (eveningness) and HRQoL has been found17,18 and it is proposed that insomnia symptoms may be the mediating factors in this relationship.18 Another possible association between insomnia and HRQoL may be the direct result of sleep deprivation.15
In adolescents, the longitudinal studies performed so far indicate that insomnia may have a high rate of persistency.8,12,19 HRQoL is understood to “encompass those aspects of overall quality of life that can be clearly shown to affect health either physical or mental”20 and the advances in HRQoL research have played a significant contribution to the improvement in other areas of medicine.
We hypothesize that insomnia is negatively associated with adolescents’ HRQoL in a significant way and that the impairment in HRQoL is parallel to its association with depressive symptoms and daytime sleepiness. Thus, the aim of this study was to determine the prevalence of insomnia in a sample of Portuguese adolescents and to assess its repercussions on HRQoL, daytime sleepiness and depressive symptomatology.
MethodsIn a cross-sectional study that took place during the year 2013 in the county of Viseu, Portugal, we evaluated a sample composed of students from 26 public secondary schools, chosen using convenience and random criteria (one school with 7th to 12th grade students per each township; in 2 townships there were no schools with 7th to 12th grade students and two schools were chosen – one with 7th to 9th grade students and another with 10th to 12th grade students). All students attending the 7th to 12th grade in the 26 schools were included. This sample was designed to be representative of the county's adolescent population, with students of both genders aged 12–18, from rural and urban settings. There was a total of 17,100 students from the 7th to 12th grade attending public secondary schools and considering an estimate proportion of 8% of adolescents with insomnia and 30% of adolescents with insufficient sleep and a 1% error margin a 5482 minimum sample was determined with a 95% confidence. The Ethics Committee of our institution approved the data-gathering tool, as did the appropriate governmental review board and the directive and pedagogic assemblies of each school. Of 9237 questionnaires distributed, 7581 were collected (82.1%). We excluded from analysis all questionnaires from adolescents younger than 12 or older than 18 years of age (211) and unfilled forms (451). Data from a total of 6919 questionnaires were analyzed. Study design (Fig. 1) by self-administered questionnaire answered in the classroom.
The questionnaire was composed of a brief introduction, explaining the purpose of the study and asking for the student's cooperation, followed by sets of questions aiming at socio-demographic characterization, evaluation of insomnia, health related quality of life, daytime sleepiness and depressive symptoms.
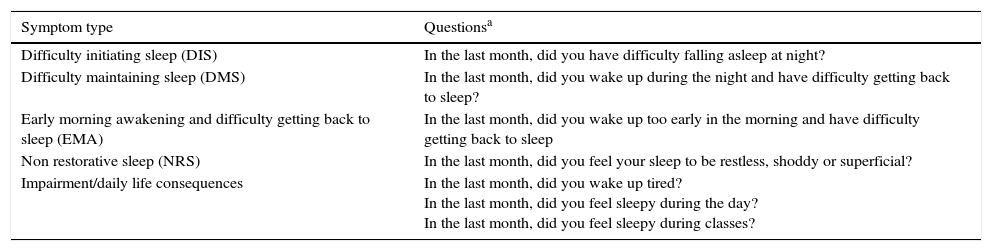
Insomnia was assessed based on the presence of insomnia symptoms as defined by the DSM-IV criteria symptoms associated with daytime impairment, in the previous month and with a frequency of at least three times per week. The questions used to evaluate insomnia symptoms and daytime impairment is shown in Table 1.
Questions used to assess the presence of insomnia.
| Symptom type | Questionsa |
|---|---|
| Difficulty initiating sleep (DIS) | In the last month, did you have difficulty falling asleep at night? |
| Difficulty maintaining sleep (DMS) | In the last month, did you wake up during the night and have difficulty getting back to sleep? |
| Early morning awakening and difficulty getting back to sleep (EMA) | In the last month, did you wake up too early in the morning and have difficulty getting back to sleep |
| Non restorative sleep (NRS) | In the last month, did you feel your sleep to be restless, shoddy or superficial? |
| Impairment/daily life consequences | In the last month, did you wake up tired? In the last month, did you feel sleepy during the day? In the last month, did you feel sleepy during classes? |
Health related quality of life was evaluated with the Medical Outcomes Study 36-item Short-Form Health Survey (SF-36), validated for the Portuguese population.21 SF-36 is a generic measure composed of two dimensions (physical health and mental health) subdivided into an 8-scale profile with 35 items. Scores range from 0 to 100 with higher scores indicating better health status. Health related quality of life was treated as a continuous variable.
Daytime sleepiness was assessed with the Epworth Sleepiness Scale (ESS).22 Each item is rated on a 4-point Likert-type scale ranging from 0 to 3, and the adolescent is asked to imagine how he/she would be affected by each situation picking the closest option: 0 – would never doze; 1 – slight chance of dozing; 2 – moderate chance of dozing; 3 – high chance of dozing. The classification is as follows: <10 – no sleepiness; 10–15 – light sleepiness; 16–20 – moderate sleepiness; 21–24 – severe sleepiness and was considered the adolescent suffered from sleepiness when presenting a score ≥10. For depressive symptoms we used the Beck Depression Inventory for Adolescents (BDI-II) validated for the Portuguese population.23 Results in each item vary from 0 (low) to 3 (high), and the total score can amount from 0 (minimum) to 63 (maximum). Studies have established 13 as the cutoff value of the following global classification: 0–13, “minimum” depressive symptoms; 14–19, “light”; 20–28, “moderate”; and equal or above 29, “serious or severe” depressive symptoms.24
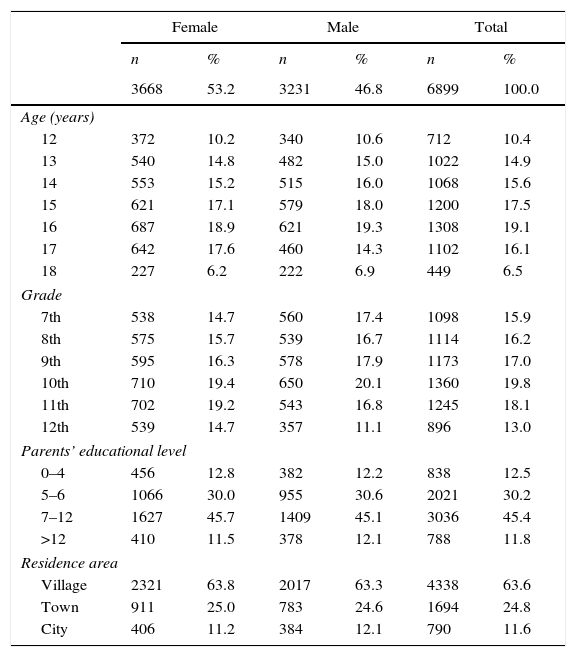
Sample characterizationThe characteristics of the study population are shown in Table 2. The complete sample consisted of 6919 adolescents, of which 3668 (53.2%) were of the female gender. The largest percentage was of 16 years old adolescents (19.1%) and of adolescents attending the tenth grade (19.8%). A total of 45.4% of parents had a 7th to 12th grade education and 63.6% of adolescents lived in a village.
Socio-demographic characteristics of the sample.
| Female | Male | Total | ||||
|---|---|---|---|---|---|---|
| n | % | n | % | n | % | |
| 3668 | 53.2 | 3231 | 46.8 | 6899 | 100.0 | |
| Age (years) | ||||||
| 12 | 372 | 10.2 | 340 | 10.6 | 712 | 10.4 |
| 13 | 540 | 14.8 | 482 | 15.0 | 1022 | 14.9 |
| 14 | 553 | 15.2 | 515 | 16.0 | 1068 | 15.6 |
| 15 | 621 | 17.1 | 579 | 18.0 | 1200 | 17.5 |
| 16 | 687 | 18.9 | 621 | 19.3 | 1308 | 19.1 |
| 17 | 642 | 17.6 | 460 | 14.3 | 1102 | 16.1 |
| 18 | 227 | 6.2 | 222 | 6.9 | 449 | 6.5 |
| Grade | ||||||
| 7th | 538 | 14.7 | 560 | 17.4 | 1098 | 15.9 |
| 8th | 575 | 15.7 | 539 | 16.7 | 1114 | 16.2 |
| 9th | 595 | 16.3 | 578 | 17.9 | 1173 | 17.0 |
| 10th | 710 | 19.4 | 650 | 20.1 | 1360 | 19.8 |
| 11th | 702 | 19.2 | 543 | 16.8 | 1245 | 18.1 |
| 12th | 539 | 14.7 | 357 | 11.1 | 896 | 13.0 |
| Parents’ educational level | ||||||
| 0–4 | 456 | 12.8 | 382 | 12.2 | 838 | 12.5 |
| 5–6 | 1066 | 30.0 | 955 | 30.6 | 2021 | 30.2 |
| 7–12 | 1627 | 45.7 | 1409 | 45.1 | 3036 | 45.4 |
| >12 | 410 | 11.5 | 378 | 12.1 | 788 | 11.8 |
| Residence area | ||||||
| Village | 2321 | 63.8 | 2017 | 63.3 | 4338 | 63.6 |
| Town | 911 | 25.0 | 783 | 24.6 | 1694 | 24.8 |
| City | 406 | 11.2 | 384 | 12.1 | 790 | 11.6 |
The analysis and processing of data were done using the Statistical Package for the Social Sciences version 21 (SPSS 21). Continuous variables were described by measures of central tendency (mean) and dispersion (standard deviation). Mann–Witney and Kruskal–Wallis tests were used to compare the distribution of continuous variables, regardless of the nature of distribution. The Chi-square test was used to compare proportions, with a 5% level of significance. The magnitude of the association between variables and insomnia was estimated through Odds ratio (OR) with the respective 95% confidence interval (CI).
ResultsIn the total sample, the prevalence of insomnia according to DSM-IV criteria was 8.3%. Another 13.1% of adolescents presented symptoms of insomnia but did not meet the daytime impairment criterion for insomnia. The remaining 78.6% of adolescents had no symptoms of insomnia. Thus, we divided our population into 3 groups: adolescents with insomnia – 8.3%; disturbed sleepers (adolescents with symptoms of insomnia but without daytime impairment) – 13.1%; and normal sleepers – 78.6%. Both insomnia and disturbed sleep were higher in the female gender (10.1% versus 5.9% and 25.6% versus 15.8%, respectively, p<0.01).
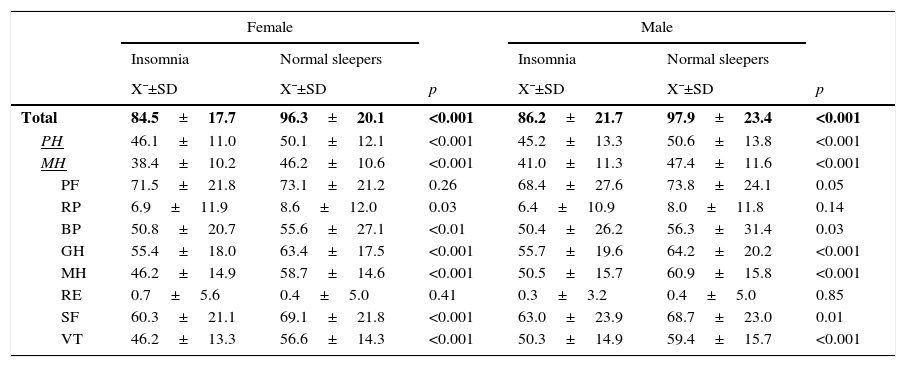
HRQoL was significantly lower among adolescents with insomnia (85.0±19.0 vs. 97.1±21.6, p<0.001), both girls and boys (84.5±17.7 vs. 96.3±20, p<0.001 and 86.2±21.7 vs. 97.9±23.4, p<0.001, respectively). Table 3 shows the differences in HRQoL between adolescents with insomnia and normal sleepers. For girls there was a statistically significant reduction in quality of life in all measures except “physical functioning” and “role-emotional”. For boys there was a statistically significant reduction in quality of life in all measures except “role-physical” and “role-emotional”.
Health related quality of life (SF-36) and insomnia.
| Female | Male | |||||
|---|---|---|---|---|---|---|
| Insomnia | Normal sleepers | Insomnia | Normal sleepers | |||
| X¯±SD | X¯±SD | p | X¯±SD | X¯±SD | p | |
| Total | 84.5±17.7 | 96.3±20.1 | <0.001 | 86.2±21.7 | 97.9±23.4 | <0.001 |
| PH | 46.1±11.0 | 50.1±12.1 | <0.001 | 45.2±13.3 | 50.6±13.8 | <0.001 |
| MH | 38.4±10.2 | 46.2±10.6 | <0.001 | 41.0±11.3 | 47.4±11.6 | <0.001 |
| PF | 71.5±21.8 | 73.1±21.2 | 0.26 | 68.4±27.6 | 73.8±24.1 | 0.05 |
| RP | 6.9±11.9 | 8.6±12.0 | 0.03 | 6.4±10.9 | 8.0±11.8 | 0.14 |
| BP | 50.8±20.7 | 55.6±27.1 | <0.01 | 50.4±26.2 | 56.3±31.4 | 0.03 |
| GH | 55.4±18.0 | 63.4±17.5 | <0.001 | 55.7±19.6 | 64.2±20.2 | <0.001 |
| MH | 46.2±14.9 | 58.7±14.6 | <0.001 | 50.5±15.7 | 60.9±15.8 | <0.001 |
| RE | 0.7±5.6 | 0.4±5.0 | 0.41 | 0.3±3.2 | 0.4±5.0 | 0.85 |
| SF | 60.3±21.1 | 69.1±21.8 | <0.001 | 63.0±23.9 | 68.7±23.0 | 0.01 |
| VT | 46.2±13.3 | 56.6±14.3 | <0.001 | 50.3±14.9 | 59.4±15.7 | <0.001 |
Note: PH, Physical Health component; MH, Mental Health component; PF, physical functioning; RP, role-physical (role limitations due to physical problems); BP, bodily pain; GH, general health; MH, mental health; RE, role-emotional (role limitations due to emotional problems); SF, social functioning; VT, Vitality.
When comparing adolescents with insomnia to disturbed sleepers, HRQoL was significantly reduced in adolescents with insomnia (85.0±19.0 vs. 93.2±19.6, p<0.001). And when comparing disturbed sleepers to normal sleepers, HRQoL was inferior for adolescents with disturbed sleep (93.2±19.6 vs. 97.7±21.9, p<0.001).
Most of the adolescents (76.7%) stated having no illnesses. The remaining 23.3% reported comorbid conditions, ranging from asthma (9%) to lactose intolerance (1 adolescent). No other sleep disorder was reported as comorbidity. When students with comorbid conditions were excluded from analysis, there was still a statistically significant reduction in HRQoL in adolescents with insomnia, both girls (86.6±17.0 vs. 97.7±20.2, p<0.001) and boys (90.0±20.5 vs. 97.6±24.0, p<0.01).
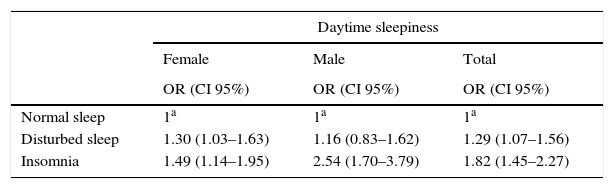
The prevalence of daytime sleepiness in the total sample was 33.1% and the mean ESS score was 7.69. Daytime sleepiness was more prevalent in girls (36.6% vs. 29.1%, p<0.001). There was a statistically significant reduction in the prevalence of daytime sleepiness from adolescents with insomnia to disturbed sleepers and to normal sleepers (47.1% vs. 38.8% vs. 32.9%, p<0.001). Table 4 shows the differences in risk of daytime sleepiness between the 3 groups.
The prevalence of depressive symptoms in our population was 20.9% and the risk of presenting depressive symptoms was higher among girls (OR=1.96; CI95%: 1.73–2.23). All severity scores of depressive symptomatology were more prevalent in female adolescents (p<0.001).
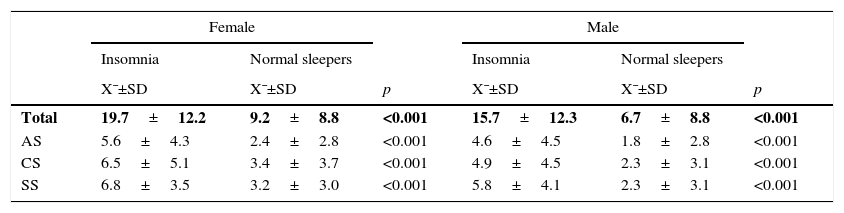
There was a statistically significant decrease in the prevalence of depressive symptoms from adolescents with insomnia to disturbed sleepers and to normal sleepers (65.6% vs. 36.9% vs. 18.6%, p<0.001) and adolescents with insomnia presented more severe depressive symptoms than did the other two groups (18.53±12.34 vs. 12.31±10.72 vs. 7.43±8.41, p<0.001). Insomnia represented a much higher risk of suffering from depressive symptoms (OR=7.11; CI95%: 5.56–9.11) when compared to disturbed sleep (OR=2.47; CI95%: 2.02–3.02).
Mean scores for all dimensions of BDI-II (affective, cognitive and somatic depressive symptoms) were higher in adolescents with insomnia of both genders. Table 5 shows the differences in depressive symptoms between adolescents with insomnia and normal sleepers.
Depressive symptoms (BDI-II) and insomnia.
| Female | Male | |||||
|---|---|---|---|---|---|---|
| Insomnia | Normal sleepers | Insomnia | Normal sleepers | |||
| X¯±SD | X¯±SD | p | X¯±SD | X¯±SD | p | |
| Total | 19.7±12.2 | 9.2±8.8 | <0.001 | 15.7±12.3 | 6.7±8.8 | <0.001 |
| AS | 5.6±4.3 | 2.4±2.8 | <0.001 | 4.6±4.5 | 1.8±2.8 | <0.001 |
| CS | 6.5±5.1 | 3.4±3.7 | <0.001 | 4.9±4.5 | 2.3±3.1 | <0.001 |
| SS | 6.8±3.5 | 3.2±3.0 | <0.001 | 5.8±4.1 | 2.3±3.1 | <0.001 |
Note: AS, affective symptoms; CS, cognitive symptoms; SS, somatic symptoms.
As hypothesized, insomnia was associated with decreased HRQoL and increased daytime sleepiness and depressive symptoms among adolescents.
In fact our results show a clear association between insomnia in adolescents and a poorer HRQoL, and there was a well defined continuous of reduced HRQoL from normal sleepers to disturbed sleepers and to adolescents with insomnia. Despite conflicting results10 this finding is concordant with previous investigations in adolescents and young adults with sleep disorders.5,15,16 However, comparisons must be made with caution as these different studies address different sleep disorders (insomnia, insomnia symptoms, sleep deprivation) and use different instruments of measurement for quality of life.
However, after exclusion of students with comorbidity from analysis, there was still a significant reduction in HRQoL among adolescents with insomnia, corroborating the association of insomnia to worse HRQoL. Insomnia may potentially influence quality of life in many ways (direct effect of sleep deprivation, fatigue, daytime sleepiness, depressive symptoms, substance abuse). Daytime sleepiness and depressive symptoms may be important mediators in this relationship. In our investigation female adolescents presented a greater reduction in HRQoL and they also presented more daytime sleepiness and depressive symptoms. More studies will be necessary to highlight the pathways linking insomnia to quality of live and to understand if daytime sleepiness and depressive symptoms are surrogate markers of quality of live among adolescents with insomnia.
Health related quality of life has been researched mainly on chronic diseases. The publication of DSM 5 has established a definition for chronic insomnia and on the before mentioned study on college students it was found that the chronic insomnia group had lower quality of life.5 The DSM-IV criteria we used do not include such a definition and our assessment of insomnia does not allow us to know if symptoms lasted for more than one month. Nevertheless, the existing evidence suggests that insomnia among adolescents is a chronic condition.8,12,19
In respect to daytime sleepiness, though our findings showed a high prevalence (33.1%) it is still bellow that reported by studies with comparable populations.14,25,26 This difference may arise from different socio-demographic backgrounds especially the fact that other investigations include adolescents of predominantly urban areas whereas only 36.4% of our study population lived in urban settings. Yet, there was a continuous increase in the prevalence of daytime sleepiness from normal sleepers to disturbed sleepers and to adolescents with insomnia and these outcomes strengthen the conclusions of other investigations correlating daytime sleepiness with insomnia among adolescents.14,26
Our results also reinforce the findings in the literature on depressive symptoms and depression as consequences of insomnia in adolescents.27–29 Overall, as for HRQoL and daytime sleepiness, the prevalence, severity, and risk for depressive symptoms increased from normal sleepers to disturbed sleepers and from these to adolescents with insomnia.
Until now, the repercussions of insomnia in adolescents have mainly been considered in its somatic and psychosocial features. Our investigation shows an association of insomnia to a lower quality of life and this is an important finding. It has been suggested, concerning childhood sleeping patterns and behavioral patterns established during adolescence, that there might be knock on effects throughout life.4,5,30 Thus, adolescents with insomnia present a higher risk of becoming adults with sleep disorders and experience an enduringly reduced quality of life.
Our findings add to the comprehensive knowledge of the consequences of insomnia and the evidence that insomnia is negatively associated with adolescents HRQoL is a contribution to highlight the importance of insomnia among adolescents as a public health issue. Health promoting strategies must be undertaken to allow adolescents with insomnia and their families to obtain the necessary assistance as soon as possible. We suggest that daytime sleepiness and depressive symptoms may be remarkably important warning signs among adolescents with insomnia as they may predict an impact on HRQoL.
This study has some limitations. As a cross-sectional study it does not allow to establish a causality link between insomnia and the studied variables. However, most of the available data on insomnia among adolescents comes from cross-sectional studies such as this and the use of rigorous diagnostic criteria resulted on a prevalence of insomnia in our population (8.3%) concordant with the findings of other epidemiological studies.29 Prevalence of adolescents with symptoms of insomnia, with or without daytime impairment (21.4%) is also within the values revealed in other investigations. Another limitation is the fact that all information is based on self-reported symptoms among adolescents. This may result in information biases, namely memory bias and socially desirable answer bias. However, given the difficulty in obtaining objective data about sleep, epidemiological studies in this area have always used indirect methods to assess sleep. Yet another limitation is the fact that our exploration for impairment included only daytime fatigue and sleepiness. Using a broader array of assessment for daytime impairment (especially academic performance and social functioning) could be desirable but would probably result in the consideration of indicators that are not specific to sleep.
Sleep disorders, essentially insomnia, are increasingly prevalent among adolescents and the insomnia is a clear public health issue among adolescents. There are few investigations on insomnia, daytime sleepiness, quality of life and depressive symptoms among Portuguese adolescents. The impact of insomnia on adolescent's health related quality of life and the theoretical pathways linking insomnia to quality of life were largely unknown.
What we get out the study?This study allowed for a situation diagnosis about insomnia and the daytime sleepiness, quality of life, depressive symptoms among Portuguese adolescents. Insomnia is associated to a significant reduction of adolescents health related quality. Daytime sleepiness and depressive symptoms may be the link between insomnia and health related quality of life. As the leading sleep disorder among adolescents and due to its association with worse quality of life, insomnia is a clear public health issue among adolescents.
The authors declare that they have no competing interests.