The aim of this paper was to analyse the association of demographic, clinical and pharmacological risk factors with the presence of SARS-COV-2 virus infection, as well as to know the variables related to mortality from COVID-19 in nursing home (NH) residents.
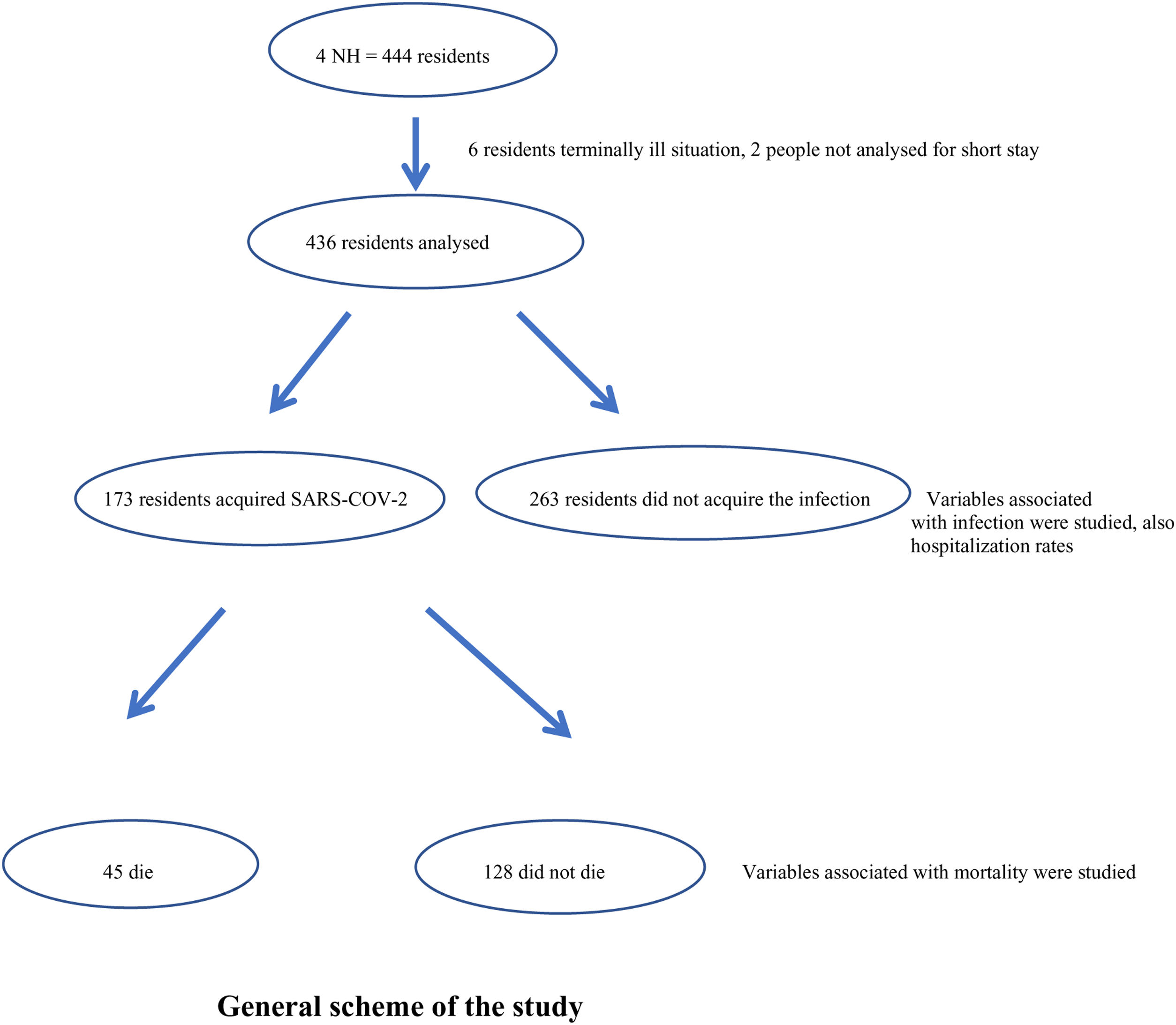
DesignRetrospective case–control study. The study variables of those residents who acquired the infection (case) were compared with those of the residents who did not acquire it (control). A subgroup analysis was carried out to study those variables related to mortality.
SiteNursing homes in the region of Guipúzcoa (Spain).
Participants and interventions4 NHs with outbreaks of SARS-CoV-2 between March and December 2020 participated in the study. The infectivity and, secondary, mortality was studied, as well as demographic, clinical and pharmacological variables associated with them. Data were collected from the computerised clinical records.
Main measurementsInfection and mortality rate. Risk factors associated with infection and mortality.
Results436 residents were studied (median age 87 years (IQR 11)), 173 acquired SARS-CoV-2 (39.7%). People with dementia and Global Deterioration Scale ≥6 were less likely to be infected by SARS-CoV-2 virus [OR=0.65 (95% CI 0.43–0.97; p<.05)]. Overall case fatality rate was 10.3% (a mortality of 26% among those who acquired the infection). COVID-19 mortality was significantly associated with a Global Deterioration Scale ≥6 (OR=4.9 (95% CI 1.5–16.1)), COPD diagnosis (OR=7.8 (95% CI 1.9–31.3)) and antipsychotic use (OR=3.1 (95% CI 1.0–9.0)).
ConclusionsAdvanced dementia has been associated with less risk of SARS-CoV-2 infection but higher risk of COVID-19 mortality. COPD and chronic use of antipsychotics have also been associated with mortality. These results highlight the importance of determining the stage of diseases such as dementia as well as maintaining some caution in the use of some drugs such as antipsychotics.
El objetivo de este trabajo fue analizar la asociación de factores de riesgo demográficos, clínicos y farmacológicos con la presencia de infección por virus SARS-CoV-2, así como conocer las variables relacionadas con la mortalidad por COVID-19 en residentes institucionalizados en centros residenciales.
DiseñoCasos y controles retrospectivo. Se compararon las variables de estudio de aquellos residentes que adquirieron la infección (caso) con las de los residentes que no la adquirieron (control). Se realizó un análisis de subgrupos para conocer aquellas variables relacionadas con la mortalidad.
EmplazamientoCentros residenciales de la provincia de Guipúzcoa (España).
Participantes e intervencionesCuatro centros residenciales con brotes de SARS-CoV-2, entre marzo y diciembre del 2020. Se estudiaron la infectividad y, de manera secundaria, la mortalidad, así como variables demográficas, clínicas y farmacológicas asociadas con las mismas. Los datos fueron recogidos de las historias clínicas informatizadas.
Mediciones principalesTasa de infección y mortalidad. Factores de riesgo asociados a la infección y a la mortalidad.
ResultadosSe estudió a 436 residentes (mediana de edad 87 años [RIC 11]), 173 de ellos adquirieron la infección (39,7%). Los residentes con demencia y un índice en la Global Deterioration Scale ≥6 tuvieron menor probabilidad de infectarse por el virus SARS-CoV-2 (OR=0,65 [IC del 95%, 0,43-0,97; p<0,05]). La tasa de mortalidad global fue del 10,3% (del 26% entre aquellos que adquirieron la infección). La mortalidad por COVID-19 se asoció de manera significativa con un índice Global Deterioration Scale ≥6 (OR=4,9 [IC del 95%, 1,5-16,1]), tener un diagnóstico de EPOC (OR=7,8 [IC del 95%, CI 1,9-31,3]) y con el uso de antipsicóticos (OR=3,1 [IC del 95%, CI 1,0-9,0]).
ConclusionesLa demencia avanzada se asoció con menor riesgo de infección y mayor de mortalidad por COVID-19. La EPOC y el uso crónico de neurolépticos se asociaron también con la mortalidad por esta enfermedad. Estos resultados ponen de manifiesto la importancia de determinar la fase evolutiva en enfermedades como la demencia, así como mantener cierta precaución en el uso de medicamentos como los antipsicóticos.
SARS-CoV-2 virus is the cause of COVID-19 disease; the first cases were diagnosed in Wuhan (China) around December 2019. Some weeks later it was already a world-wide pandemic.1,2
SARS-CoV-2 shows a broad spectrum of disease presentation, from asymptomatic infection to respiratory failure with high mortality.3 Most patients affected by SARS-CoV-2 present a pseudo-influenza-like illness with mild symptoms such as fever, cough and some degree of dyspnoea. However, a small percentage of patients develop pneumonia which, in some cases, leads to respiratory distress syndrome, septic shock, metabolic acidosis and coagulopathy.4 Some studies indicate that coagulation dysfunction is the main cause of death in patients with severe COVID-19.1,5
This pandemic has led to a major crisis in nursing homes (NH). The combination of a vulnerable population living in the same facility with non-specific and atypical COVID-19 presentations, coupled with a shortage of rapid diagnostic tests and personal protective equipment, have complicated disease management.2 This fact has led some researchers to study the impact for infection and mortality as well as those risk factors associated with a worse evolution.
A cohort study conducted in 15,038 US NHs from April to September 2020 showed an infectivity of 28.4% and a mortality of 19.2%. Risk of infection increased with increasing body mass index (BMI) (adjusted hazard ratio 1.19; 95% CI 1.15–1.24), but varied little by other residents characteristics.6 However, the study of Shi et al. found that male sex, bowel incontinence and staff residence in a community with a high burden of SARS-CoV-2 infection were predictors of that infection.7
On the other side, a health database analysis3 looked at predisposing factors for hospitalisation and mortality from COVID-19 in people over 65 years of age. Type II diabetes mellitus (T2DM), dementia, chronic obstructive pulmonary disease (COPD), pneumonia, depression, atrial fibrillation and arterial hypertension (AHT) were independent predictors of COVID-19 hospitalisation, the first 5 remaining statistically significant for related mortality. Some authors found that frailty was a better predictor of negative health outcomes than age or co-morbidity.8 The impact of obesity on severe COVID-19 has also been highlighted given the increased thrombotic risk and by being frequently associated with other co-morbidities.9
Another study investigated the possible relationship between severe COVID-19 and prior pharmacological treatment.10 The results associate severe COVID-19 with polypharmacy and drugs that cause sedation, respiratory depression or dyskinesia and drugs with anticholinergic effects. The drugs with the largest effects were antipsychotics (rate ratio 4.18 (95% CI 3.42–5.11)).
It is important to improve knowledge of COVID-19 risk factors and its impact in NHs to design strategies for the management of the disease. For this reason, the aim of this paper was to analyse the association of demographic, clinical and pharmacological risk factors with the presence of SARS-COV-2 virus infection, as well as to know the variables related to mortality from COVID-19 in nursing home (NH) residents.
Materials and methodsDesignRetrospective case–control study in old people living in some NHs affected by SARS-CoV-2 outbreaks between March and December 2020 in the region of Guipúzcoa (Basque Country, Spain).
The four NHs included in the study belong to a non-profit foundation that manages 7 NHs. They all have their own physician with standardised social and health care, although variable in size (capacity from 78 to 145 residents). 4 centres, those with positive cases, were included.
Study sampleAccepting an α risk of 0.05 and a β risk of <0.2, it takes a minimum of 74 cases and 74 controls to detect a minimum odds ratio of 2.5. It is assumed that the exposure rate in the control group will be 0.5. A loss to follow-up rate of 0% has been estimated. The poison approximation has been used.
Analysis strategyThe main analysis was carried out with those residents that acquire the infection (case) in the population of the 4 centres (no infection=control). A subgroup analysis was carried out of those who acquired the infection and died (case) compared to those who acquired the infection and did not die (control). Mortality not related to COVID-19 was not analysed in the search for relationships. SARS-CoV-2 cases were confirmed by polymerase chain reaction (PCR).
SubjectsThis study included all residents that lived in NHs that had at least one positive case (outbreak) of SARS-CoV-2. Terminally ill residents at the time of the first SARS-CoV-2 positive diagnosis were excluded from the study, also those with less than one month stay in the NH.
Study variables (data collection)Socio-demographic, clinical and pharmacotherapeutic data were collected from the computerised clinical records of the Basque Health Service (Osakidetza) and the computerised records of the NHs. Data on gender, age, BMI, main co-morbidities (AHT, T2DM, COPD, dementia) were recorded. Likewise, less than one-year-old data from the different scales from the last comprehensive geriatric assessment were collected, which measured functionality (Barthel Index),11 cognitive status (Global Deterioration Scale – GDS)12 and frailty index (Frail-VIG index – based on a comprehensive geriatric assessment).13 With regard to pharmacotherapeutic treatment, data were obtained on the number of drugs received by residents 10 days before the first detected case of SARS-CoV2 in each NH (measured as the number of prescription lines), as well as whether they were receiving anticoagulant, antiplatelet and/or psychotropics. In those that registered SARS-CoV2 infection, data associated with infection, symptomatology, patient referral and death by COVID-19 were collected.
Ethical considerationsThe study was approved for execution by the local Research Ethics Committee with acceptance of waiver of informed consent request. Residents’ identification data were anonymised in the database.
Statistical analysisThe descriptive analysis of the variables was expressed as mean (SD), median (IQR) or frequency (%). Pearson's χ2 test was used for comparison in the case of qualitative variables. Student's t-test and Mann–Whitney U test were used for comparisons in parametric and non parametric distributions, respectively.
We conducted two conditional logistic regression analyses to determine crude and adjusted odds ratios (ORs) with 95% confidence intervals (CI): the main for SARS-CoV-2 infection as a dependent variable and a subgroup analysis with SARS-CoV-2 positive cases for the COVID-19 mortality as a dependent variable. For the final analysis of the multivariate model, the Wald backward elimination technique was used to determine the adjusted OR and 95% CI. In that model all variables that showed a p value <0.1 in univariate analyses were included. Goodness-of-fit of the model was established using Nagelkerke's R2 as well as the Hosmer–Lemeshow test. All analyses were performed using SPSS software (SPSS Inc, Chicago, IL version 20.0). A p<0.05 was considered statistically significant.
ResultsThe study variables of the 436 residents of the four NHs were studied. 6 residents were excluded because of terminally ill situation and 2 because of short stay. Demographic data, scales from geriatric assessment, comorbidities and pharmacological data of the entire population studied are shown in Table 1.
General characteristics and description of the population studied.
| Variable | Results |
|---|---|
| Number of residents | 436 |
| Median age, years (IQR) | 87 (11) |
| Gender, n (%) | 316 women (72.1) |
| Functionality and cognitive functioning | |
| Median Barthel Index (IQR) | 38.0 (61.0) |
| GDS≥5, n (%) | 239 (54.8), 26 lost |
| GDS≥6, n (%) | 169 (38.6), 26 lost |
| Frailty | |
| Median Frail-VIG (IQR) | 0.44 (IQR=0.16), 116 lost |
| Frail-VIG>0.5 | 23.1% (n=74), 116 lost |
| BMI mean (SD) | 25.31 (5.1), 30 lost |
| Co-morbidity | |
| Dementia, n (%) | 297 (68.1) |
| AHT, n (%) | 258 (58.9) |
| Diabetes, n (%) | 86 (19.6) |
| COPD, n (%) | 45 (10.3) |
| Pharmacological characteristics | |
| Number of medications, median (IQR) | 7.0 (4.0) |
| Antiplatelet, n (%) | 100 (22.9) |
| Anticoagulants, n (%) | 60 (13.8) |
| Antipsychotics, n (%) | 201 (46.1) |
| BZD and analogues, n (%) | 197 (45.2) |
| Antidepressants, n (%) | 276 (63.3) |
| Polypharmacy | |
| Polypharmacy (≥5 medications), n (%) | 345 (79.1) |
| Hyperpolypharmacy (≥10 medications), n (%) | 100 (22.9) |
AHT: hypertension; BMI: body mass index; BZD: benzodiazepines; COPD: chronic obstructive pulmonary disease; GDS: Global Deterioration Scale; Frail VIG: frailty index based on the comprehensive geriatric assessment; IQR: interquartile range; SD: standard deviation.
173 residents were infected with SARS-CoV-2 (39.7%), two of the NHs were infected during the first wave (March–May 2020) and the other two during the second wave (October–December 2020). 122 people (70.5%) had symptoms (12.1% delirium, 32.4% oxygen saturation <90%, 28.9% coughing, 27.1% fever >38°C). Of those residents infected, 113 (65.3%) were treated in their NH, 33 (19.0%) were referred to acute care hospitals or intermediate care units, and the rest 27 (15.6%) were referred to NHs or social health centres established as monographic centres for the care of SARS-COV-2 positive patients.
There were no significant differences in the profile of the patient transferred or not to the hospital in terms of age, frailty (Frail-VIG index) or dependence (Barthel index), but there were in women and in those with advanced dementia (GDS≥6) that were less likely to be transferred (Table 2).
Location of residents infected by SARS-CoV-2 after diagnosis.
| Variable | NH | Hospitalized | p |
|---|---|---|---|
| Number of residents (%) (3 lost) | 137 (79) | 33 (19) | |
| Median age, mean (IQR) | 85.74 (6.6) | 84.85 (8.7) | 0.60 |
| Gender, n (%) | 105 women (76.6) | 17 women (51.5) | 0.04* |
| Functionality and cognitive functioning | |||
| Median Barthel Index (IQR) | 40.0 (61.0) | 60.0 (58.0) | 0.09 |
| GDS≥6, n (%) | 51 (38.9) | 5 (16.1) | 0.02* |
| Frailty | |||
| Median Frail-VIG (IQR) | 0.40 (0.16), 19 lost | 0.40 (0.16), 5 lost | 0.75 |
| BMI mean (SD) | 25.75 (5.37) | 26.60 (5.39) | 0.42 |
| Pharmacological characteristics | |||
| Number of medications, median (IQR) | 8.0 (4.0) | 8.0 (6.0) | 0.07 |
NH includes those residents who remained in the NH of origin and those who were referred to COVID-19 specific NHs.
BMI: body mass index; GDS: Global Deterioration Scale; Frail VIG: frailty index based on the comprehensive geriatric assessment; IQR: interquartile range; SD: standard deviation.
People with dementia and GDS≥6 were less likely to be infected by SARS-CoV-2 virus with an OR of 0.64 (95% CI 0.43–0.97; p<0.05). There was a trend for people with diabetes to a higher risk of acquiring the infection (OR 1.61 (95% CI 0.98–2.64), p=0.061). No other significant differences were found in the variables studied among people infected and not infected by the virus (Nagelkerke's R2: 0.03 and Hosmer and Lemeshow test: 0.88) (Table 3).
Bivariate and multivariate analysis of association between demographic, clinical and pharmacological factors and SARS-CoV-2 infection.
| Variable | Acquire SARS-CoV-2 (n=173) | Doesn’t acquire SARS-CoV-2 (n=263) | Crude OR (95% CI) | Crude p-value | Adjusted OR (95% CI) | Adjusted p-value |
|---|---|---|---|---|---|---|
| Mean age (SD) | 85.68 (8.6) | 85.53 (8.8) | 0.861 | |||
| Men, n (%) | 49 (28.3) | 72 (27.4) | 1.05 (0.68–1.61) | 0.829 | ||
| Mean Barthel Index (SD) | 45.95 (32.3) | 40.35 (31.57) | 0.074 | |||
| Dementia, n (%) | 116 (39.6) | 181 (69.9) | 0.89 (0.59–1.35) | 0.592 | ||
| GDS≥6, n (%) | 57 (34.5)9 lost | 112 (45.3)17 lost | 0.64 (0.43–0.97) | 0.033* | 0.65 (0.43–0.97) | 0.037* |
| Mean Frail-VIG index (SD) | 0.41 (0.103)26 lost | 0.41 (0.122)90 lost | 0.899 | |||
| BMI≥30 (%) | 29 (17.6)9 lost | 33 (13.7)21 lost | 1.34 (0.78–2.32) | 0.285 | ||
| AHT, n (%) | 106 (61.3) | 151 (57.4) | 1.17 (0.79–1.74) | 0.423 | ||
| Diabetes, n (%) | 42 (24.3) | 44 (16.7) | 1.60 (0.99–2.57) | 0.053 | 1.61 (0.98–2.64) | 0.061 |
| COPD | 20 (11.6) | 25 (9.5) | 1.24 (0.67–2.32) | 0.490 | ||
| Mean medications (SD) | 7.46 (3.13) | 7.05 (3.57) | 0.218 | |||
| Hyperpolypharmacy†, n (%) | 44 (25.4) | 55 (20.9) | 1.29 (0.82–2.03) | 0.270 | ||
| Anticoagulants, n (%) | 21 (12.1) | 38 (14.5) | 0.82 (0.46–1.45) | 0.481 | ||
| Antiaplatelets, n (%) | 39 (22.5) | 60 (22.8) | 0.99 (0.62–1.56) | 0.947 | ||
| Antipsychotics, n (%) | 76 (43.9) | 125 (47.5) | 0.87 (0.59–1.27) | 0.461 | ||
| BZD and analogues, n (%) | 83 (48.0) | 112 (42.6) | 1.24 (0.85–1.82) | 0.268 | ||
| Antidepressants, n (%) | 112 (64.7) | 163 (62.0) | 0.89 (0.60–1.32) | 0.559 |
AHT: arterial hypertension; BMI: body mass index; BZD: benzodiazepines; COPD: chronic obstructive pulmonary disease; GDS: Global Deterioration Scale; OR: odds ratio; SD: standard deviation.
Forty-five residents died from COVID-19 (26.0% of those who acquired the infection, 10.3% of the entire sample). The average number of days between the first PCR positive and death was 10.3 (SD=7.9) days (range 1–31). 23 residents (51.1%) died in the NH. People transferred to hospitals were more likely to die (41.7%) than those that remained in NH with COVID-19 (16.3%) (OR 3.7 (95% CI 1.4–9.9); p=0.01).
As shown in Table 4, neither age nor gender were factors that influenced COVID-19 mortality. However, a low Barthel index or advanced dementia (GDS≥6) were factors associated with higher COVID-19 mortality (p<0.05). The mean Frail-VIG index of those who died from COVID-19 was 0.45 (SD=0.08), while for those who acquired the infection and did not die was 0.39 (SD=0.11), the difference being statistically significant (p=0.001). Obesity was not a factor associated with COVID-19 mortality, nor were T2DM or AHT influencing factors. However, the relation between COPD sufferers and COVID-19 mortality was statistically significant (p=0.026).
Bivariate and multivariate analysis of association between demographic, clinical and pharmacological factors and covid-19 mortality.
| Variable | Dies from COVID-19 (n=45) | Doesn’t die from COVID-19 (n=128) | Crude OR (95% CI) | Crude p-value | Adjusted OR (95% CI) | Adjusted p-value |
|---|---|---|---|---|---|---|
| Mean age (SD) | 86.71 (9.3) | 85.28 (8.3) | 0.339 | |||
| Men, n (%) | 15 (33.3) | 34 (26.6) | 1.37 (0.66–2.85) | 0.402 | ||
| Mean Barthel Index (SD) | 37.33 (31.07) | 49.29 (32.25) | 0.032* | |||
| Dementia, n (%) | 35 (77.8) | 80 (62.5) | 2.01 (0.91–4.44) | 0.080 | ||
| GDS≥6, n (%) | 23 (53.5)2 lost | 34 (26.6)7 lost | 2.91 (1.42–5.97) | 0.003* | 4.9 (1.5–16.1) | 0.010* |
| Mean Frail-VIG index (SD) | 0.45 (0.08)4 lost | 0.39 (0.11)22 lost | 0.001* | |||
| BMI≥30 (%) | 9 (20.5)1 lost | 20 (16.7)8 lost | 0.78 (0.32–1.87) | 0.573 | ||
| AHT, n (%) | 25 (55.6) | 81 (63.3) | 0.71 (0.36–1.41) | 0.330 | ||
| Diabetes, n (%) | 10 (22.2) | 32 (25.0) | 0.85 (0.38–1.91) | 0.690 | ||
| COPD, n (%) | 9 (20.0) | 10 (7.9) | 2.93 (1.10–7.75) | 0.026* | 7.8 (1.9–31.3) | 0.004* |
| Mean medications (SD) | 8.33 (3.4) | 7.13 (3.0) | 0.027* | |||
| Hyperpolypharmacy†, n (%) | 17 (37.0) | 27 (21.1) | 2.25 (1.08–4.70) | 0.029* | ||
| Anticoagulants, n (%) | 5 (11.1) | 16 (12.5) | 0.87 (0.30–2.52) | 0.793 | ||
| Antiaplatelets, n (%) | 11 (24.4) | 27 (21.1) | 1.20 (0.54–2.67) | 0.658 | ||
| Antipsychotics, n (%) | 29 (64.4) | 47 (36.7) | 3.09 (1.52–6.27) | 0.001* | 3.1 (1.0–9.0) | 0.041* |
| BZD and analogues, n (%) | 28 (62.2) | 54 (42.2) | 2.23 (1.11–4.47) | 0.023* | 2.8 (0.9–8.5) | 0.062 |
| Antidepressants, n (%) | 33 (73.3) | 78 (60.9) | 1.73 (0.82–3.66) | 0.151 |
AHT: arterial hypertension; BMI: body mass index; BZD: benzodiazepines; COPD: chronic obstructive pulmonary disease; GDS: Global Deterioration Scale; OR: odds ratio; SD: standard deviation.
The mean number of drugs prescribed per resident, as well as those with hyperpolypharmacy (≥10 drugs) were factors related to COVID-19 mortality (p<0.05, the more drugs prescribed, the higher the COVID-19 mortality). Taking antipsychotics and benzodiazepines had a statistically significant relationship with COVID-19 mortality (p<0.01 and p=0.023 respectively). However, neither antiplatelet or chronic anticoagulants, nor antidepressants were associated with COVID-19 mortality (p>0.05).
In an adjusted analysis to determine the main predictive variables on COVID-19 mortality, a multivariate regression revealed that COPD (OR 7.8 (95% CI 1.9–31.3, p<0.01)), a GDS≥6 (OR 4.9 (95% CI 1.5–16.1, p=0.01)), antipsychotic use (OR 3.1 (95% CI 1.0–9.0, p=0.041)) and benzodiazepine use (OR 2.8 (95% CI 0.9–8.5, p=0.062)) were the most influential variables, the first 3 being statistically significant (Nagelkerke's R2: 0.33 and Hosmer and Lemeshow test: 0.85).
DiscussionResearch has shown that residents with dementia and GDS≥6 infected less by SARS-CoV-2 but died more. Besides, those with COPD and those who took antipsychotics died more.
Little is known about characteristics of people in NHs and risk of acquiring SARS-CoV-2. Some authors14 identify risk of infection by SARS-CoV-2 dependent of respiratory diseases, cardiovascular diseases and low level of functional dependence of daily living. Another study6 identify BMI and estimated poor life expectancy associated with a higher risk of infection. We found dementia and a GDS≥6 and diabetes the only two variables with an association to lower and higher risk of infection, respectively, only the first being statistically significant. On the other hand, the validity of the model was poor.
Regarding the relationship between dementia and COVID-19, in our study we found that advanced dementia (GDS≥6) is associated with lower risk of SARS-CoV-2 infection and a higher risk of mortality due to COVID-19, but not dementia as a diagnosis. However, the work of Yu and colleagues found that the diagnosis of Alzheimer's disease itself predicts the highest risk of SARS-COV-2 and mortality in older people.15 In our study, 68% of the people studied had a diagnosis of dementia, which may be the cause of these differences. In any case, the lower risk of infectivity associated with advanced dementia is surprising due to lower capacity to respect the measures of partner distance and use of a mask in those people.
Besides, it is interesting how the indicator that is associated both with infection and with mortality is not the history of dementia but the GDS≥6, which indicates the relevance of carrying out this assessment periodically.
In our analysis, we found that demographic variables such as age and gender were not significantly associated with COVID-19 mortality in the institutionalised residents studied, neither T2DM nor AHT. Several studies have reported that different comorbidities increase COVID-19 mortality, such as respiratory and cardiovascular pathologies.16,17 Its predominance in the older people has led some authors to establish age as an important risk factor in mortality from COVID-19.18 There are, however, varying data; some authors found an association between being older than 80 years and being a male with mortality due to COVID-19 in NH residents19 and other found no differences due to age but did find higher mortality for men.15,20,21 It should be borne in mind that in our case 72% of the population studied were women.
Our results show that advanced dementia (GDS≥6), COPD and antipsychotic use are variables related to COVID-19 mortality. In an unadjusted logistic regression analysis, a low Barthel index, frailty, hyperpolypharmacy and benzodiazepine use are added to these variables. These findings indicate the need for precaution with advanced dementia patients, those with COPD, dependent and frail patients and, above all, more importantly, as these are modifiable variables, to review polypharmacy and specifically the use of antipsychotics and benzodiazepines and its combination. It is important to highlight the strong association between COPD and COVID-19 mortality, since, despite being only 19 cases, the OR in the multivariate analysis is as high as 7.8.
In terms of medication use, prior use of antipsychotics and benzodiazepines were found to be associated with COVID-19 mortality; hyperpolypharmacy also seems to indicate a similar relationship. In the same way, a matched case–control study investigated the possible relationship between severe COVID-19 and previous drug treatment. It found that severe COVID-19 was associated with polypharmacy and with drugs that cause sedation, respiratory depression or dyskinesia; those with anticholinergic effects; and with drugs that affect the gastrointestinal system such as proton pump inhibitors. Antipsychotics were the drugs with the greatest effect (rate ratio 4.18 (3.42–5.11)).10
This work found that 39.7% of residents tested positive for SARS-CoV-2 and 10.3% died (26% of those who acquire the infection). This observation is similar to that published by Graham et al. in the United Kingdom20 who found that 40% became infected and 13% died and to that by Soldevila et al. in Catalonia, Spain14 with 27.7% infected and 11.3% died, the two of them in NHs. The findings in mortality are lower than those reported in some NHs in Madrid, Spain22 and in the Netherlands23 where 44.7% and 47.5% of the NH residents with COVID-19 died, respectively.
Healthcare institutions and other structures such as NHs had to move quickly at the beginning of 2020 in the face of a new and highly demanding type of infection. This is likely to explain the different hospitalisation rates of NH residents in different countries. In our study only 19% were referred to hospitals, much lower than that published by McMichael and colleagues (54.5%) in Washington24 or the geographically closest figure of 45.9% in Madrid.22 It should be noted that in our case, around 15% of residents were referred to NHs or social health centres specifically prepared to care for people with this new infection, so these differences may be due, at least in part, to the different strategies adopted locally.
In our NHs only advanced dementia (GDS≥6) was a criterion for non-derivation, which differs from what was observed by other authors22 who found differences in the derived profile with respect to factors such as age (mean age 87 vs 88), frailty (median CSF 6 vs 7), Barthel's index (45 vs 30), dementia (39.4% vs 57.8%) and more comorbidity (2 vs 1), derived vs not, respectively. These same authors22 found no differences in mortality in patients transferred with respect to those not transferred, which also occurs differently in our work, with higher mortality in those referred to the hospital compared to those who continue in residential care (41.7% vs 16.3%), which will probably be due to less severe forms of presentation of COVID-19.
Our findings should be considered in light of several limitations. One of them is that only those cases available have been studied. This little sample size could have conditioned some results (for example, the number of people who die from COVID-19 was only 45). It would be very interesting to delve into this type of study with larger sample size. Another set of limitations correspond to the loss of some records, although they have been distributed in the groups. Data on symptomatology and evolution of the infection may have been lost in some referral centres and in people who died, something which has been a limitation. The comprehensive assessments at the institution to which the NHs belong are carried out usually once a year and in the event of important changes in the resident, but have not been updated as rigorously due to the workload imposed by the pandemic, which may have led in some cases to data being less up-to-date than they should. It is believed that this would in any case have led to maximising certain results.
The strengths of this study are related to the important impact of the COVID-19 pandemic on the NHs, so knowing the factors that may induce a higher risk of infection and mortality in these homes is important for establishing priorities and actions for future interventions.
As conclusion, the results of this study show that advanced dementia (GDS≥6) has been associated with less risk of SARS-CoV-2 infection but higher risk of COVID-19 mortality. COPD and chronic use of antipsychotics have also been associated with mortality from this disease. These results highlight the importance of determining the stage of diseases such as dementia as well as maintaining some caution in the use of some drugs such as antipsychotics and may be useful in taking the utmost precaution in this predominantly frail population.
- •
The pandemic has led a major crisis in NH.
- •
Information is needed to deal with future outbreaks and new infectious diseases.
- •
It is necessary to create secure NH models as they attend fragile people.
- •
The study enlarges the knowledge about the SARS-CoV-2 infection and mortality risk factors in institutions with a significant risk of spreading the virus and in a population at special risk of severity.
- •
The results of this work show a relationship between SARS-CoV-2 infection and mortality from COVID-19 with some clinical and pharmacological factors, not so much with demographic ones.
- •
In our study, only 19% of those residents infected with SARS-CoV-2 were referred to acute care hospitals or intermediated care units. Those transferred were more likely to die most likely due to the severity of the infection.
- •
Residents with dementia and GDS≥6 have shown higher mortality from COVID-19, as well as those with COPD presenting an OR of 7.8. We want to highlight the relationship of medications such antipsychotics and benzodiazepines, an aspect that necessary needs to be studied because it is potentially modifiable.
Observational and retrospective study. The work was approved for execution by the local Research Ethics Committee with acceptance of waiver of informed consent request. Residents’ identification data were anonymised in the database.
FundingNone declared.
Conflict of interestNo conflict of interest.