1. Introduction
We present the case of a 9 year 4-month-old female patient with a diagnosis of acute lymphoblastic leukemia (ALL). She arrived at the emergency department with fever, vomiting and bowel movements decreased in consistency.
1.1. Family history
The patient's mother is a 48-year-old housewife diagnosed with hypertension at age 40 and treated with captopril. The patient's father lives outside the family nucleus. There are two healthy brothers aged 26 and 24 years. Maternal grandparents have a history of type 2 diabetes mellitus.
1.2. Social history
The patient is a native of and resident of the Federal District (Mexico City). The family is of low socioeconomic status. There are all domiciliary services in the home. The patient was exclusively breastfed until 2 months of age and was integrated into the family diet at 7 months of age. The patient demonstrated apparently normal psychomotor development and attended school until first grade. Immunizations were complete for age.
1.3. Perinatal and medical history
The patient was the product of a third gestation with prenatal control from the first month of gestation with placenta previa and retroplacental hematoma. Birth was by cesarean section at 40 weeks gestation with a birth weight of 3 kg. The patient had recurrent lower urinary tract infections and urethral stenosis diagnosed at 3 years of age.
1.4. Current condition
November 2007. The patient presented for the first time to the emergency department of this institution due to fever and abdominal distension of 3 months duration.
Physical examination revealed petechiae, ecchymoses on the extremities, 10 × 11 × 11 cm hepatomegaly and the lower pole of the spleen at 10 cm from the costal margin. The patient had a holosystolic murmur of 2/6 in intensity that was audible in the four apices. In the bone marrow aspirate (BMA) there were 99% of 12 blasts with pre-B immunophenotype observed. There were no blasts observed in the cerebrospinal fluid (CSF). Chemotherapy with vincristine, daunorubicin, L -asparaginase and dexamethasone was begun.
December 2007. The patient was admitted due to fever of up to 38.9°C, cramping abdominal pain of 2 days duration, and green fetid decreased bowel movements of 24 h duration without mucous or blood. Computed tomography (CT) of the abdomen showed thickening of the walls of the bowel loops and distended loops of bowel in the left lower flank. The bladder was distended with urine, without intraperitoneal collections or data of neutropenic colitis. The patient was discharged with intensification of chemotherapy with etoposide and cytarabine in addition to antibiotic treatment with amoxicillin.
February 2008 to February 2009. The patient continued with consolidation chemotherapy with high-dose methotrexate (five cycles), intrathecal chemotherapy and maintenance scheme for standard risk leukemia.
June 2008. The patient presented urinary symptoms. Urine culture and urinary tract ultrasound showed no abnormalities.
July 2008-October 2009. The patient was admitted on five occasions due to complications of leukemia and its treatment: one for fever of possible urinary origin that was unconfirmed, one for epistaxis, and two for oral and perianal mucositis. During the fourth admission, the patient had a systemic inflammatory response and probably neutropenic colitis, which was managed with meropenem.
August 2009. The patient was admitted for fever and vomiting with serum amylase of 374 U and serum lipase of 430 U, which was managed with cefepime and amikacin.
November 2009. The patient experienced the first CNS relapse: BMA in M1. The patient was started on induction therapy with vincristine, daunorubicin, cyclophosphamide, L-asparaginase and dexamethasone.
November-December 2009. The patient was admitted to the emergency department due to intense retrosternal pain, vomiting and fever up to 39°C. On endoscopy, esophagitis due to Candida sp. was noted and was managed with amphotericin B. CT of the paranasal sinuses demonstrated left ethmoidal, maxillary and sphenoidal sinusitis. Klebsiella sp. was isolated in a peripheral blood culture for which cefepime, amikacin and meropenem were indicated and amphotericin was changed for caspofungin. Thoracoabdominal CT demonstrated right apical consolidation, pleural effusion, thickening of the esophageal mucosa and of the ascending colon. The patient required red blood cells and platelet transfusions. Because of reappearance of fever and isolation of positive cocci in the urine, vancomycin was added.
December 2009-March 2010. Cerebrospinal fluid (CSF) was free of blasts. Three phases of consolidation chemotherapy were administered with methotrexate and rescue with folinic acid. Radiotherapy at a dose of 24 Gy in the brain and 10 Gy in the spinal canal was given.
July-August 2010. The patient was admitted due to fever associated with perianal cellulitis, pulmonary congestion and hepatomegaly. CT scan of the chest showed pulmonary lesions compatible with Aspergillus sp., which was managed with amphotericin B. Echocardiogram showed an ejection fraction of 82%.
October 2010. The patient was hospitalized for fever and managed with cefepime and amikacin. Erythema of the left ear lobe was added with insidious, progressive bone pain, triggered by administration of vincristine. Staphylococcus aureus was isolated from the ear lobe and Listeria monocytogenes from the blood culture. The patient was given a 25-week chemotherapy maintenance scheme for high-risk ALL with vincristine, L-asparaginase and dexamethasone. The last dose was received during January 2011.
January 21, 2011. The patient presented with progressive sudden fever of 38.3°C with con piloerection, without chills or diaphoresis. She vomited on two occasions and had bowel movements of liquid consistency. On physical examination the patient was found to be pale, dehydrated, chest with vesicular murmur with no added breath sounds, precordium with decreased sounds in intensity, without aggregates, abdomen soft with decreased peristalsis, thick green vaginal secretions, and weak distal pulses. Two boluses of crystalloids (20 ml/kg/dose), oxygen and meropenem (100 mg/kg/day) were added. The patient had a cardiac arrest. Resuscitation maneuvers were provided for 20 min with five boluses of adrenaline, dobutamine and calcium gluconate without response.
2. Case presentation
2.1. Coordinator (Dr. Aurora Medina Sansón)
The case of a patient with a diagnosis of ALL is presented, which illustrates a death in remission despite having obtained a good response. The patient presented CNS relapses.
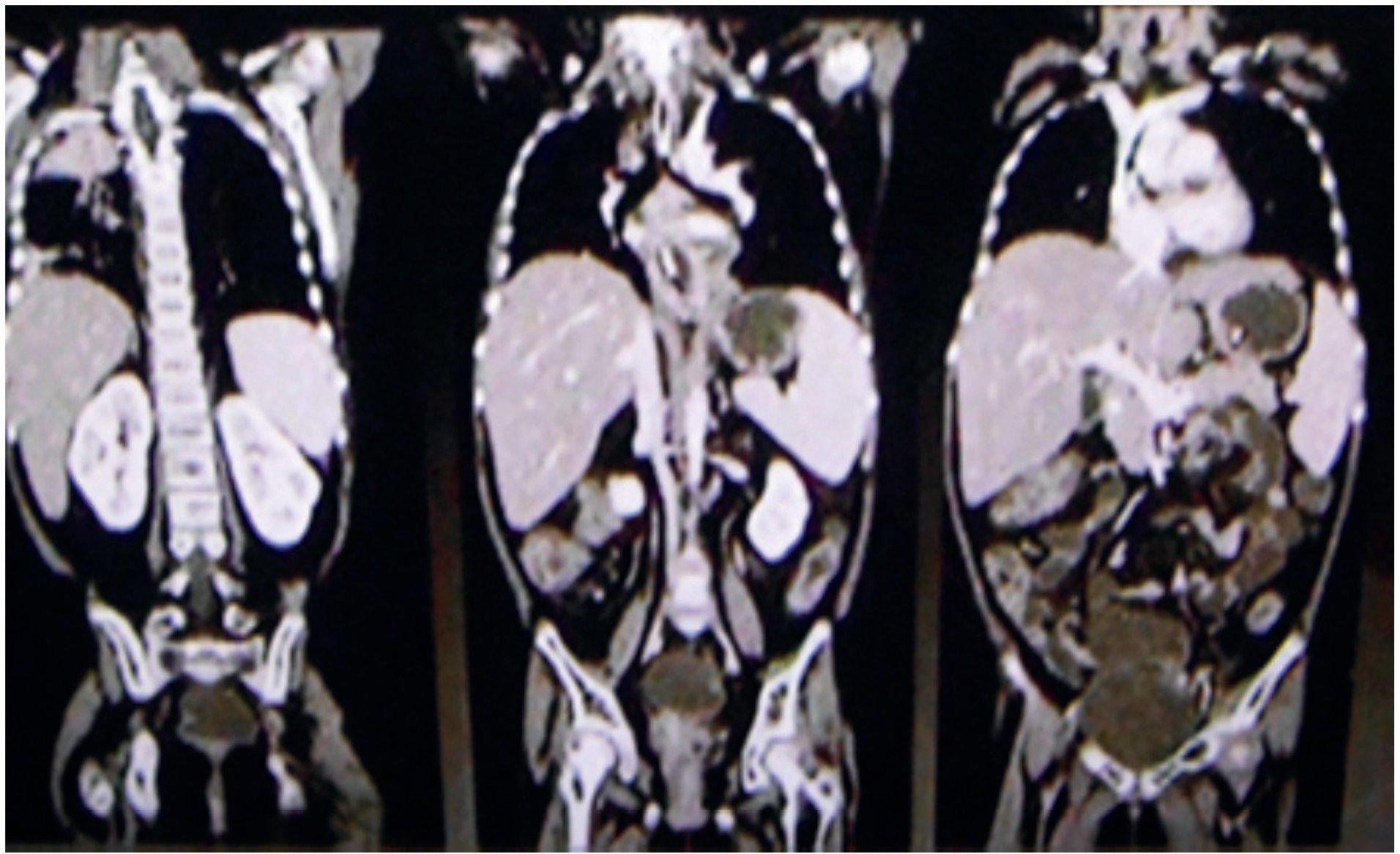
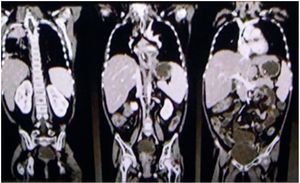
2.2. Imaging (Dr. Pilar Dies Suárez)
In 2009, a deep focus CT was performed. This radiological study explores from the paranasal bones up to the pelvic space, attempting to detect any infectious foci. This patient presented with thickening of the left maxillary sinus mucosa and of the osteomeatal complex. The patient had right-side apical pulmonary consolidation and areas of bilateral interstitial thickening, predominantly of the right side. The patient presented no changes in the abdominal region (Fig. 1). There was no significant radiological finding in the remainder of the radiological studies.
Figure 1. Thoraco-abdominal tomography.
When requesting imaging studies, we must always consider the radiation dose received by the patient. The dose of radiation from a deep focus CT scan is roughly equivalent to 300 plain x-rays. In conclusion, the only finding was thickening of the mucosa and lung consolidation that can be seen with a simple x-ray and found on auscultation (Fig. 1).
2.3. Discussion (Dr. Elianneth Rey Helo)
Syndromatic diagnoses were as follows:
• Infiltrative syndrome: lymphadenopathy, hepatomegaly and splenomegaly
• Anemic syndrome: pallor, systolic murmur II/VI and Hbg 9.1 g/dl
• Hemorrhagic disease syndrome: petechiae, ecchymosis of the extremities and platelet count of 71,000
• Infectious syndrome: fever, urinary, ear, pulmonary and abdominal symptomatology
Nosological diagnoses are as follows:
• Normal risk ALL due to the presence of an infiltrative, anemic and hemorrhagic syndrome, bone marrow aspirate with 99% blasts, age within 1 to 10 years, B-cell precursors and response to remission induction
• Recurrent urinary tract infection due to the presence of proteinuria, pyuria, microhematuria on urinalysis, presence of Escherichia coli in two urine cultures and urethral stricture
• Neutropenic colitis due to the presence of profound neutropenia, absolute neutrophil of 100/mm3, stools decreased in consistency and vomiting
ALL is the most common form of cancer in children. It constitutes 30-34% of all diagnosed cases of cancer. Of these, 80% correspond to ALL and the remaining 20% to acute myeloid leukemia (AML).
In the evolution of children with ALL, fever is an event that occurs in 80%, as was the case in the multiple hospitalizations in this patient. The events of fever were associated with neutropenia and on various occasions there was evidence of infectious foci (aural, pulmonary and gastrointestinal, GI). The events of fever and neutropenia presented by the patient were categorized as high risk because of profound neutropenia lasting >7 days and hemodynamic instability and GI symptoms characterized by vomiting and diarrhea. Although the clinical criteria for neutropenic colitis are not well established, one study found that diarrhea and associated hypotension were the most common symptoms in patients with this condition. The patient in the present case presented these symptoms coupled with fever and profound neutropenia <100/mm3.
Treatment of ALL is carried out in three stages as follows:
• Induction of remission
• Consolidation phase
• Maintenance phase
With this treatment scheme, 80-85% of patients have a prolonged remission and cure, and 20% may present isolated remission to the bone marrow or extramedullary sites. In this case, the patient had a central nervous system relapse during the maintenance phase. For this reason she required craniospinal radiotherapy and chemotherapy with vincristine, L-asparaginase and dexamethasone. The erythema in the left ear lobe was attributed to an allergic reaction to vincristine, which was ruled out because this is not an adverse effect described for such an alkaloid. Rather, it is believed that it was a cellulitis due to Staphylococcus aureus.
Mention is made in the clinical history of symptoms of lower urinary tract infection and a diagnosis of urethral stenosis at 3 years of age. This is a rare condition in females and is diagnosed by urethrography. The etiology of urethral stricture is unknown in most cases. During the pediatric age, recurrent urinary tract infections cause the presence of stenotic urethral rings plus urethral musculature decreases in thickness at its distal part, incorporating connective tissue fibers until they disappear.
During the patient's last admission, she presented a rapidly evolving acute infectious gastroenteritis with severe dehydration, which ended up in a mixed, hypovolemic and cold septic shock refractory to amines, characterized by the presence of tachycardia, tachypnea, hypotension, prolonged capillary refill, weak pulses, decompensated metabolic acidosis, hyperlactatemia of 9.7. There was no improvement after administration of two boluses with saline and administration of adrenaline, dobutamine and meropenem. A true hypovolemic hyponatremia was documented with serum sodium of 125 mEq/l, which was most likely triggered by GI losses secondary to vomiting and diarrhea. Addressing this type of hyponatremia requires knowledge of the serum and urine osmolality and urinary electrolytes, which were not provided in the medical record.
Mixed refractory shock to amines conditioned multiple organ failure (MOF), which is classified as primary and which presented itself in the first 7 days of onset. The diagnosis of MOF in this patient is comprised by the following data:
1) Cardiovascular impairment, mean arterial pressure <5th percentile for age and need for vasopressor agents after cardiovascular resuscitation.
2) Hematologic dysfunction with decrease of the three cell series, Hbg 10.6 g/dl, WBC 500/mm3, total neutrophils 100/mm3, platelets 83,000/mm3, prothrombin time 16.2 sec, partial thromboplastin time >130 sec.
3) Renal dysfunction with creatinine 1.7 mg/dl.
4) Hepatic dysfunction with alanine aminotransferase >100 IU/L and total bilirubin 1 g/dl.
With these data, the organ failure index (OFI) is 4/6 points, indicating 80% risk of death. Observations for the therapeutic management of this event are that it was a patient receiving dexamethasone and refractory septic shock to amines who required the administration of stress doses of hydrocortisone.
The final diagnoses are mentioned below:
• ALL L2, with a history of relapse isolated to the central nervous system in the maintenance phase
• Urethral stricture secondary to recurrent urinary tract infection
• Genital infection, probably vulvovaginitis
• Probable neutropenic colitis
• Mixed septic shock refractory to amines
• Multiple organ failure
2.3.1. Cause of death
Mixed shock refractory to amines and multiple organ failure.1-11
2.4. Department of Evaluation and Drug Analysis (Dr. Luis Jasso Gutiérrez)
Although they are expected effects, neutropenic colitis and mucocytosis are adverse reactions associated with chemotherapy and, as such, should be reported to the Department of Evaluation and Drug Analysis.
2.5. Nephrology (Dr. Ricardo Muñoz Arizpe)
I am not convinced that the patient had a urethral stricture because, as mentioned, it is very rare in females. In addition, the necessary urological studies were not carried out. If infections were confirmed in the institution, a cystoscopy and urodynamic studies could have been done, plus urethrocystography in order to detect bladder dyssynergia. This should be done in any patient with these symptoms or with this history, especially in an immunocompromised child because infectious foci are life threatening.
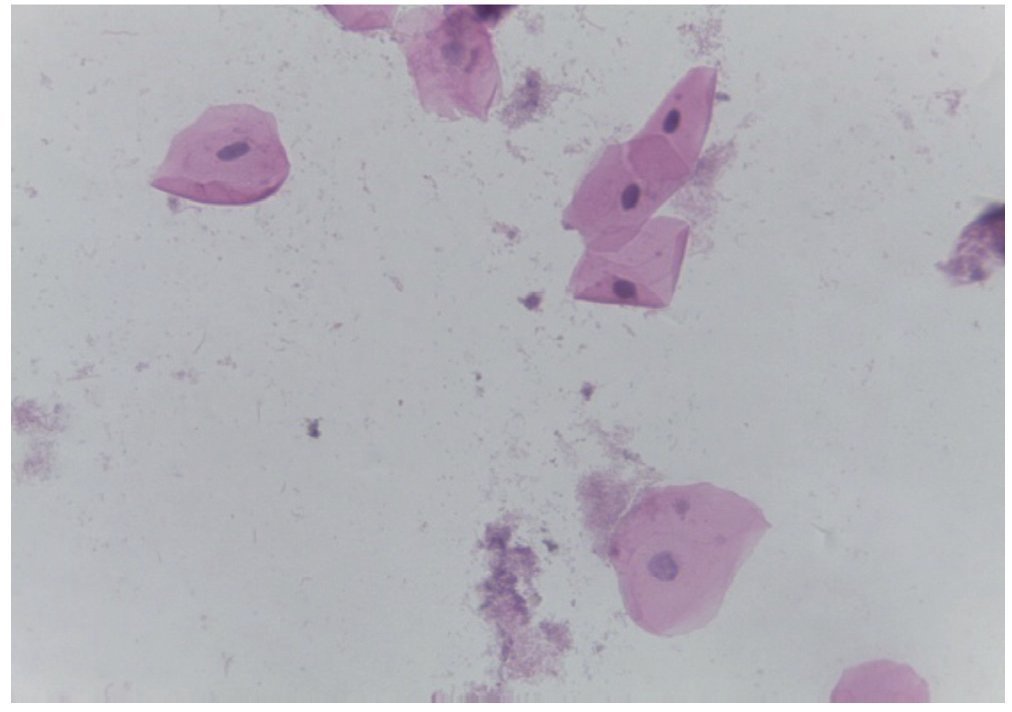
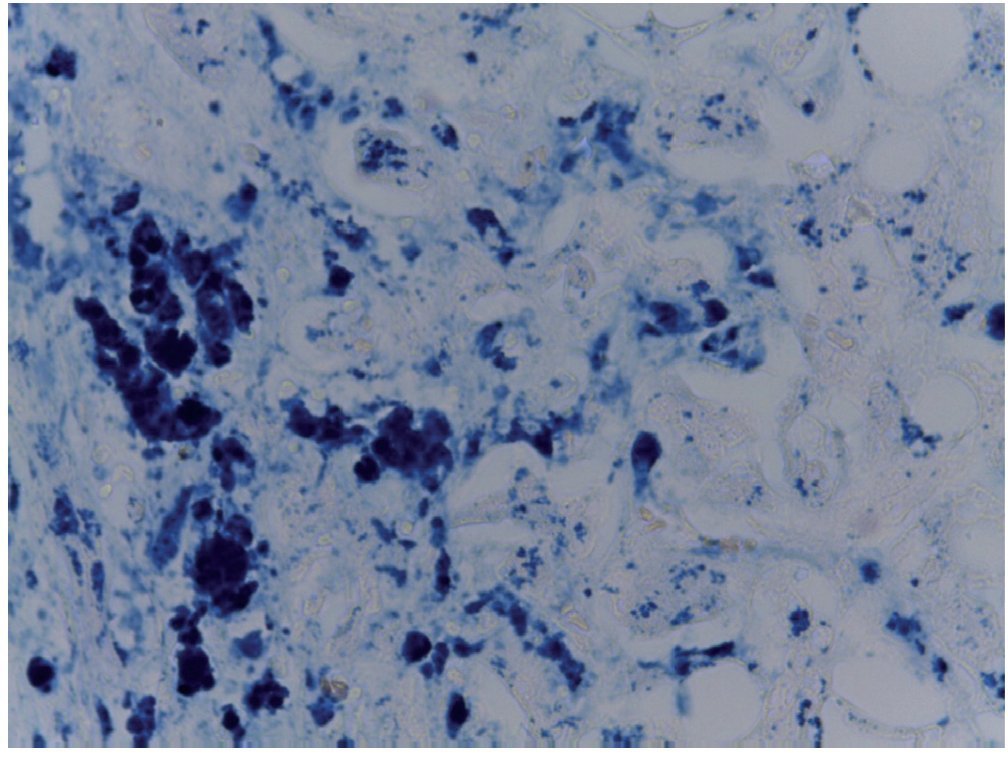
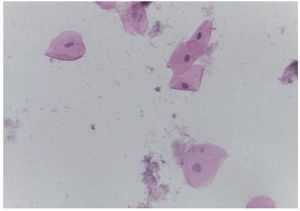
2.6. Pathology (Dr. María Sánchez Escobar Algeria)
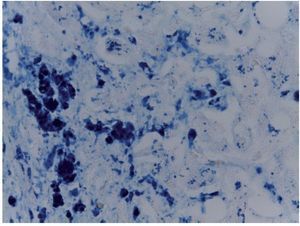
Cytology of oral mucosa (premortem). Epithelial cells do not exhibit cytopathic changes and no viral inclusions. There were no fungi (Fig. 2) observed. Diagnoses made at that time were as follows:
Figure 2. Cytology of the oral cavity (H/E 20X). Epithelial cells without alterations. Negative for fungus and viral inclusions.
• C-08-06. Inadequate material for diagnosis
• C-09-225. Negative for viral and fungal inclusions
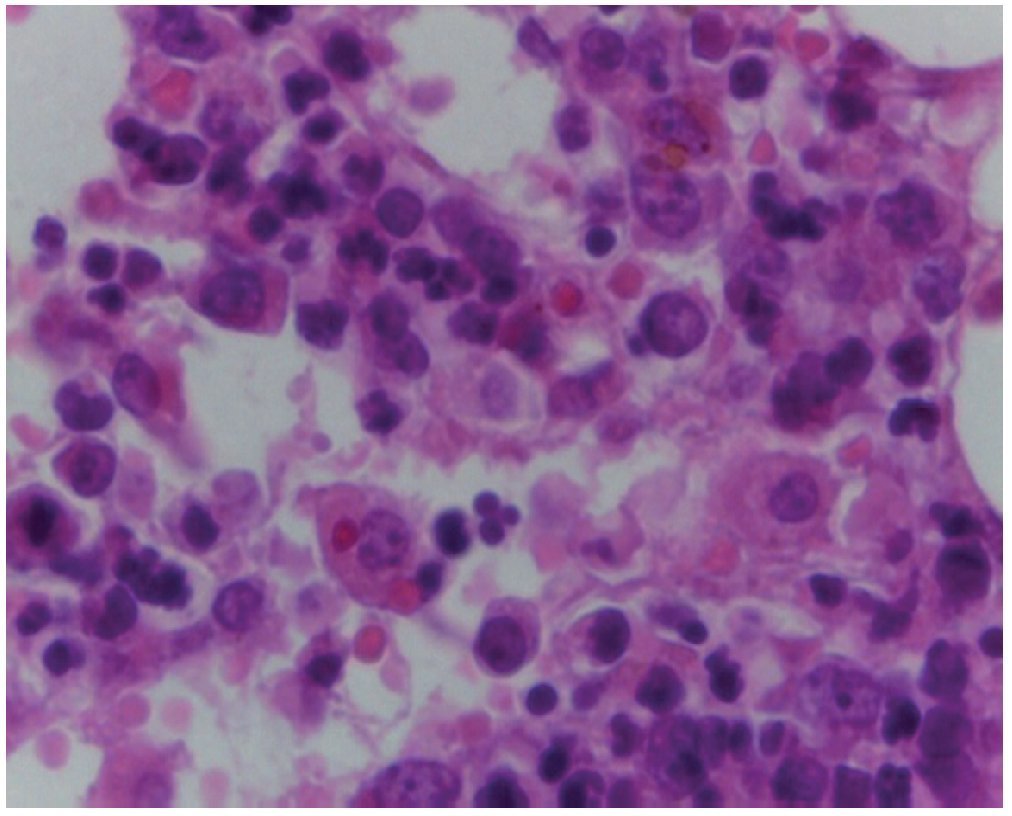
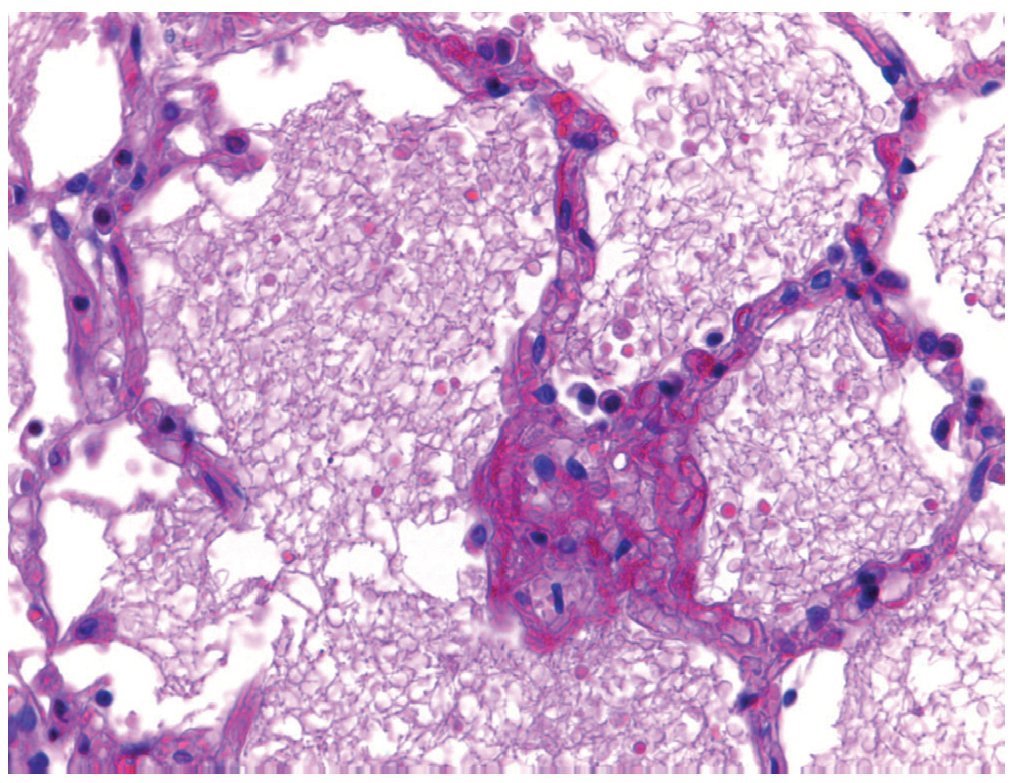
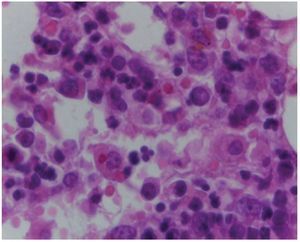
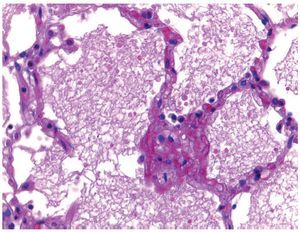
Bone marrow. Bone trabeculae were observed lining osteoblasts, and cells were occupied by the three hematopoietic series. The ratio of bone marrow cellularity compared to adipose tissue is 50-60%. When greater increased cellularity is observed, it is appreciated that there are elements mainly of myeloid series with granulocyte maturation up to the bands. The presence of megakaryocytes was also observed and a few erythroid elements. It is noteworthy that there are no blasts present. Another important finding is the recent hemorrhage and hemosiderin deposition. It is important to mention the presence of megakaryocytes as it is the first series that disappears in the presence of leukemia. At this time, the bone is recovered. With a 100× objective we can see the presence of histiocytes with erythrocytes in their cytoplasm. This hemophagocytosis is secondary to a neoplastic process, both the neoplastic process as well the treatment and evolution of this patient (Fig. 3).
Figure 3. Bone marrow with elements of three hematopoietic series, absence of blasts and hemophagocytosis (H/E 100×).
Postmortem diagnoses of bone marrow were as follows:
• Bone marrow in remission without the presence of blasts with presence of hemosiderosis, hemophagocytosis and of the three hematopoietic series with normal maturation.
3. Final diagnoses
Principal disease: Acute ALL in remission.
There were no significant changes in the outer habitus.
The abdominal content was observed to have an important distension of the bowel loops.
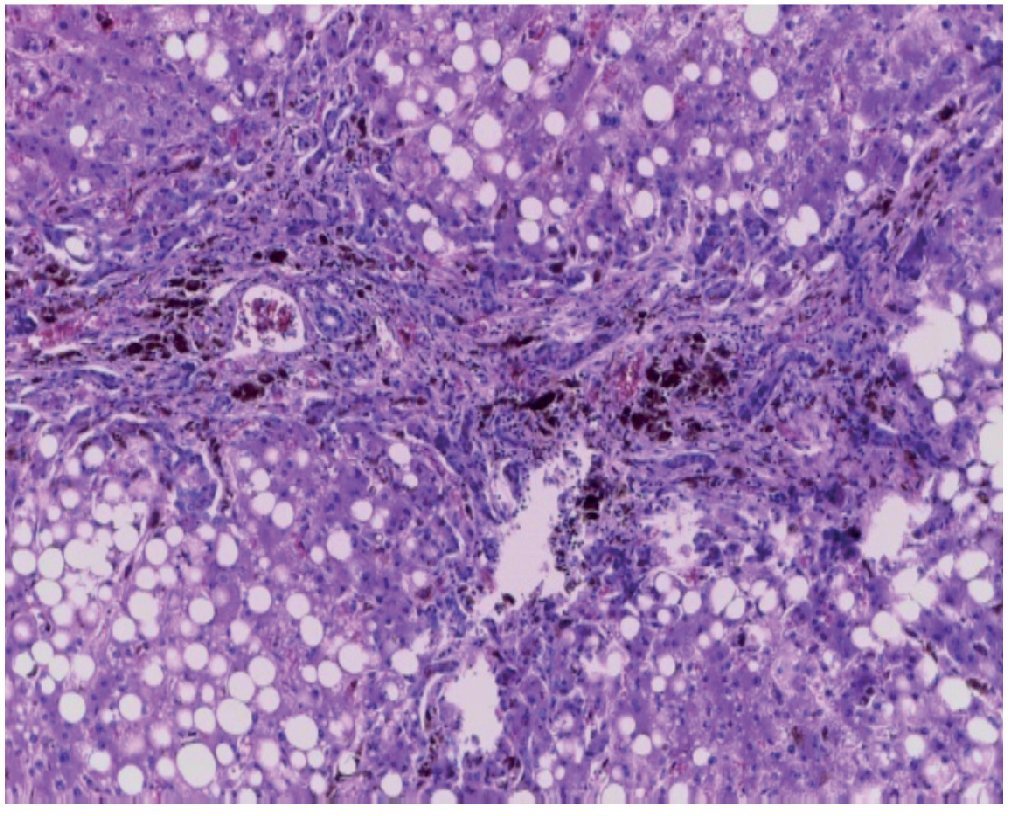
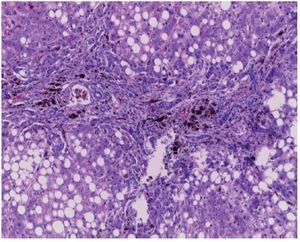
There were 35 mL of blood found in the left hemithorax and 25 mL in the pericardium, as well as a mediastinal hemorrhage. Histological sections of the mediastinum demonstrated adipose tissue with extensive hemorrhage. Remnants of the thymus demonstrated calcified Hassall corpuscles and lymphoid depletion. Continuing with the mediastinum, the heart had a weight of 100 g vs. 115 g expected. What was notable, from a macroscopic point of view, was the petechial hemorrhage in the pericardium, the atrium and the right ventricles. As observed from its posterior face, hemorrhage was demonstrated in the adventitia of the pulmonary artery and there was a subepicardiac hemorrhage of 3 × 2 cm. Histological sections demonstrated cardiomyocytes with vacuolated cytoplasm, some with mild increase in the size of the nucleus. This is important because the patient had received daunorubicin, which is cardiotoxic. However, there are no histological changes secondary to the administration of this drug. The liver had an expected weight of 1600 g vs. an expected weight of 756 g. Macroscopically, a light brown color was seen; many changes were histologically seen such as important changes in the architecture due to the presence of fibrosis mainly at the central venous level. At the level of the portal spaces and central veins many hemosiderophages were observed (Fig. 4). In the lobule, there is macro- and microvesiculars steatosis. These data are important in the lesion due to drugs which, apparently, is what is seen in the liver. The presence of macrovesicular steatosis is secondary to steroids, and the presence of microvesicular steatosis is secondary to the administration of methotrexate and L-asparaginase. Fibrosis, and the damage that we see in the portal spaces, is secondary to the hemosiderin deposit that is so extensive in the patient. There is also intracytoplasmic cholestasis. A Masson stain was done where the presence of fibrotic bridges can be observed, which join the central veins with the portal spaces, data suggestive of an irreversible lesion that most probably would progress to cirrhosis. A greater increase is evident of collagen IV and VI deposits and the important expansion at the level of the portal spaces and central veins. In a Perls stain, specific for demonstrating iron deposits, the presence of hemosiderophages are seen, with distribution in coarse granules in all fields (Fig. 5). This is important because histological grading is done based on this information. This is a grade IV/IV on the Krause scale, with presence of hemosiderin in all fields with coarse granule distribution.
Figure 4. Histological cut of the liver with portal fibrosis, hemosiderophages and panlobular macro- and microvesicular steatosis (H/E 20×).
Figure 5. Staining to observe iron deposition, presenting hemosiderophages in the liver (Perls 40×).
The spleen also had an increased weight of 260 g vs. an expected weight of 73 g. Histologically, congestion of the red pulp was observed, hemosiderin deposition and significant decrease in the lymphoid tissue in the white pulp. In other areas the presence of fibrosis and hemosiderophages that correspond to a passive chronic congestion of the spleen are seen.
Continuing with the mononuclear phagocyte system, the lymph nodes are normal size and what is observed is the depletion of lymphoid tissue. Follicles were not observed. All these changes are secondary to chemotherapy. There was also an extensive hemosiderosis, with numerous hemosiderophages located in the cortical as well as in the medullary sinuses. With these findings, the concomitant changes are listed below.
• Subepicardial hemorrhage of 3 × 2 cm
• Hepatomegaly (1600 g vs. 756 g)
• Macro- and microvesicular panlobular steatosis compatible with drug damage
• Stage III/IV extensive portal fibrosis
• Hemosiderosis Krause grade IV/IV
• Splenomegaly (260 g vs. 73 g)
• Chronic passive congestion
• Hemosiderosis Krause grade IV/IV in lymph nodes and spleen
• Lymphoid depletion
• Hemophagocytosis in lymph nodes and bone marrow
• Acute thymic involution
In two articles, reference is made to the presence of liver damage secondary to hemosiderin in patients who had been treated with multiple transfusions, mainly for ALL. In a study that included 30 liver biopsies, the most significant damage was fibrosis.12,13
The lungs weighed almost double their normal weight. Macroscopically, there were areas of congestion at the level of the basal lobes; histologically, the architecture was preserved. What called the attention was the presence of some areas of atelectasis and intraalveolar edema (Fig. 6). There were also vegetable fibers in the lumen of the bronchioles; however, there was no tissue reaction found and this suggests that the patient probably had episodes of bronchoaspiration. One must remember that the patient was immunocompromised and so did not present a good inflammatory response. However, some foci of inflammatory infiltrate were observed, both in the alveoli as well as in the bronchi and bronchioles. There was no presence of microorganisms, which were intentionally sought; among them, Pneumocystis jirovec.
Figure 6. Pulmonary parenchyma with intraaveolar edema (H/E 40×).
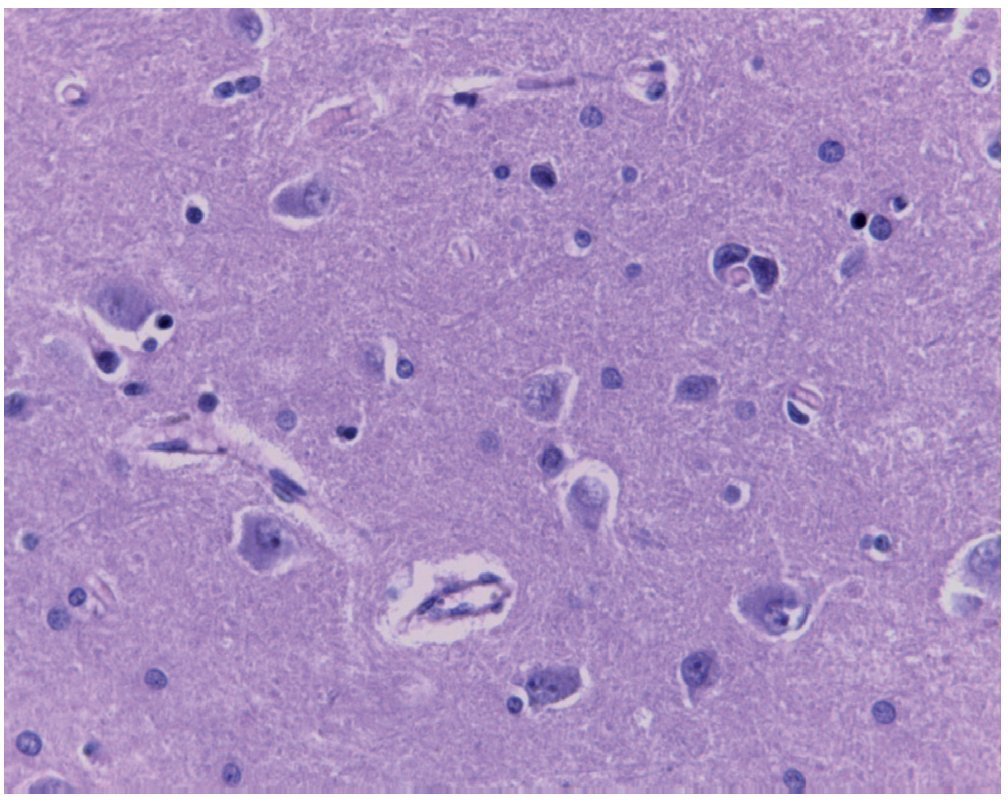
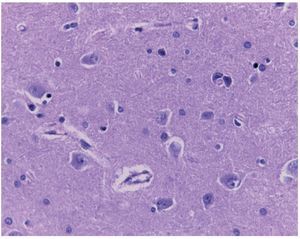
The brain was mildly decreased in weight with respect to what was expected (1150 g vs. 1275 g) and presented significant congestion of the subarachnoid vessels as seen by the convexity and by the base. On serial cuts, a discrete dilatation of the ventricular system was observed. Histological sections demonstrated neuronal hypoxia (Fig. 7). Numerous cuts were evaluated to confirm the presence of blasts both in the subarachnoid vessels as well as in the parenchymal vessels. At that time there was no neoplastic activity at the CNS level or in any other site.
Figure 7. Cut of central nervous system with neuronal hypoxia and absence of neoplastic infiltration (H/E 40×).
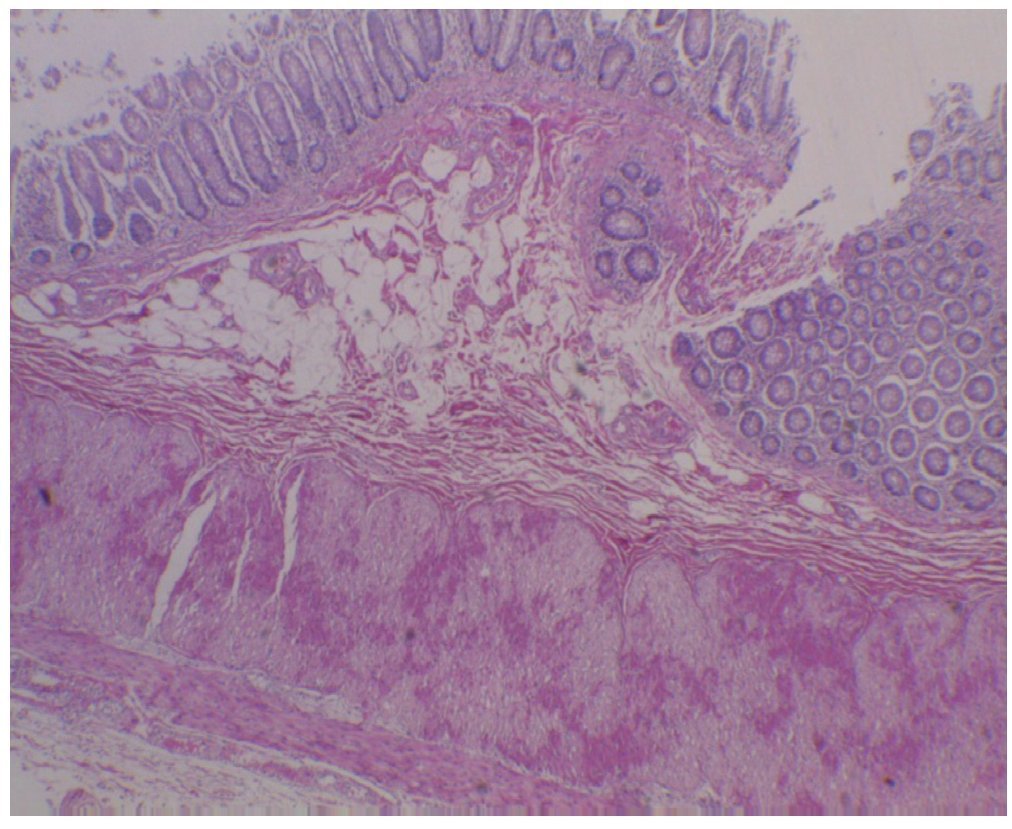
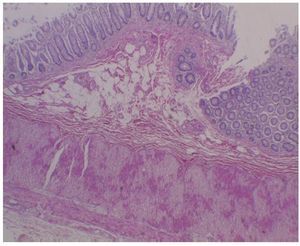
The esophagus presented congestion, especially at the level of the superior third, as did the gastric mucosa, which preserved its folds. Histological sections demonstrated wall integrity with preserved mucosa, submucosal congestion and contraction bands at the level of the muscular wall, secondary to shock. The remainder of the gastrointestinal tract showed the following. In the small intestine a mild flattening of the folds was noted. Microscopically the wall was complete, with only adipose infiltration, most probably because the patient was overweight secondary to the administration of steroids. All the cuts demonstrated whole mucosa, depletion of lymphoid tissue and submucosal congestion. The different segments of the colon demonstrated complete mucosa. It is notable that there is no macroscopic data of neutropenic colitis. There is no presence of necrosis and this is corroborated histologically because the wall and the mucosa are seen to be completely whole. There were only contraction bands seen in the muscular wall secondary to shock (Fig. 8).
Figure 8. Integral colon wall without data of neutropenic colitis. Only observed were contraction bands of the muscle wall secondary to shock (H/E 10×).
In the pancreas, areas of congestion were observed. One must keep in mind that this patient received L-asparaginase, which can cause pancreatitis; however, this patient did not present any histological changes.14 Some ducts were seen that presented mild secretion within their lumen, probably secondary to shock and dehydration. The islets of Langerhans were histologically normal as were the acini.
The kidneys were increased in weight (260 g vs. 165 g). The congestion at the level of the renal medulla is notable; however, the cortex-medulla relationship was preserved. Histologically, congestion was found only at the level of the glomerular capillaries and loss of cortical tubule epithelium, secondary to shock. There are no data of leukemic infiltration or of inflammation or microorganisms.
The clinical history reports that the patient presented with multiple episodes of lower urinary tract infections. The bladder had mucosal edema and significant thickening (∼1 cm thickness) of the muscular wall. However, the bladder urethra was permeable. Histologically, hypertrophy of the bladder wall was observed, but there was no fibrosis and there were no data of infectious processes or recent reactions.15,16 Only observed in the wall was hypertrophy secondary to multiple infectious processes that the patient presented (Fig. 9). The clinical history also described that the patient had vaginal secretions. Macroscopically, the reproductive system (ovaries, uterus and vagina) was without alterations. At the time of the study, a frotis of the vaginal secretion was obtained and only epithelial cells were observed. There was no presence of fungus, viral inclusions or any other microorganisms. The sections that correspond to the uterus showed the ectocervix with integral stratified nonkeratinized squamous epithelium and slight congestion of stromal vessels. The endometrium also did not show histological changes, and the ovaries demonstrated primary follicles and the stroma without changes.
Figure 9. Macroscopic photograph of the bladder with evidence of uretheral stenosis, with hypertrophy of the muscle wall.
The adrenal gland showed congestion of the cortex and medulla. There were no other abnormalities.
With these findings the following comorbid diagnoses were integrated:
• Bilateral bronchopneumonia
• Bilateral intra-alveolar edema
• Cerebral atrophy (1175 g vs. 1250 g)
• Hypertrophy of the bladder wall
• Anatomic data of shock:
— Hypoxic ischemic visceral myopathy
— Acute tubular necrosis
— Multivisceral congestion
Postmortem cultures were as follows:
• Blood culture: Staphylococcus aureus, Staphylococcus epidermidis, Streptococcus viridans
• Right lung: Streptococcus viridans, Streptococcus sp.
• Left lung: Streptococcus viridans, Streptococcus sp., Staphylococcus aureus
• Small intestine: Pseudomonas stutzeri, Shewanella putrefaciens
• Large intestine: three morphotypes of Escherichia coli, Citrobacter youngue, Citrobacter amalonaticus
• Perianal: Escherichia coli, Citrobacter youngue, Citrobacter amalonaticus
• CSF, spleen and liver: negative
It is noteworthy that no infectious or neoplastic activity was found. The patient was probably infected, but there was no gross or microscopic evidence, only the anatomic impact of shock, liver damage due to drugs and liver fibrosis caused by such extensive hemosiderin.
4. Expert commentary
4.1. Oncology (Dr. Miguel Angel Palomo)
Prognosis. There are two important facts: one is the site of relapse and the other is how long the patient was in remission. In this case, the site of relapse was extramedullary in the CNS and the time to relapse was ∼24 months. Accordingly, the possibility of achieving a second remission was almost 95%. Patients with extramedullary relapse after 18 months of maintenance, treated exclusively with chemotherapy, have an overall 5-year survival of 40%. In this case with CNS relapse, the patient did not benefit from the bone marrow transplant.
4.2. Oncology (Dr. Elisa Dorantes Acosta)
Chemotherapy toxicity. There are various factors that affect the pharmacokinetics of chemotherapy such as age, body water distribution and protein bound fraction. This patient was not a newborn and no data of significant malnutrition are present, which would cause hypoalbuminemia.
To evaluate the toxicity of chemotherapy, the WHO scale is used, which ranges from zero to four. Each drug has a degree of toxicity in addition to the interaction among different drugs. Some have dose limitations, for example, those with grade IV toxicity. There are studies at the molecular level on pharmacogenetics and pharmacokinetics where the determination of some genes and polymorphisms may help to consider establishing some doses.
4.3. Urology (Dr. Fernando González Ledón)
Uretheral stenosis and urinary tract infections. When the clinical history is taken, there is sometimes no information to suggest urinary tract infections, and at the time of taking the urine culture the measures are not adequate. It was commented in this case that the urinary tract infections may have triggered vulvovaginitis, but it is not so. On the contrary, the cause of the infections is the ascent of the bacteria from the vulva and the anus. It must be made clear that the vesicoureteral reflux is not the cause of the urinary tract infections. The cause is that the bacteria enters the bladder, and the majority of these bacterias will manifest themselves, if there is no reflux, with symptoms of the lower urinary tract such as cystitis, urethritis or simply meatitis. The repeated meatitis is what could cause stenosis, but not in the female urethra. It is simply a loss of the elasticity of the meatus, which will behave as obstructive. The female urethra is a muscular tube that lacks the spongy body, for which it is almost impossible to have stenosis. In cases where this is suspected, it is necessary to perform a micturation urethrocystogram to observe these characteristics. In the case of the thickening of the vagina, the first suspicion is a neurological problem or in patients with micturition disorders who have advanced symptoms and who do not receive treatment, they may have hypertrophy of the bladder. In regard to the prevention of urinary tract infections, 80% of girls who come for the first time for urological consultation have vulvovaginitis characterized by erythema and burning, which is a risk factor for bacterial colonization and urinary tract infections. For this reason, patients must be taught to urinate, especially those with risk factors and with immunocompromise that could favor recurrent infections.
4.4. Infectious diseases (Dr. Servelio Moreno Espinosa)
Microbial sensitivity to nitrofurantoin. It is necessary to take into account the susceptibility of the germ, the action mechanism of the antibiotic and the state of immunocompetency in patients with these characteristics. In lower urinary tract infections, nitrofurantoin is a very stable drug. Despite its wide use, a collection of studies from 32 federal entities report a resistance of 15%. It is considered that a resistance of <20% for a drug is adequate, so its use is considered to be appropriate.
Listeriosis. As for Listeria monocytogenes, isolation is more common in lupus patients than in patients immunocompromised by chemotherapy. It follows that when the blood culture was isolated from this patient, she was already on antibiotic treatment. Although the treatment of choice should be ampicillin, this patient was being treated with vancomycin. Although that is not the treatment of choice, it is effective. The patient had also progressed well, so it was not necessary to administer ampicillin.
4.5. Hemat ology (Dr. Mariana Revueltas)
Hemosiderosis. In several studies it has been observed that there is a cumulative transfusion dose as a risk factor of 120 ml/kg. In the hospital, we analyzed 85 cancer patients who had been multitransfused. They were grouped according to <10 transfusions, 10-15 transfusions and >20 transfusions. Some patients had liver failure. It is very important to consider the number of transfusions and to assess ferritin levels.
Conflict of interest
The authors declare no conflict of interest of any nature.
Received 31 January 2014;
accepted 6 February 2014
* Corresponding author.
E-mail:bcnhim20091@hotmail.com (M.A. Escobar-Sánchez).