En la práctica médica pediátrica es frecuente encontrar a pacientes en circunstancias que representan un dilema ético para los profesionales de la salud. Un dilema corresponde a una situación en la que los preceptos morales o las obligaciones de similar obligatoriedad ética se encuentran en conflicto, de forma que cualquier solución posible al dilema es moralmente intolerable.
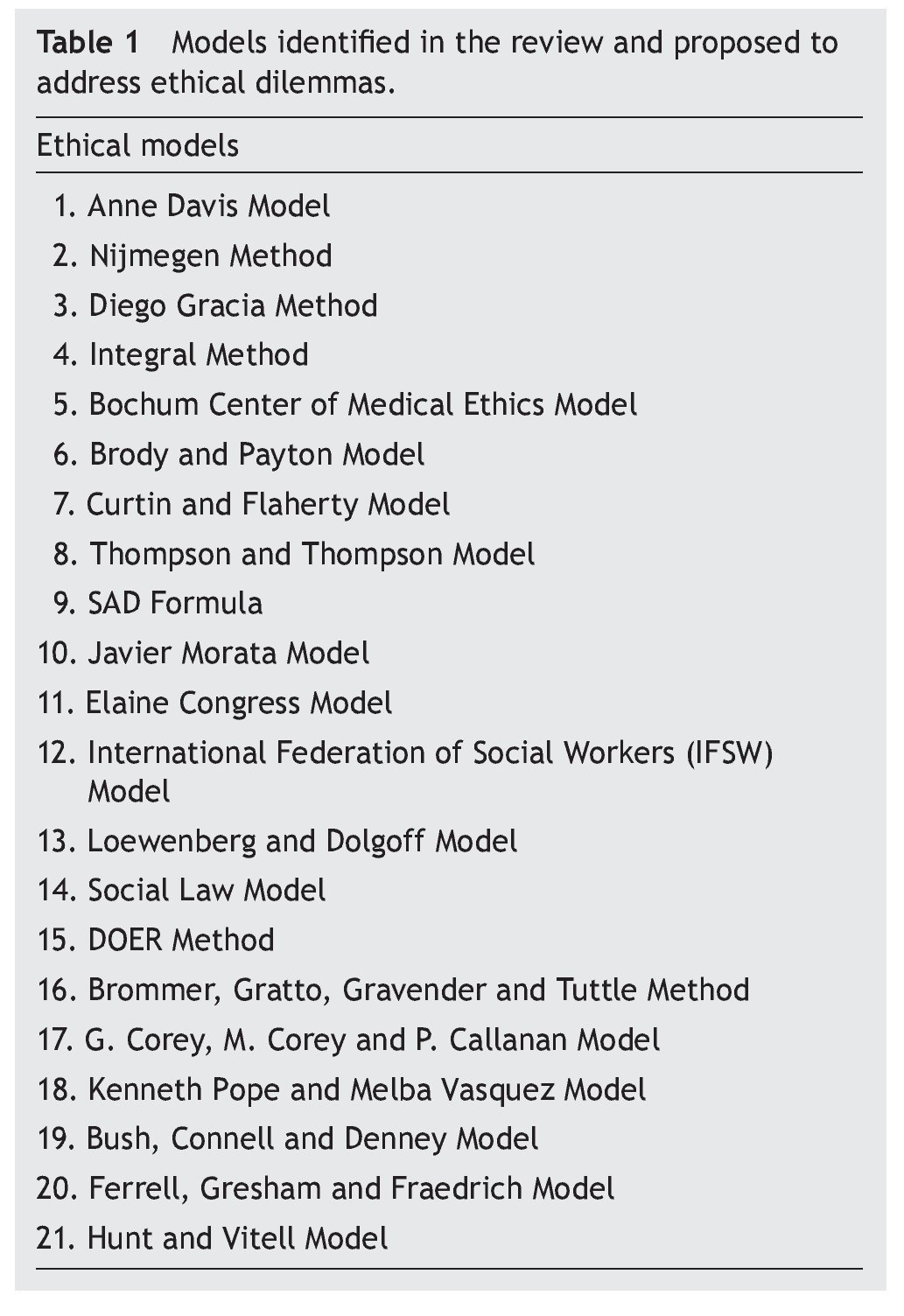
Una revisión de la literatura permitió identificar diferentes modelos que abordan esta clase de dilemas. Se localizaron artículos utilizando las bases de datos Ebsco Host, ProQuest, Ovid e InMex, así como metabuscadores como metacrawler. Algunos de los modelos analizados fueron los siguientes: el Modelo de Anne Davis, el Método de Nijmegen, el Método de Diego Gracia, el Método Integral, el Modelo del Centro de Ética Médica de Bochum, el Modelo de Brody y Payton, el Modelo de Curtin y Flaherty, el Modelo de Thompson y Thompson, la Fórmula SAD, el Modelo de Javier Morata, el Modelo de Elaine Congress, el Modelo IFSW, el Modelo de Loewenberg y Dolgoff, el Modelo de la Ley Social, el Método DOER, el Modelo de Brommer, el Modelo de Corey y Callanan, el Modelo de Pope y Vasquez, el Modelo de Bush, Connell y Denney, el Modelo de Ferrell, Gresham y Fraedrich y el Modelo de Hunt y Vitell.
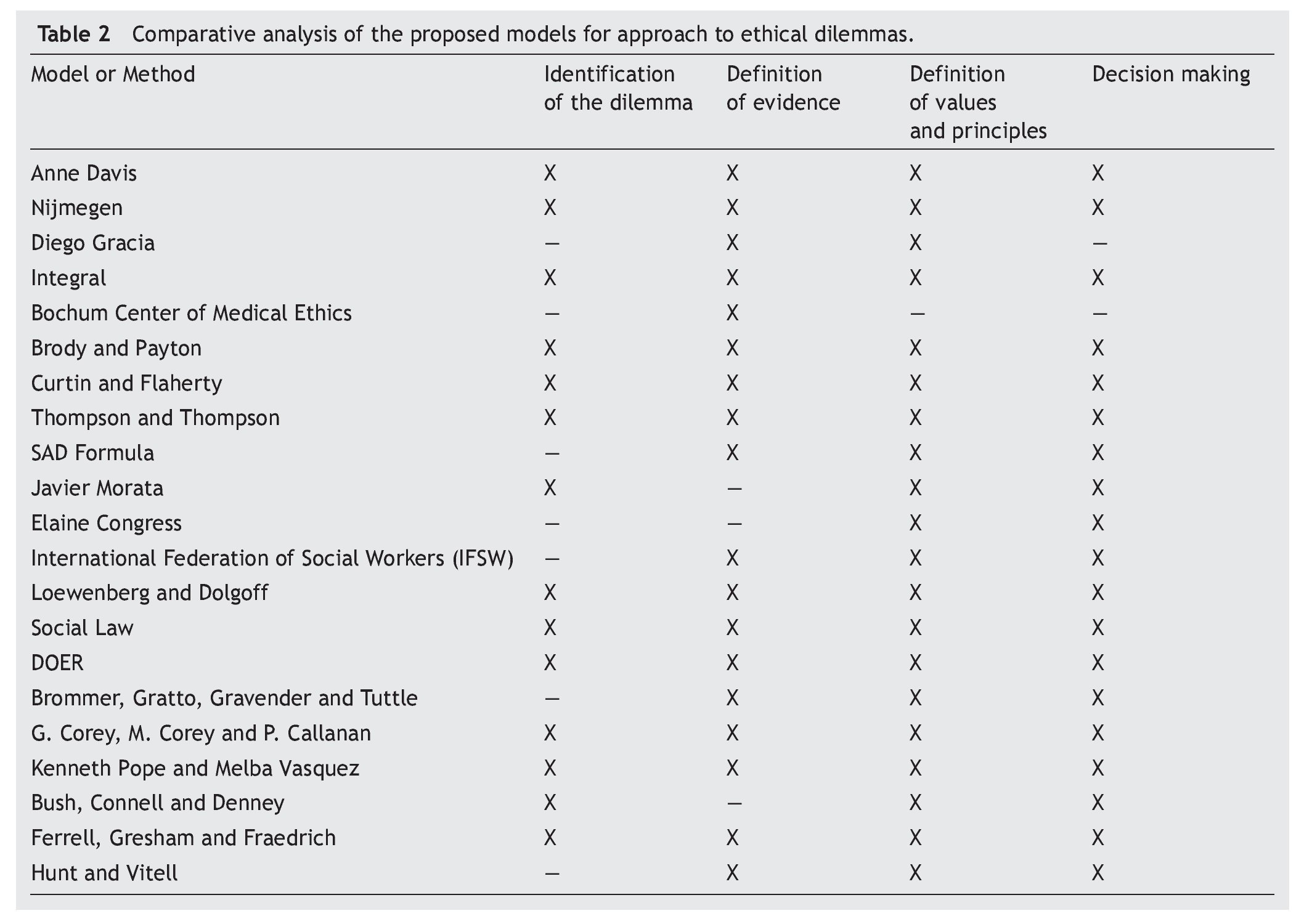
Los criterios compartidos entre los diferentes modelos fueron los siguientes: a) la especificación del dilema ético; b) la descripción de los hechos a considerar; c) la definición de valores, principios y la postura ética que será tomada en consideración; y d) la toma de decisiones con la identificación de alternativas de solución. De acuerdo con la literatura revisada, se explican algunos modelos con el fin de identificar y ejemplificar elementos críticos que pudieran ser utilizados de manera práctica por los Comités de Ética Clínica u Hospitalaria en las instituciones de salud pediátrica en México.
In pediatric medical practice it is common to encounter situations that represent a dilemma for health professionals. A dilemma occurs when ethical problems found in professional practice cause serious internal conflicts because they imply actions that contradict their colleagues, employees, or their own personal values and are classified as personal value conflicts, conflicts with other professionals, conflicts with clients and with organizations.
A literature review allowed identifying different models to debate these types of dilemmas. The present work is a review of the search of scientific articles using databases such as Ebsco Host, ProQuest, Ovid, and InMex as well as metasearch tools such as metacrawler. The models found are as follows: Model of Anne Davis, Nijmegen method, Method of Diego Gracia, Integral method, Bochum Center Ethics model, Model of Brody and Payton, Model of Curtin and Flaherty, Model of Thompson and Thompson, SAD method, Model of Javier Morata, Model of Elaine Congress, IFSW model, Model of Loewenberg and Dolgoff, Ley Social Model, DOER method, Model of Brommer, Model of Corey and Callanan, Model of Pope and Vasquez, Model of Bush, Connell and Denney, Model of Ferrell, Gresham and Fraedrich, and Model of Hunt and Vitell.
The key criteria shared in the different models are a) specifying the ethical dilemma, b) description of the facts, c) value definition, moral code and facts, decision making and d) identifying alternative solutions. In order to review the literature, some models are explained with the purpose of identifying and representing critical elements that clinical ethics committees could use in a practical manner in pediatric health institutions in Mexico.
Pagina nueva 1
1. Introduction
In the practice of pediatric medicine, patients do not directly participate in decision making regarding their health care. Because of this, their wellbeing is dependent on the decisions made by others, which can cause certain ethical dilemmas. Generally, pediatric patients are under the care of their parents or guardians who have multiple obligations and duties. This has an influence, sometimes unfavorable, on the decisions made on behalf of the children. Because of this, physicians have the responsibility of formulating an independent judgment about the best interests of the patient as well as the duty to evaluate and question the decisions made by the parents, always seeking to place the best interest of the child first.1
A dilemma (from the Latin dilemma, two premises) is formulated from two contrary propositions dijunctively.2 An ethical dilemma is a situation in which the moral precepts or similar mandatory ethical obligations are in conflict, so that any possible solution to the dilemma is morally intolerable. Seen from another perspective, an ethical dilemma is a situation where the moral principles that guide behavior do not allow the obvious determination of what is correct or incorrect before two possible courses of action.3
In the area of health, it is necessary to separate the ethical problems that arise from the medical scientific research from the problems that arise during the course of clinical care of patients and that also bring about dilemmas in the decision-making process. In the first case, there is a frame of reference, a standard and legislation for approaching ethical problems associated with the practice of science, tools with which the Ethics Committee of Investigation have for approaching the conflicts generated. In the realm of individual patient care, the field of study of Clinical Ethics4 has emerged as a response to a time when there are more frequent moral conflicts. This discipline has established a space and context for the discussion of ethical problems that arise in patient care. The present work is focused on the latter type of dilemma.
The objective of this study was to identify the necessary or indispensable key elements to carry out the process of reviewing the ethical dilemmas through the analysis of different models described in the literature.
2. Methods
For the literature search, the following databases were used: Ebsco Host, ProQuest, Ovid, and InMex, as well as metasearch engines such as metacrawler. The following key words, both in English and Spanish, were used: «bioethics», «ethics», «ethical and ethics dilemmas», «moral dilemmas», «resolving ethical dilemmas», «analysis dilemmas», «ethical model of decision making», «making an ethical decision», «moral philosophy», «ethic analysis», «models and methods for ethics analysis», «discuss ethics dilemmas».
According to Weinstein et al., a model can be defined as a schematic representation of reality so that its usefulness is eminently practical because it attempts to approach a complex reality, trying to simplify it.5 The models that had an explicit statement by the authors of the following criteria were included: a) the proposal for a model, and as objective b) the analysis of ethical dilemmas. The search was not limited to models focused on health care. The models identified were analyzed by at least two of the authors, and the key elements considered were analyzed to describe them and carry out a comparative exercise. The following aspects were considered for judging an element as a key: to) relevance to meet the goal of analyzing and resolving dilemmas; (b) possibility of applying it to the clinical nature of the problems in health; (c) ability to be adapted to the organizational context of the ethics committees of clinic or hospital in Mexico; and (d) feasibility of applying it in the majority of health care organizations providing specialized pediatric care in the country.
The models identified in the literature are described in the present document, originally proposed to establish a frame of reference for discussing and resolving ethical dilemmas in general and that, in the judgment of the authors, could be useful for formally and structurally facing the ethical dilemmas found in the daily clinical practice of pediatrics. The purpose was to perform a comparative analysis that would allow identifying the common elements that could potentially serve as a foundation for a general model. We did not intended to perform an exhaustive search of all models that have been described for approaching ethical dilemmas. We selected those which, in the opinion of the authors, were representative of the dilemmas for the analysis based on the aforementioned criteria. We identified 21 models having to do with ethical dilemmas and their resolution or with ethical decision making, which were included in the present work as they provided explicit recommendations about how to carry out the analysis of the ethical dilemmas, whether it be in the area of health care or in any other context (Table 1).
From the personal experience of the authors in different health institutions (Mexican Social Security Institute, National Health Institutes and hospitals from the health department), the elements that would be fundamental to carry out the analysis of the dilemmas that tend to present themselves in the ethics committees of the different health institutions in Mexico were discussed. (Phase 1).6 The discussions centered on the need to establish a structured and flexible protocol analysis which, in turn, would be able to be adapted to the general forms of discussion and resolution of the dilemmas commonly presented in the Clinical Ethics Committees. In Phase 2 the different models identified in the literature were analyzed, intentionally searching for those elements of potential use as previously discussed in Phase I. During the review, aside from the search for the aspects previously defined, the intent to identify aspects that had not been previously specified and could be useful for systematizing the analysis was maintained. Once the review was completed and on the basis of the criteria considered key to the analysis, we carried out a comparison of these elements in the models identified (Table 2). It is not considered as necessary for all the models to include all the key elements. Included were those aspects seen with greater frequency.
Finally, the common elements were contrasted with the authors’ experience in the review of ethical dilemmas through meetings in which the relevance and applicability of these elements in the analysis of the dilemmas frequently submitted to the Hospital’s Ethics Committee in Mexico were discussed.
3. Results
3.1. Anne Davis Model
This model presents a guide where the circumstances surrounding the dilemma are considered to be a very important factor. Davis suggests identifying the existence of a dilemma, obtaining the information necessary to establish the facts and limitations of the situation and looking at the ethical principles affected, the obligations of the participants in decision making, and the role of the organization. It proposes the following questions as a way of obtaining relevant information: What is the information available? Is it scientific or sociocultural? What values are involved? What information is needed and is unknown?7,8
3.2. Nijmegen Model
This is a method of deliberation applicable to clinical practice developed in Holland by a multidisciplinary group of physicians with the idea of applying it to ethical discernment. The method emphasizes that it should be the treating physician and health personnel responsible for the patient who should make the ethical decisions. In this sense, it moves away from the North American focus of seeking advice. The method initially consists of defining the dilemma or ethical problem, the surroundings relative to the organization and its influence on the health personnel as well as the patient’s values and social background. Subsequently, evaluation is done based on the good of the patient, taking into consideration autonomy and responsibility of the professionals with health care. Decision making should summarize the moral problem and then evaluate it to see its impact.9
3.3. Diego Gracia Method
This method proposes that moral reasoning, which is established in order to carry out a process of deliberation, has three levels: the first is the general frame of reference or canon of morality from which the facts should be contrasted. The frame of reference is fundamentally ethical, which states that all humans are persons and therefore have dignity at any cost. In this sense, one would have to accept the precept that all persons are equal and deserve the same consideration and respect. A second level focuses on defining and establishing moral outlines in the form of values and ethical principles (autonomy, beneficence, nonmalfeasance and justice), for which, however, Gracia provides a critical framework. The third level of moral reasoning is the analysis of the circumstances and consequences of the concrete act that ultimately leads to the definition of a moral duty as well as a legal duty.10
3.4. Whole Method
Developed in Mexico by a group of physician specialists in the field, this method suggests the need to work in clinical practice with the highest level of ethics that guarantees the development and integrity of persons according to technological scientific and biomedical advances. It integrates the three aspects of the action: the moral agent, action (rights and obligations) and the consequences of the action. It analyzes the good from various ethical perspectives, with flexibility and searching for ethical principles that refine persons in the relationship between clinicians and patients. Critical thinking is favored in which the entire health care team, patients and relatives participate, allowing the treating physician to make a responsible decision, i.e., with knowledge, free will and freedom, deploying the physician’s maximum moral power. It does not seek consensus because the ethical decision by consensus is anonymous and no one takes direct responsibility. Ethical analysis should be performed from the utilitarian, deontological and erotological points of view, i.e., integral, in order to achieve the widest possible vision.11,12
3.5. Medical Ethics Center of Bochum Model
This model was developed by Dr. Hans-Martin Sass and Dr. Heben Viefhues, the founder of the center of medical ethics in Bochum in 1985 and has been widely used in Argentina. It is based on the formulation of questions and on the identification of scientific and medical/ethical findings. It seeks to carry out reflections of a general nature surrounding the health and wellbeing of a person as well as inquiring about information in regard to the patient’s self-determination. The authors emphasize case management and recommend taking into account the physician’s actions as well as the inherent medical responsibility. Additionally, the authors pose questions regarding the manner in which the ethical evaluation takes place in cases with prolonged treatment, which have social relevance and in which family, emotional, economic and profession complications are identified.13
3.6. Brody and Payton Model
At the beginning of the 1970s, Howard Brody developed a model for making ethical decisions based on utilitarianism and deontology. The model could be applicable in different situations related to health care and from any theoretical perspective. The perception of the problem could be developed through the utilitarian approach, with a list of alternatives and their possible consequences. A value would be assigned to the happiness produced and the alternative that could produce the greatest happiness would be selected. Using the deontological perspective the alternatives could be enlisted and then compared with the rules and principles. If an alternative is consistent with the standard/principle, then it would indicate a correct action. If several alternatives were consistent with the standards/principles, it would mean that there are several correct actions. However, only one action should be chosen.14
3.7. Curtin and Flaherty Model
In the first place, this model proposes to gather information related to the history of the case, for which it suggests several questions to be answered to complement them. For example, who is compromised in this situation? What scientific, cultural, sociological and psychological information is available? What additional information is required? As a second point, the ethical component and the ethical principles involved need to be identified. It needs to be defined whether it is an ethical conflict or conflict of rights, if it is a matter of lying or telling the truth, or if the matter translates into a conflict of power against authority. It recommends that the persons involved be defined in the decision making and to outline the possible options for action trying to predict the possible consequences, always identifying the underlying principles and moral/ethical theories (utilitarian, deontologic, theory based on human rights, and personal or professional ethics). The following step is the compilation of facts and principles, placing them hierarchically, as well as the inclusion of the points of view of each one of the participants. Finallly, a resolution should be reached and should be executed.15
3.8. Thompson and Thompson Model
This model was developed in the early 1970s and has been a reference for the development of other models. This proposal places emphasis on the identification of the decision that should be taken so that the persons involved in the process direct their efforts toward it. In a second step the situation is reviewed to identify the context and the problems, the ethical and moral aspects and the persons involved in the situation. In third place, information must be gathered to clarify the situation, link the problem with the ethics of the situation and subsequently the moral and ethical position is defined, both personal as well as professional, as well as the conflicts with values or principles, if they exist. It is necessary to determine who should make the decisions and identify the scope of the actions and anticipate the results. Once this is done, a decision should be made on the behavior to follow, explain it and place it into practice. Finally, it is necessary to review and evaluate the results of the decision and the action taken.16
3.9. SAD Formula
This proposal was developed by Louis Alvin Day with the goal of integrating elements of critical thinking on moral reasoning. Critical thinking is a rational focus on making decisions that emphasize the careful analysis and evaluation, both of the definition of the problem as well as the solutions adopted. The method consists of the following steps:
Situation: Its purpose is to identify the facts and to obtain sufficient information on the problem so as to understand the context of the ethical dilemma.
Analysis: This phase constitutes the longest part of the exercise because it requires the identification of the principles and values involved. Its purpose is to apply moral theories and to consider ethical alternatives.
Decision: This last step is focused on describing in one line the behavior to follow so that the person responsible carries it out. This decision should be defended so one should be prepared to substantiate it in front of its critics. Its purpose will be to establish an ethical judgment or conclusion based on the information and available alternatives.17
3.10. Javier Morata Model
Family medicine. Family medicine establishes the need to carry out ethical reflection and, as a result, to make interventions at the first level of clinical practice. It mentions that ethical dilemmas are not always the type involving life or death situations because there are dilemmas found in daily practice in which one must face situations that cause ethical conflicts. Morata makes explicit the possibility that once all these steps have been exhausted, there is no satisfactory solution found, or that once the solution found is applied, that it does not totally resolve the problem. His model consists of the following three phases:
1) Stage I: Gathering data to detect problems from the clinical, technical, and ethical point of view as well as from similar experiences in order to study the personal, family and social circumstances.
2) Stage II: Examine the possible courses of action and evaluate the consequences that require preventive actions to take place. During this stage the subject of the action is analyzed and has to collaborate on the solution; therefore, the degree of competence, aptitude, and ability of the physician, the patient and the remainder of the participants should be recognized.
3) Stage III: Decision making and execution.18
3.11. Elaine Congress Model
Elaine Congress, Professor and Associate Dean at Fordham University (NY) in the early 1990s, suggested a model for ethical decision-making that would be fast and efficient at the same time. Congress, using the two underlying philosophical traditions in social work—the Kantian or deontological (self-determination and confidence) and the utilitarian or teleological (consequentialist)—attempted to simultaneously take into consideration the principles and the philosophical bases of both traditions to propose a model called ETHIC, whose bases rest on the values, code of ethics and context in which social work is carried out. Her method takes the following steps into consideration:
E. Examine the relevant and social values of the person, business, user and professional.
T. Apply to the situation the standards of the Code of Ethics of the NASW as well as the relevant laws.
H. Propose a hypothesis about the possible consequences of the different decisions.
I. Identify who will benefit and who will harmed in light of the obligation of the social work with the most vulnerable population.
C. Consult with the supervisor and with other colleagues about the ethical decision judged to be adequate.19
3.12. International Federation of Social Workers (IFSW) Model
The International Federation of Social Workers, founded in Paris in 1928 and reestablished in Munich in 1956, proposed a resolution of an ethical dilemma model jointly with the Center for Human Rights. It is a model that requires taking into account the basic principles contained in the codes of ethics, the context in which actions are carried out, the reasons persons have for their behavior, the moral content of the acts and their consequences. The model proposes four steps:
1) Should be based on the deontological and utilitarian ethical theories
2) Should use a moral code
3) System of rules derived from the principles
4) Superiority of the moral rules above and beyond judgments and individual actions20
3.13. Loewenberg and Dolgoff Model
This work had a great influence during the 1980s. It is based on the theoretical proposals of different authors and recommended gradual decision making and in which several factors, people and history should be taken into consideration. It proposes the following:
1) Identify the problem and the factors contributing to maintaining the problem.
2) Take into consideration the persons and institutions involved with the mentioned problem.
3) Identify the values held by the different participants and which are relevant to the problem.
4) Express the goals and objectives to be resolved, or at least to be reduced, in relation to the problem.
5) Make explicit the intervention strategies being considered.
6) Ensure the effectiveness and efficacy of each alternative in terms of the goals identified.
7) Determine who should be involved in the decision making.
8) Choose the most appropriate strategy.
9) Implement the strategy selected
10) Follow-up on the implementation, paying particular attention to the consequences not previously anticipated.
11) Evaluate the results and identify additional problems.21
3.14. Social Law Model
Based on previous proposals,10 a model was proposed that intends to emphasize the justification of the ethical decisions made within the institutions. The model is divided into three parts, the first more generic, whereas in the second part the ethical principles are analyzed and a hierarchy within them is proposed; the third part includes the action and the evaluation. First part: 1) narrate the events; 2) identify the relevant data from the case; 3) identify the nature of the ethical problem; 4) identify those affected by the problem and their reasons; 5) generate possible alternatives to the problem posed; 6) consider the difficulties of putting such alternatives into practice.
In the second part, ethical evaluation and decision making is required: 7.1) a system of moral reference; 7.2) consider the moral principles; 7.3) take into account the moral consequences, both subjective as well as objective (it is necessary to ask oneself if there is conflict within the consequences); and 7.4) take the moral decision in which resolution of the conflict should be achieved. The consequences should be related with the principles and resolve, if there exists, the conflict in principles. This is done in order to obtain a contrast of the results with the system of reference and, in this way, make a final decision.
In the third part, it is necessary 8) to place into practice the decision adopted and 9) to evaluate it.22
3.15. DOER Method
The DOER method was proposed by the Spanish Society of Nursing Urgencies and Emergencies. This method is comprised of four phases:
Delimit the conflict with a complete evaluation of the patient’s health, identifying reasons, circumstances and facts. It is also necessary to consider the deontological code.
Offer the patient options with objective, true and complete information.
Elect the option that seems optimal for the patient who should choose it freely based on the alternatives offered.
Resolve the conflict and communicate with the interdisciplinary team the option chosen by the patient and the stance to adopt, later evaluating this choice.23
3.16. Brommer, Gratto, Gravender and Tuttle Model
These authors propose a model whose goal is to explain ethical decision making. The model makes fundamental reference to two broad categories that have an influence on decision making; on one hand, environmental factors and on the other, individual factors. Among the factors attributable to the environment are diversity of the environment, work, personnel who work in the organizations, professional aspects, governmental, legal and social aspects. Individual factors may also intervene in the decision; however, these factors are not raised as constraints, but as facilitators. The model is comprised of six large groups divided into categories, although in general, it is expected that in the model about 20 variables would intervene or would be relevant for making ethical decisions.24,25
3.17. G. Corey, M. Corey and P. Callanan Model
These authors propose a model that integrates eight steps.
1) Identifythedilemma.
2) Identify the possible problems involved.
3) Review the relevant ethical codes.
4) Know the laws and regulations that may be applied to the case.
5) Make the consults that may be required to clarify the case.
6) Consider the possible directions of the action to carry out.
7) Enumerate the consequences of the different alternatives.
8) Decide which would be the best option.
The model comes up in the context of counseling. In this aspect, it recommends not assuming a sole posture in relation to the theories. On the contrary, one must use the elements that are useful for better decision making. These authors visualize counseling as a tool that can substantially change the lives of people. From there, they emphasize on the ethical elements that should be considered.26
3.18. Kenneth Pope and Melba Vasquez Model
This model was initially published in 1991 and consists of the following steps:
1) Identify the situation that requires making an ethical decision.
2) Anticipate who will be affected by this decision.
3) Identify the person who is in the center of the events.
4) Assess the relevance of the different areas involved in the situation (e.g., degree of knowledge and experience).
5) Review the ethical standards.
6) Include the pertinent aspects of the legislation to the case.
7) Review the theory and the relevant investigations.
8) Take into consideration the personal feelings and identify if there are prejudices or any conflicts of interest.
9) Foresee the social, cultural and religious effects.
10) Consult with other experts.
11) Identify the different courses of action that could be taken in the case.
12) Evaluate different alternatives of action.
13) View from the perspective of each of the persons who will be affected.
14) Decide what will be done, then review and consider it.
15) Act assuming the responsibilities of the decision.
16) Evaluatetheresults.
17) Assume the responsibility of the consequences of the actions.
18) Anticipate the implications of the case to be prepared for planning action responses.27
3.19. Bush, Connell and Denney Model
This model is based on the Theory of Systems and is focused on forensic psychology ethical decision making, which includes the following points:
1) Identification of the problem
2) Development of possible solutions
3) Consideration of the consequences for each of the possible solutions
4) Election and implementation of a course of action
5) Evaluation of the results and execution of necessary changes
To this model, three additional steps are added before a decision is made:
A) Considerations about the context of the problem and its surroundings
B) Identification and use of the ethical-legal resources
C) Analysis of the beliefs and values of the persons involved in the dilemma28
3.20. Ferrell, Gresham and Fraedrich Model
This model incorporates the theory of Kohlberg’s cognitive moral development. In this way, personal aspects can be combined with elements of the environment. It supposes that the behavior before an ethical dilemma is found to be directly related with its nature, the characteristics of each person and close persons, as well as the opportunities available to resolve it. The approach is based on the point of view of the institutional organization and takes into consideration the following factors:
1) Individual factors—in decision making, individuals are influenced by moral, family, and social aspects and by their education, as well as by beliefs and behaviors acquired through formal education and by the relevant cultural background for ethical behavior.
2) Organizational factors—the ethical behavior of individuals will largely depend on the influence of key persons within the organization to which they belong.
3) Social and economic environment—from here come the previously established codes of ethics or punishments and rewards relative to the behavior of the individuals within the organization.29
3.21. Hunt and Vitell Model
These authors designed the “General Theory of Marketing Ethics.” In this model, the moral philosophical theory, from the deontological and teleological perspectives, make up a large part. The proposal emphasizes on ethical decision making. It does not prescribe. It arises from the idea that in the organizations, employees generally perceive ethical problems when these arise. The key elements in the model structure describe the possible alternatives and specify the following environments to consider:
1) Cultural environment—religion, legal system and the political system
2) Professional environment—informal standards, formal codes and application of the codes
3) Labor/industrial environment
4) Organizational environment
5) Personal characteristics—religion, values, strength of moral character, moral cognitive development, beliefs and ethical sensitivites30,31
4. Discussion
Hospital ethics committees face, on a daily basis, the enormous challenge of analyzing deep moral problems and have the responsibility of issuing opinions and recommendations regarding their resolution. To meet these commitments, a professional, multidisciplinary staff is required, having the theoretical tools and necessary experience to make judgments that will affect essential aspects of human nature.
The analysis of an ethical dilemma in medicine is of great complexity, especially due to the great diversity of aspects involved and because of ethical positions, sometimes poorly defined, of the committee members. To carry out this task, it is crucial that when cases are discussed there is information available that would give order to the process to ensure an exhaustive review of the different aspects involved as well as a clear definition of the ethical stances faced in topics in which divergent opinions are commonly held and positions found. In the experience of the authors, the review process carried out by some of the ethics committees in Mexico tends to be poorly structured and commonly lack systematization. Generally, it is guided by intuition. The ethical postures are not made explicit and occasionally the dilemmas are not clearly stated. This situation makes for a difficult debate and makes resolution rare.
The models described in this article are examples of various attempts to deal with the discussion and analysis of ethical dilemmas in the health care field. Most of the models emphasize the specification of the dilemma, identification of values and ethical principles that may serve as a basis for its resolution and, finally, in decision making.
Derived from the identification of commonalities in the models reviewed and with the integration of local experience, an attempt is being made to identify a proposal adapted to our context with the highest level of simplification. It was possible to identify four relevant stages. The first is to establish the ethical dilemma, an aspect in which the majority of the models agreed. In the second stage the facts seen as relevant should be specified for discussion and potential resolution of the dilemma. In the third stage, it is appropriate to make explicit the values and principles that will be considered as well as the ethical stances assumed in the case itself. In the fourth stage it is required that a joint decision be made as a committee in order to establish educated recommendations to those requesting the decisions.
In order to facilitate an in-depth and relevant analysis of cases presented to the clinical and hospital ethics committees, the participation of professionals from diverse areas of health care is required, including legal areas. In general, it can be considered that this aspect is found to be advanced in Mexico because the legislation provides a defined frame of reference. This article, however, is centered on the proposal of structuring, in a reasonable and flexible manner, review of the cases, which should be sufficiently dynamic and general such as to allow approaching the high complexity of the problems presented.
The legal framework related with the actions of the hospital ethics committee is contemplated in the General Health Act and operated through the National Bioethics Committee (CONBIOETICA), a decentralized body of the Ministry of Health with technical and operative autonomy and the ability to point out the criteria under which both the hospital bioethics committee as well as the ethics in research committee should act.32,33
One element that emerges from the analysis in the majority of models reviewed is that which refers to the need to make explicit the values, principles and ethical positions, first at an individual level and second by the committee in order to face the dilemma and to attempt its resolution. This aspect requires the clinical or hospital ethics committees to promote and facilitate the education and culture necessary for its members to incorporate these elements into their professional background with the purpose that the discussion and analysis be many, broad and sensitive around the different world views. The fact of delving deeply into the ethical theories that underpin medical practice will contribute to offer greater clarity and transparency to the recommendations by the hospital ethics committee. These recommendations, without a doubt, will deeply affect not only the life and future of the patients, but will also have a decisive influence in their familial and social surroundings.
Based on the analysis of the models that have been described for dealing with ethical dilemmas, four stages in the review process could be identified. The stages are as follows: 1) identify the ethical dilemma; 2) explain the relevant facts for the discussion of the dilemma; 3) expose the ethical positions; 4) make a decision.
Fulfillment of these stages would make it possible to ensure a comprehensive review by the clinical ethics committees. The members of hospital ethics committees require forming an ethical posture that allows them to give greater strength and transparency to its recommendations.
Ethical responsibilities
Protection of human and animal subjects. The authors declare that no experiments were performed on humans or animals for this investigation.
Confidentiality of Data. The authors declare that no patient data appear in this article.
Right to privacy and informed consent. The authors declare that no patient data appear in this article.
Funding
None.
Conflict of interest
The authors declare no conflict of interest of any nature.
Received 13 February 2015;
accepted 24 March 2015
http://dx.doi.org/10.1016/j.bmhimx.2015.03.006
* Corresponding author.
E-mail:juan.gardunoe@gmail.com (J. Garduño-Espinosa).