El cumplimiento medio final de criterios en el grupo de información escrita fue del 74%, frente a un 82% en el grupo de información oral. Conclusiones. El uso de información escrita sobre el uso de aerosoles en pacientes con EPOC mejora significativamente su calidad de utilización, en grado similar a su explicación oral.
Introduction
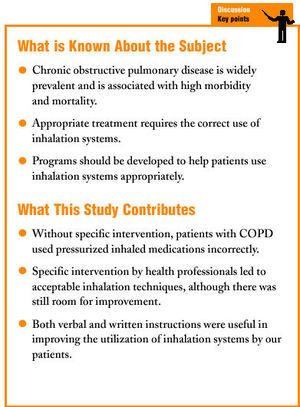
Diseases of the respiratory system continue to pose substantial public health problems, given their high morbidity and mortality. One of the most prevalent respiratory diseases is chronic obstructive pulmonary disease (COPD), and appropriate health education for these patients is necessary for self-care and control of the disease. These patient should be encouraged to quit smoking, and should be taught to use prescription medications correctly. Inhaled medications should be the treatment of choice whenever possible, as they make it possible to administer high concentrations of the active principle directly to the site of action. This diminishes systemic side effects and increases therapeutic efficacy.1-4
However, the inhalation route also has some disadvantages, especially in that it requires some skill on the patient's part to ensure correct administration. To offset this disadvantage, several devices are available such as pressurized canister inhalers, spacers, and dry powder inhalers,5-8 although the most commonplace and widely used device is the pressurized canister inhaler.
To ensure the correct us of these devices, health professionals usually provide brief instruction, although large patient loads often leave little time for this. The pharmacist or a relative usually provides additional information. Nevertheless, there are a number of questions remain to be answered: do our patients use pressurized canister inhalers correctly? Which kind of health education is the most effective? Is verbal information as effective as written information?9,10
Because of these questions, and with the aim of improving inhalation techniques in our patients, we designed the present study with two main objectives:
1. To determine whether the use of written information alone improved the performance of pressurized canister inhaler technique in patients with COPD.
2. To compare the effectiveness of written information alone on the use of inhalers with that of verbal information given by nursing staff members.
Material and Methods
This interventional study was done at an urban health center located outside the city center. The participants were 120 patients with a diagnosis of COPD who were prescribed daily treatment with pressurized canister inhalers for more than 3 months. We excluded patients who used inhalers on an as-needed basis only, or who used them only occasionally. Other criteria for exclusion were psychiatric disorder, dementia or neurological disease that might interfere with the patient's ability to coordinate the steps in the correct use of inhalers. Chronic obstructive pulmonary disease was diagnosed on the basis of spirometric criteria (FEV1/FVC<70%).
All patients were men aged between 60 and 75 years. We excluded patients who had not received primary education or who were illiterate. Women were excluded to maximize similarity
between groups, and because of the higher prevalence of COPD among men. Table 1 shows the distribution of patients according to smoking habit. All patients were recruited during the same 6-month period from among patients assigned to 5 family physicians at our health center, located in a suburban area.
The 120 patients were divided randomly into 3 groups of 40 patients each, who did not differ significantly in any of the demographic characteristics. No intervention was used in the first group, verbal explanation was used as the intervention in the second group, and written information was provided as the intervention in the third group. The verbal intervention consisted of a detailed, 5-minute explanation of the inhalation technique (Table 2),11 provided by a member of the nursing staff. At the end of the explanation patients were asked to demonstrate their inhalation technique with a placebo. The written intervention consisted of giving the patient a pamphlet with printed instructions (Table 2). No verbal explanation was provided, and the patient's performance of the inhalation technique was not checked.
The outcome measurement consisted of calculating percentage compliance with each of the 5 criteria for the correct use of inhalers at the start of the study and 3 months after the intervention in all groups. Age, sex, and level of education (no formal education, primary school, secondary school, university) were recorded for all patients. Data on the performance of inhalation technique were recorded by a nurse specially trained in the use of inhalation systems, who observed each patient as he or she performed 2 consecutive inhalations. The following criteria were evaluated:
Criterion 1: each patient with COPD who uses pressurized canister inhalers should exhale completely before pressing down on the canister.
Criterion 2: each patient who uses inhalers to treat COPD should breath in slowly after exhaling completely.
Inhalation was considered slow when it lasted more than 4 seconds.
Criterion 3: each patient who uses inhalers to treat COPD should depress the canister only after inhalation has begun. This criterion was considered to be performed correctly only when the canister was depressed during the first second of inhalation.
Criterion 4: each patient who uses inhalers to treat COPD should hold his or her breath for 10 seconds after inhaling the dose.
Criterion 5: each patient who uses inhalers to treat COPD should keep his or her lips closed firmly around the mouthpiece during the procedure.
To compare the initial and follow-up findings, statistical analysis consisted of calculation, for each criterion, of absolute and relative improvement (referred to greatest possible improvement) and statistical significance (with one-tailed z tests for comparison of proportions). To create a database and analyze the data we used the SYSTAT program (version 5.0).12 A P value <0.05 was considered statistically significant. On the basis of our study design, a sample size of 40 for each group was considered sufficient.
Results
We found no significant differences between groups in age, sex, or level of education. At the initial evaluation inhalers were found to be used incorrectly by our patients with COPD: mean compliance with the criteria was 40% in all 3 groups. There were no significant differences between groups at this initial evaluation, a result that confirmed homogeneity of the sample of participants. In overall terms, criterion 4 (holding breath for 10 seconds after inhaling the dose) was performed correctly by only 8% of the patients. In contrast, overall compliance with criterion 3 at the initial evaluation (i.e., before the intervention) was 72.5% (Table 3).
After verbal or written information was given, performance improved significantly for all criteria (P<.05) in both intervention groups, with no significant differences between them (ns). Mean final compliance for all criteria in the group that received written information was 74%, versus 82% in the group that received verbal information. Compliance with criterion 4, which was only 8% at the initial evaluation, increased to 55.5% in the group that received verbal information, and to 37.5% in the group that received written information. These figures indicate that additional improvements in compliance are desirable. Compliance with criterion 3, which was already high in the initial evaluation, increased further to 97% in the verbal intervention group, and to 95% in the written intervention group. Compliance with the other three criteria also improved significantly (Table 3).
In the group that received no intervention we found no significant improvements in compliance in the second evaluation. This group served as a control to facilitate the identification of variables that might have interfered with the results.
Discussion
The present study evaluates inhalation techniques used with the inhalation system indicated most frequently by health professionals. Initially we found that pressurized canister inhalers were being used incorrectly by patients with COPD. This indicated that despite correct prescribing practices by physicians, the results obtained are not those anticipated by the patient or the health professional. Performance improved significantly in both intervention groups, with no significant differences between the two. Hence a specific intervention for this type of treatment significantly enhances its efficacy. The results of studies such as the present one are increasingly important to maintain the viability of the current national health system in Spain.
We note that there were no significant differences in the results between the groups that were given verbal and written instructions about the correct technique for using pressurized canister inhalers. This may represent considerable time saved at each patient-physician contact, as simply handing the patient a pamphlet and urging the patient to read it carefully may achieve the same results as spending a few minutes to explain the technique verbally. We also found that if the patient is given no verbal or written information about how to use pressurized canister inhalers, the results will be poor, and treatment will not have the expected effect.
Madueño et al13 investigated whether primary care physicians in training had adequate theoretical and practical knowledge about inhalation systems. These authors found that inhalation systems were often misused, and recommended specific training for primary care professionals in the use of inhaled drug therapy. Their findings indicate that if health professionals are not familiarized with the use of these devices, we will not be able to explain to our patients how to use them appropriately. Other studies14-17 have also analyzed how patients use inhalers, and have found performance of inhalation techniques to be poor. These findings suggest that greater emphasis should be placed on inhalation techniques, and that physicians should ensure that the patients knows how to use the inhaler correctly. It is important to emphasize here that using an inhaler incorrectly is equivalent to not taking any medication at all.
Among the potential biases in this study is the limitation imposed by including only patients with COPD, as pressurized canister inhalers are also widely used for chronic diseases such as asthma and interstitial disorders, as well as for acute diseases such as bronchitis and pneumonia. It should be recalled that patients with an acute disease have less experience, hence the rate of incorrect inhalation technique can be assumed to be higher among them. Another potential source of bias is the fact that when we designed the study, we did not take into account measures by the pharmaceutical industry to improve patients' inhalation technique by producing improved devices that require less coordination to use correctly. It would be interesting to compare the different devices now available on the market.
Future studies in this area should be designed to analyze the efficacy of information provided to the patient at the pharmacy, and to compare this information with that provided at the health center. Fomenting cooperation between pharmacies and health center professionals is a key step toward improving compliance with therapy and providing effective health education for these patients.
In conclusion, the use of written information about inhalation techniques for the use of aerosols by patients with COPD significantly improves performance, and the improvements are similar to those obtained when patients are given a verbal explanation of how to use the inhaler.