The rapid pace of socioeconomic development in the Arabian Gulf nations and the rapidly changing environment are probably determining the altering scenario of child and adolescent nutrition in the developed societies. The rapid urbanization in everyday life, accompanied by decreased levels of physical activity and increased caloric intake of non-traditional food has become responsible for the emerging of obesity in children and adolescents as a major public health issue in these countries. The six Arabian Gulf nations are a good example for this developmental transition and its consequences.
Prevalence is high among Kuwaiti and Saudi pre-school children (8–9%), and among the highest in the world among Kuwaiti adolescents (40–46%), taking into account that different standard of assessment of obesity are used. Although data on the prevalence of type 2 diabetes (T2DM) and metabolic syndrome (MS) in children in the region are sparse, both morbidities are expected to rise, knowing the strong association between obesity and T2DM in the adult population. Prevention strategies need the collaborative efforts of governmental and community-led agencies to establish long-term programs to improve health education, targeting young children and their families. Healthy eating and physical activity should be promoted and encouraged in schools, nurseries, and child care settings.
This article gives an overview of overweight and obesity among children and adolescents in the 6-Arabian Gulf countries. It will also address possible strategies for the prevention and management of this major health epidemic.
El frenético ritmo de los avances socioeconómicos en los países del Golfo Pérsico y el rápidamente cambiante entorno está probablemente definiendo el perturbador panorama de la nutrición de niños y adolescentes en las sociedades desarrolladas. La fugaz urbanización de la vida diaria, acompañada por unos niveles reducidos de actividad física y un aumento de la ingesta calórica en forma de alimentos no tradicionales, ha convertido la obesidad en los niños y adolescentes en un tema de salud pública de gran importancia en estos países. Los seis países del Golfo Pérsico son un buen ejemplo de esta transición en el desarrollo y de sus consecuencias.
La prevalencia es elevada entre los niños preescolares kuwaitíes y saudíes (8%-9%), y entre los adolescentes kuwaitíes cuenta con una de las más elevadas en el mundo (40%-46%), de cuerdo con diferentes estándares para valorar la obesidad. Aunque los datos sobre la prevalencia de la diabetes tipo 2 (DMT2) y el síndrome metabólico (SM) en los niños de la región son escasos, se esperan que ambas morbilidades aumenten, debido a la existencia de una importante asociación entre la obesidad y la DMT2 en la población adulta. Las estrategias de prevención exigen una fuerte colaboración entre el gobierno y las agencias dirigidas por la comunidad para establecer programas a largo plazo para mejorar la educación sanitaria, centrada en los niños pequeños y sus familias. Es necesaria la promoción de una dieta saludable y de la actividad física tanto en colegios, como en guarderías y centros de puericultura.
Este artículo aporta una visión general del sobrepeso y la obesidad en niños y adolescentes en los seis países que conforman el Golfo Pérsico. También se contemplan posibles estrategias para la prevención y la gestión de esta importante epidemia sanitaria.
The Gulf Cooperation Council (GCC) is a political and economic union of the Arab states bordering the Arabian Gulf and constituting the Arabian Peninsula, namely Bahrain, Kuwait, Oman, Qatar, Saudi Arabia, and United Arab Emirates.1 The discovery of oil in the middle of the 20th century led to rapid socioeconomic development and epidemiologic transition.2 This resulted in a significant reduction in infant and child mortality rates approaching those of many developed countries.3
The growing urbanization and nutrition transition are largely blamed for the increasing prevalence rates of childhood and adolescent obesity and type 2 diabetes.4 In fact, the prevalence of overweight and obesity in the GCC, in some cases, is exceeding that of many developed nations.2
The health of adolescents have been neglected for many years because they are generally considered to be less vulnerable to diseases than children and elderly.5 However, there is now substantial evidence that overweight and obesity in childhood and adolescents lay the ground for adult obesity and the other risk factors associated with cardiovascular diseases.6
Worldwide, there are a total of 155 million children (one in 10) who are overweight and 30–40 million who has been classified are obese.3 The incidence of obesity-related conditions is increasing rapidly among adolescents, including type 2 diabetes; a disease previously non-existing until middle-age.5
This review will shed the light on the problem of obesity and type 2 diabetes in children and adolescents in the Arabian Gulf region, and suggests possible solutions for its prevention.
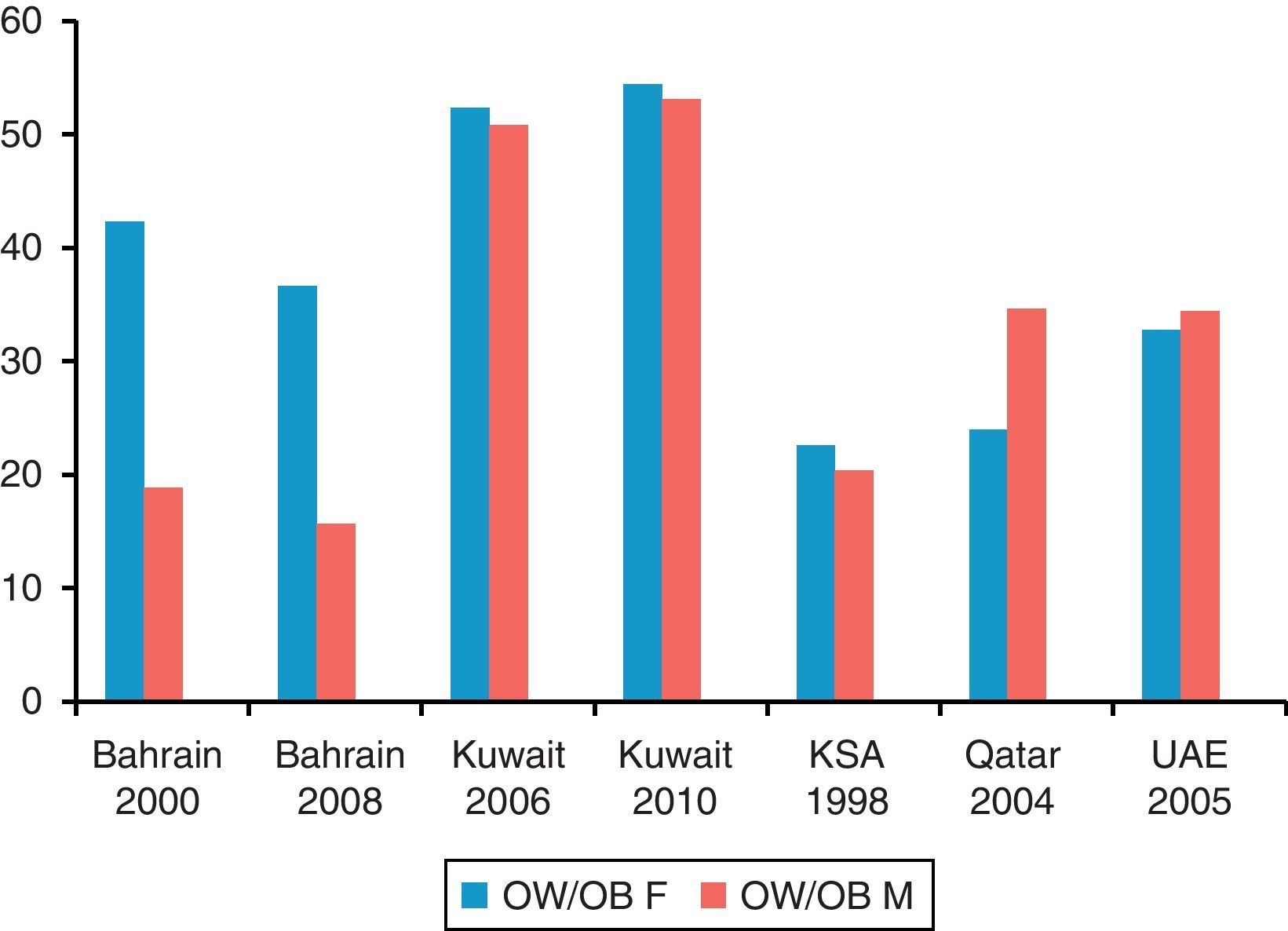
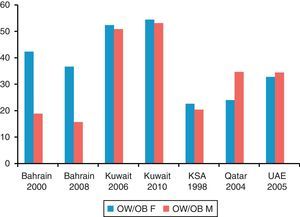
Overweight and obesityAlthough there are at least five definition used for overweight and obesity in children, it is evident that the prevalence of obesity among adolescents in the GCC countries is alarming (Fig. 1). In Bahrain, studies have revealed that obesity (BMI>95th percentile for age), among adolescent girls in the age group 10–13 year is 25%, and in the age group 14–18-year, it reached up to 38.5%.8 The mean weights for heights for girls were higher than those reported earlier7 in the same age group with no significant difference in the mean height between 1989 and 2000, indicating an increase in the fat mass among Bahraini girls.
In another report8 obesity was highest (21%) in males and in females (35%) 12–17 years of age, when the WHO criteria were used (BMI and skin fold percentile) but dropped to 15% and 18% when the age-specific BMI cut-off values were used.9 In a recent cross national survey,10 current generation of Bahraini children showed substantially higher values in arm circumference size compared to surveys done a decade ago,10 and showed an increased trend toward adiposity.
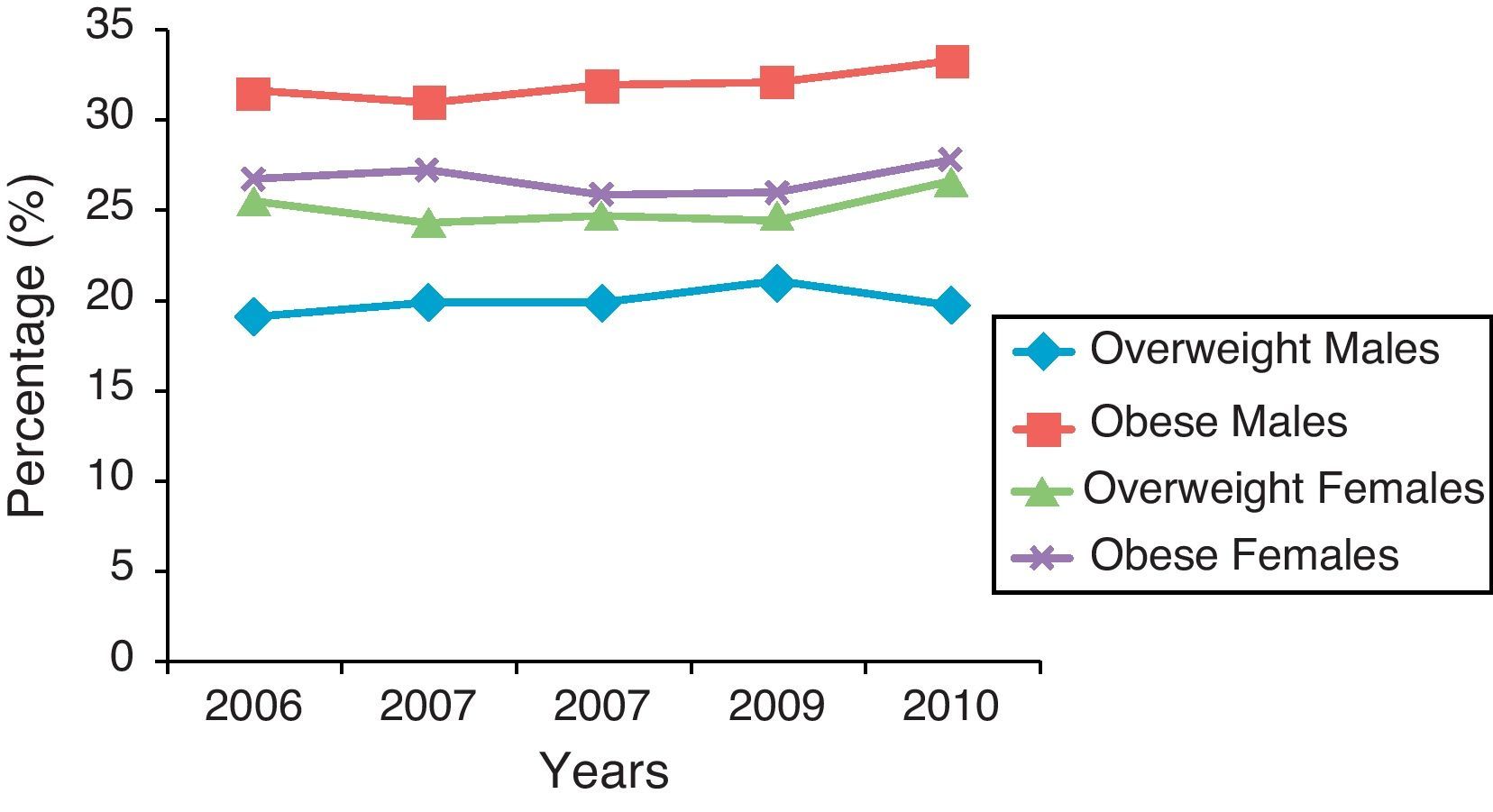
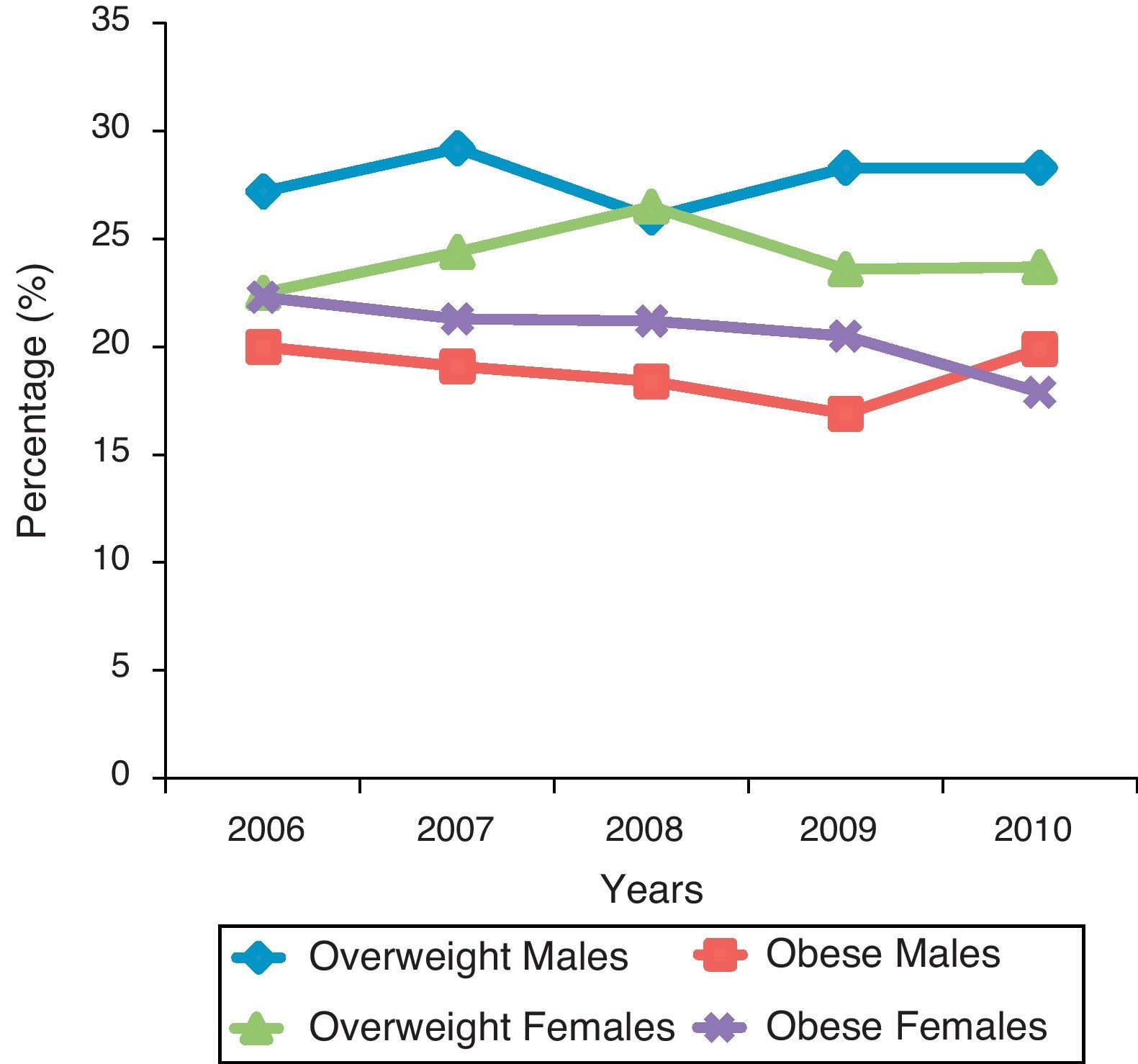
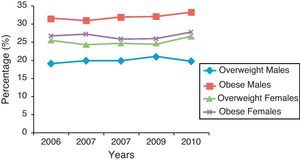
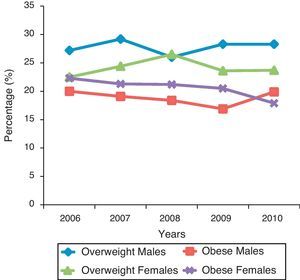
In Kuwait, since 2001, a nation-wide Nutrition Surveillance system has been implemented. The indicators include anthropometrical data on height and weight in different age groups, biochemical tests for anemia in all ages, blood sugar and cholesterol for the prevalence of diabetes and hyperlipidemia in adults. The recent data (2006–2010) showed that overweight (BMI>+2SD) among children less than 5-year-old, ranged from 5.2% in 2010 to 6.7% in 2008, and obesity (BMI>+3SD) from 2.2 in 2010 and 2.8% in 2006.11 For the 5–9-year age group, overweight in males ranged from 13.9% in 2007, and 15.7% in 2010. For females of the same age group, it ranged from 16.4% in 2007 to 18.6% in 2006. For the intermediate school boys and girls, 10–14 year old, (Fig. 2), 33.3% of the boys and 27.8% of the girls in 2010 were found to be obese, and 19.8% of the boys and 26.6% of the girls were overweight. Prevalence of obesity was significantly higher in this age group among boys. Similar finding was observed in the 15–19 year-age group (Fig. 3).11 In another recent cross-sectional study,12 involving more than 5000 school children, 10–14 year-old, the overall prevalence of overweight (BMI 85th–94th percentile) was 29.3% in males and 32.1% in females. For obesity (BMI>95th percentile), the overall prevalence was 14.9% in males and 14.2% in females. These data are much higher than those detected by the surveillance system. This is explained by the variability in the definition of both overweight and obesity used. Risk factors for overweight and obesity identified in the surveillance were excess caloric intake, lack of physical activity, excessive soft drinks and fast food consumption and frequent snacking. Moreover, among the obese and overweight children, 89% belonged to high social class families. These results were in agreement with results from neighboring countries9 and international studies.13 In another study on 700 Kuwaiti elementary male school children aged 6–10 years, 20.2% were found to be overweight, and 16.8% were obese.14 Having one or more obese brother, an unemployed father or a high (>11) number of persons living at home were significantly associated with higher risk of overweight and obesity.15
Oman society is not an exception for obesity being a serious health problem, the national health survey in 2000 of Omani adults showed that in the youngest surveyed age-group (20–34 years) 36.1% were overweight or obese, 26% had hypercholesteremia, 17.7% had hypertension and 8.4% had either type 2 diabetes or impaired glucose tolerance test.16 Data on children are lacking. In one paper studying the progression of weight status among a cohort of Omani school children in one city, the researcher revealed that the incidence of overweight and obesity progressively increased from a combined rate of 7.3% children aged 6–7 to 16% at 12–13 year and further increased to 23.3% in children aged 15–16. No previous studies are available to show the trend. Further analysis of the data showed that the risk of overweight and obesity at age 15–16 years was higher among students who were previously overweight or obese at younger age.17
The state of Qatar has experienced rapid social and economic changes and significant rise in per capita income, particularly during the oil flood of 1973–81.18 The improved health services have led to dramatic reduction in infant mortality rates and better nutrition status of the population. In a sample representing 11% of the Qatari students aged 12–17 years, using the international obesity task force (IOTF) cut-offs, the prevalence of overweight was 28.6% among boys and 18.9% among girls, and for obesity, it was 7.9% among boys and 4.7% among girls. In another study involving children and adolescents aged 6–18 years, 4.7% of males and 5.6% of males were either overweight or obese by the Qatari reference (BMI>95th percentile). When the IOTF cut-offs were used as reference for obesity, 24.3% of males and 18.7% of the females were found to be overweight, and 6.1 and 3.6% were found to be obese.19
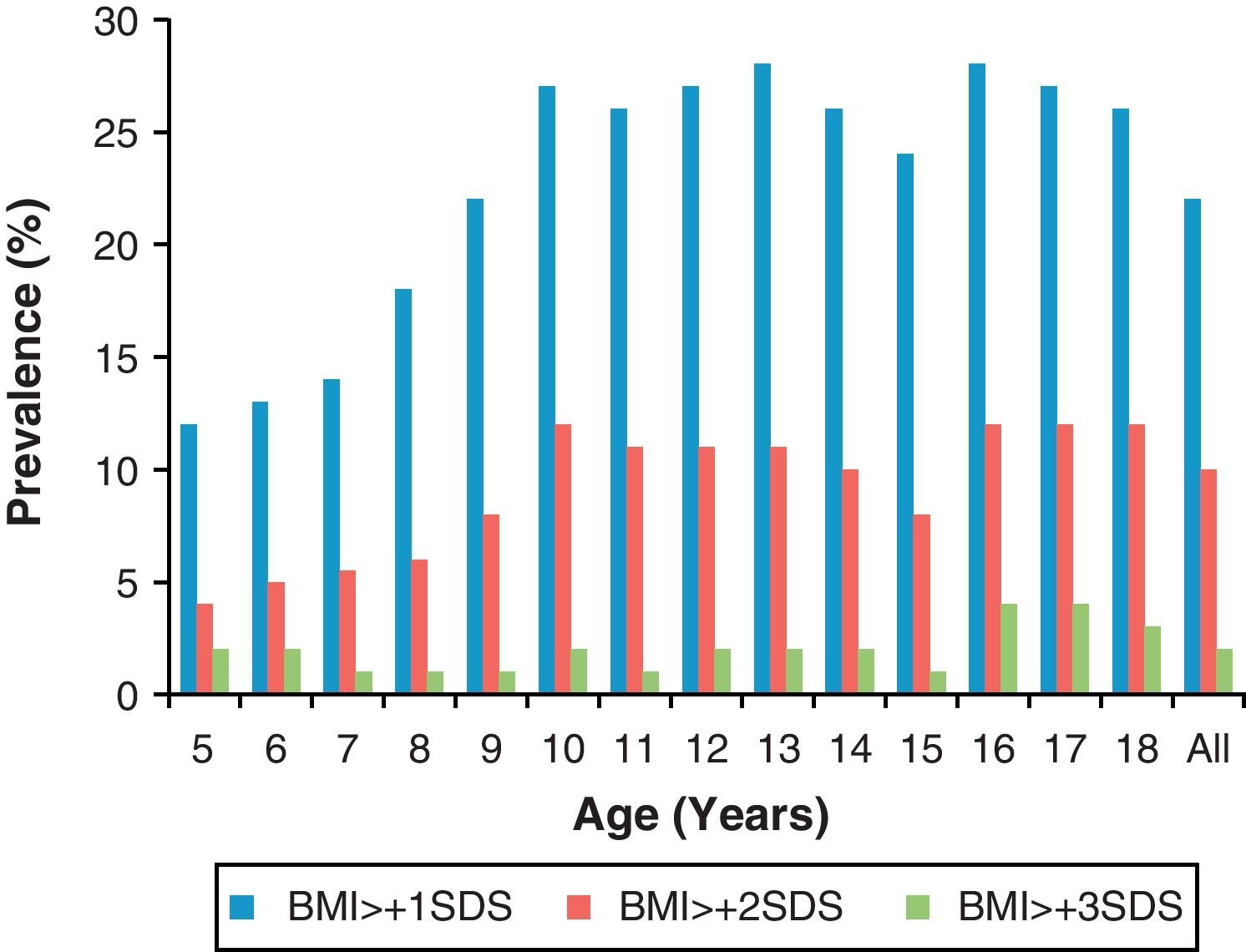
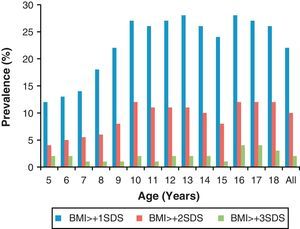
In recent decades, dietary habits have changed rapidly in the Kingdom of Saudi Arabia with the western diet replacing the traditional Arabic diet. This has resulted in an alarming increase in the number of overweight (BMI>+1SD) and obese (BMI>2SD) children and adolescents in the country (Fig. 4). In a study in 2000, including children and adolescents 1–18 years of age, the overall prevalence of overweight was 10.7% and 12.7% and that of obesity was 6% and 6.7% in boys and girls, respectively. Girls had a higher prevalence of both overweight and obesity compared to boys, and both tend to increase with age.20
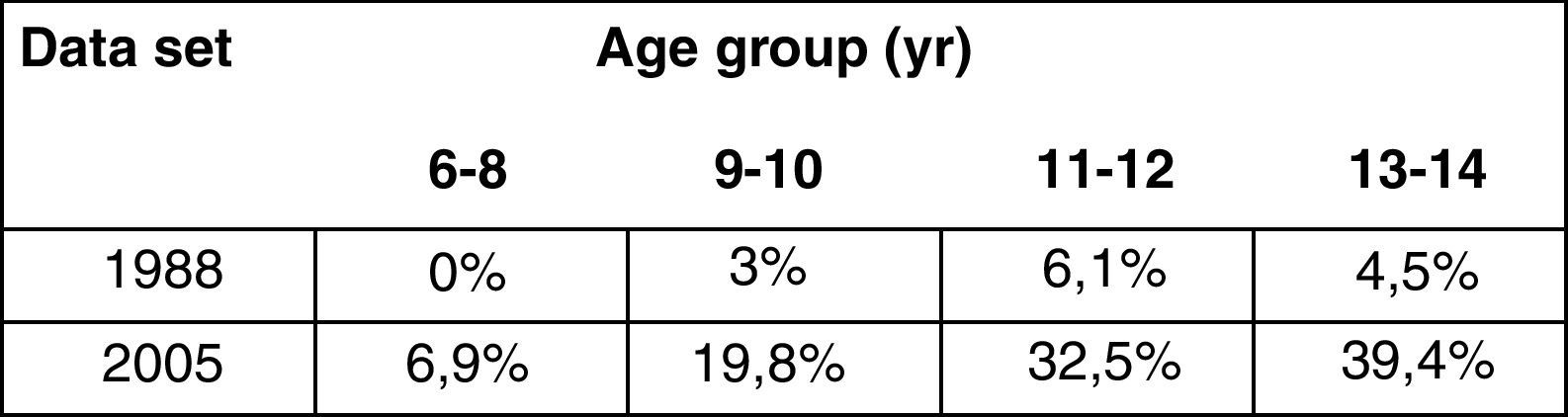
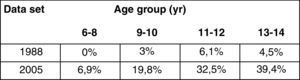
AlHazza21 analyzed the trends in obesity among school boys in central Saudi between 1988 and 2005. There was a significant increase in BMI SD, % of fat and a significant increase in the proportion of obese school boys (Fig. 5). In a study on female school children (8–12 years of age), 14.9% were found to be obese, based on BMI for age.22 In the older age group (10–19 year old), the overall prevalence of overweight and obesity was 12.2 and 27% respectively, with boys having higher obesity rates than girls.23 A significant association was found between male BMI and the consumption of sugar-sweetened beverages and fast food meals as well as total sugar intake. Using both the 2007 WHO and the 2000 CDC reference, the overall prevalence of overweight and obesity in all ages was 23.1%, 9.3% respectively. A significantly lower prevalence of overweight (20.4%) and obesity (5.7%) was found when the CDC reference was used.22
Since the discovery and exportation of oil in 1968, the United Arab Emirates (UAE), has experienced rapid urbanization and dramatic improvement in living condition. This has led to the adoption of new lifestyles, behavioral patterns and food consumption habits.24 The transition affected urban dwellers who gradually replaced their traditional eating habits with more imported, processed food including carbonated drinks and fast food together with the adoption of more sedentary life style. In a cross-sectional study involving 14-year-old adolescents,25 the prevalence of overweight was 18.5% in males and 13.1% females, and obesity was in 22.2% males and 20.5% females. In a national study in the UAE,26 it was found that in the pre-adolescence group, obesity rates were similar to levels observed in other developed countries (5%). However, by 18 years of age, obesity is approximately 3-fold greater. More recent data using BMI and skin fold thickness in a group of 13–17 year-old school adolescents showed that the prevalence of obesity and overweight was respectively 9.9% and 15.1% in females and 6.1% and 14.1% in males.27
Metabolic syndrome (MS) and T2DMThere is still no clear definition, as is the case in obesity, for metabolic syndrome in childhood and adolescence. Some of the studies28 have used three factors (BMI/insulin/lipids); others29 have used the adiposity factor, the carbohydrate factor and the carbohydrate/metabolic factor. Overall, the findings support that metabolic syndrome represent several intercorrelated entities rather than a single syndrome.
Studies on the prevalence of MS among the young in the gulf area are lacking, except for few center-based reports. In a study in the UAE, 260 children with BMI>95th percentile were screened for MS based on Cook's modified criteria. 24.2% had one criterion, 31.8% had 2 criteria and 44% qualified for the diagnosis of MS. The rate of MS was significantly higher among boys than girls (p=0.001), and there was a significant association between the occurrence of the syndrome and BMI (p=0.048).30 In another study from KSA, 29.7% met the diagnosis of the MS, based on the WHO criteria modified for children, and the NCEP-ATP III criteria.31 In the same repot, 26.3% had impaired fasting glucose, and 36% had fasting hyperinsulinemia. In a recent study in Kuwait, two different criteria were used to assess the prevalence of metabolic syndrome among a cross-sectional random sample of adolescent females aged 10–19 years. The IDF criteria gave a value of 14.8% in comparison to 9.1% using the ATP III criteria. No cases of type 2 diabetes or impaired fasting glucose were identified.32 No data were available for the prevalence of metabolic syndrome or type 2 diabetes in other gulf countries.
In a study on the prevalence of type 2 diabetes among 6–18 year-old Kuwaiti children and adolescents, the overall prevalence was 34.9 per 100,000. It was more common in boys (47.3% vs. 26.3%). A positive family history of diabetes was present in 51%, and there was a significant trend for an increase in the prevalence of type 2 diabetes with age.33
Etiologies and possible solutionsAlthough factors such as family history, sedentary lifestyle, urbanization, increased income and family diet patterns have been linked to the increased prevalence of overweight and obesity in the Gulf6–10,12,15 it is apparent that the main underlying cause may be poor knowledge about food choices and lack of physical activity.34 Moreover, there is still widespread perception among parents and their children, at least in some of the countries that overweight is a sign of high social class, beauty, fertility and prosperity.35 Owning TVs, satellite dishes and cars are considered to be markers of financial progress, contributing to significant physical inactivity. In some countries (like KSA), the social and cultural factors, especially on females, have limited their access to sports and leisure time exercise, and socialization frequently involves eating.
In May 2004, the 57th World Health Assembly (WHA) endorsed the World Health Organization (WHO) Global Strategy on Diet, Physical Activity and Health. It addressed two of the main risk factors for non-communicable diseases (obesity being an example), namely diet and physical activity.36 These two factors are closely related to five main factors which contribute to the morbidity and mortality of non-communicable diseases; high blood pressure, elevated levels of serum cholesterol, inadequate intake of fruits and vegetables, overweight and physical inactivity.
In schools, physical activity classes are frequently replaced by other, so called “more valuable and useful” classes, such as math and science. In addition, snacks provided at school, are not supervised by health authorities. They are usually of high fat and sugar content, and most children prefer to have them than take healthy alternatives from home. One unique factor for families in the Gulf region, and some other Arab nations, is that all activities involved in the preparation of food and home chores are lacking as it is usually performed by domestic servants.37
Governments and community organizations should cooperate to create an environment that encourage behavior changes in individuals, and help to maintain it. Economic, demographic and social factors should be considered when establishing programs targeting overweight and physical inactivity.36 The first task is to determine national prevalence for overweight and obesity in each nation. There is an urgent need for longitudinal data and to follow children overtime, to track growth and the incidence of overweight and obesity overtime. Available data suggest that simple anthropometric measurements done yearly at school entrance can help to identify children at risk to ensure that appropriate preventive measures be taken before onset.
Education regarding social and cultural norms and attitudes toward weight in some countries, where rich high-fat food plays an important role in daily diet, and “overweight” is considered a sign of beauty.34 Increasing the overall awareness and understanding of the influence of diet and physical activity on health and the positive impact of preventive measures.36 Physical activity of moderate-intensity at least 30min, three to five times per week, reduces the risk of cardiovascular diseases, T2DM and colon and breast cancer.34,36 In schools, physical activity classes should be an important part of the curriculum, at least 1h every alternate day.35
In rapid urbanization, children skip breakfast and get alternatives from schools. With working parents, sometimes, not even a single meal is shared by the family.
School settings should include healthy foods and snacks monitored or, if possible, provided by health authorities, avoiding financial profit as the main outcome. Classes or seminars on health and diet education should be added. A number of studies have found an association between obesity and frequent snacking, low fruit and vegetable intake and lack of activity among school children. The WHO Strategy for Diet recommendations include achieving energy balance and a healthy weight, limiting energy intake from total fat and shifting toward the elimination of trans-fatty acids, limiting the consumption of salt from all sources, decreasing the intake of sugar and increasing the consumption of fruits, vegetables, whole grains and nuts in the diet.36 One fact to mention is that health official, i.e. the people concerned with obesity and its effect on health tend to have little power within the system of governments to implicit changes needed to break the epidemic.
Children still visit the doctors when they are thin or underweight. There is no awareness of obesity being more than just a cosmetic problem.37 There is a need for the awareness that adipose tissue is an important endocrine system and a source of inflammatory cytokines that can give rise to chronic diseases. Community based intervention programs38,39 have been tried, and initial results are promising. Political and different governmental parties need to participate in any program for it to start and continue, especially in countries with political systems like those in most Gulf nations.
Health ministries have a major and significant responsibility in coordinating and facilitating the contributions of other ministries and governmental agencies. They need to engage all sectors, including civil societies and the media to develop and implement national and community policies to improve dietary habits and physical. Other ministries need to monitor scientific data, support research, and provide accurate food labeling and accurate information of the content of different food items to help consumers make healthy choices36.
Changes in patters of eating and physical activity will be gradual, however, changes in the risk factors and incidence of non-communicable diseases can occur rapidly when effective measures are implemented. Therefore, any plan should have short and intermediate goals.
In conclusion, obesity imposes an increased risk of associated diseases such as metabolic syndrome, coronary heart disease, T2DM and hypertension. There is an alarming increase in the prevalence of overweight and obesity (including morbid obesity) among children and adolescents in the Arabian Gulf region. Schools, preschools and child care settings have all been identified as the main setting for population-based obesity prevention programs, given their important role in promoting healthy eating and physical activity in children. Community and family awareness about obesity being more than a cosmetic problem, is another important area that needs improvement in most of the Gulf nations. All governmental parties, as well as community agencies need to work together to establish long-term programs to improve health education and population attitude toward overweight, obesity and healthy eating. Parallel to the implementation of prevention programs, screening for T2DM and other obesity related complications, such as hyperlipidemia, hypertension and liver steatosis should be implemented in obese children and adolescents to prevent further complications, mainly coronary artery disease.
Conflict of interestThe authors declare no conflict of interest.