In patients with septic shock, excessive fluid administration can lead to increased morbidity and mortality. The aim of this study was to evaluate the association between fluid balance, acute kidney injury and mortality in patients with septic shock.
MethodsA study of cases and controls was conducted in a pediatric intensive care unit. The fluid balance in the first 72h and the presence of acute kidney injury was compared in patients diagnosed with septic shock who died against patients who survived the same condition. Univariate and multivariate analyses were performed.
ResultsForty-five cases and forty-five controls were included in the analysis. Mortality was associated with Pediatric Risk of Mortality (PRISM III) ≥ 26 points (OR 7.5, 95% CI 2.8-18.7; p=0.000), Pediatric Logistic Organ Dysfunction (PELOD) ≥ 24 points (OR 11.0, 95% CI 4.1-29.4; p=0.000), creatinine ≥ 0.65mg/dl (OR 5.6, 95% CI 2.2-13.9; p=0.000), lactate ≥ 2.5 mmol/l (OR 2.5, 95% CI 1.1-5.9; p=0.033), SvO2 < 60% (OR 4.6, 95% CI 4.5-4.5; p=0.001), positive balance > 9% in 72h (OR 4.3, 95% CI 1.6-11.7; p=0.003), acute kidney injury (OR 5.7, 95% CI: 2.2-15.1; p=0.000). In the multivariate model, the values of PRISM ≥26 and PELOD ≥24 points were significant.
ConclusionsIn patients who died due to septic shock, the multivariate model showed an association with PRISM ≥26 and PELOD ≥24 and a trend toward association with SvO2 <60% and positive balance of liquids > 9%.
En el paciente con choque séptico, la administración excesiva de líquidos puede incrementar la morbilidad y mortalidad. El objetivo de este estudio fue evaluar la asociación entre el balance de líquidos, la lesión renal aguda y la mortalidad en pacientes con choque séptico.
MétodosSe realizó un estudio de casos y controles en una unidad de terapia intensiva pediátrica. Se comparó el balance de líquidos en las primeras 72h y la presencia de lesión renal aguda en pacientes con diagnóstico de choque séptico que fallecieron contra pacientes que sobrevivieron a la misma patología. Se realizó un análisis univariado y multivariado.
ResultadosSe incluyeron 45 casos y 45 controles en el análisis. La mortalidad se asoció con riesgo pediátrico de mortalidad (PRISM) ≥ 26 puntos (RM 7.5, IC 95% 2.8-18.7; p=0.000), disfunción orgánica logística pediátrica (PELOD) ≥ 24 puntos (RM 11.0, IC 95% 4.1-29.4; p=0.000), creatinina ≥ 0.65mg/dl (RM 5.6, IC 95% 2.2-13.9; p=0.000), lactato ≥ 2.5 mmol/l (RM 2.5, IC 95% 1.1-5.9; p=0.033), SvO2<60% (RM 4.6, IC 95% 4.5-4.5; p=0.001), balance positivo > 9% en 72h (RM 4.3, IC 95% 1.6-11.7; p=0.003), lesión renal aguda (RM 5.7, IC 95% 2.2-15.1; p=0.000). En el modelo multivariado, PRISM ≥ 26 y PELOD ≥ 24 puntos permanecieron significativas.
ConclusionesEn los pacientes que fallecieron por choque séptico, el modelo multivariado mostró una asociación con PRISM ≥26 y PELOD ≥24 y una tendencia hacia la asociación con SvO2 <60% y balance de líquidos positivo >9%.
Septic shock approach guided by goals has reduced morbidity and mortality both in adults and children.1 These guides encompass early recognition of the problem, vascular access, fluid resuscitation, antibiotics therapy and use of vasopressors during the first hour. Early fluid resuscitation is the cornerstone in the management of shock, and it is part of the goal-directed therapy of the “Surviving sepsis” campaign, aimed at restoring the hemodynamic integrity and tissue perfusion.2 However, the critical patient has an increased fluid retention secondary to an enlarged capacity of intravascular space and third space, as well as a decreased renal ability to excrete the fluid excess.3–5 The positive fluid balance has been associated with an increase in morbidity and mortality in patients with acute lung injury and septic shock. Probably this is because excessive fluid administration in patients with sepsis can lead to impairment of respiratory function, increased intraabdominal pressure, clotting disorders and cerebral edema.6,7
Recent observational papers showed an association between fluid overload and increased morbidity and mortality in the pediatric population, especially after cardiac surgery and in children requiring continuous renal replacement therapy.8–12 Acute kidney injury contributes directly to the water and sodium clearance and excretion and has been established as a mortality risk factor.13,14 In studies were children with septic shock where fluid overload was evaluated, acute kidney injury and the impact on mortality are scarce and the size of the sample is generally small. This study aimed to compare the positive fluid balance and acute kidney injury (AKI) among a group of pediatric patients who died of septic shock and children with septic shock who survived. The hypothesis assumes that fluid overload and AKI during the first 72hours was higher in patients who died from septic shock.
2MethodsThe study was conducted in the pediatric intensive care unit (PICU) of the Children's Hospital Dr. Rigoberto Aguilar Pico, in Sinaloa, Mexico, from January 2010 to December 2014. The Institutional Research Committee approved the study.
For the study, physical or electronic records from patients aged ≤ 18 years diagnosed with septic shock and hospitalization in PICU ≥ 72hours were included. Patient records with hospital admission<48hours, deaths or transfer out of the PICU, infants<30 days and records with incomplete data were excluded. To homogenize the condition in the case and control groups, children with chronic diseases, such as kidney failure, complex congenital heart disease and with surgical correction of congenital heart disease were excluded.
2.1Operational definition of variablesThe fluid balance was estimated by the difference between the total liquids administered and the total of outflows or losses during the first 72hours of admission to the PICU. The percentage of patient body weight was expressed according to the following formula:
Income (liters) – Expenses (liters)/admission weight (kg) at PICU x 100
For the fluid balance calculation, admission weight of the patient to PICU15 was documented.
Septic shock was defined as an acute organ failure (acute renal failure, respiratory failure) in the presence of an infection and the need for vasopressor for more than six hours. Respiratory failure was defined as the need for respiratory support (noninvasive and invasive ventilation).16
AKI was defined as an increase in serum creatinine ≥ 50% of baseline when admitted to PICU and/or urine output<0.5ml/kg per hour for six hours, according to the criteria of the Acute Kidney Injury Network (AKIN).17
Pediatric Risk of Mortality (PRISM) score was defined as the score that estimates the risk of mortality at PICU with the information obtained at admission.18
The Pediatric Logistic Organ Dysfunction score (PELOD) assigns values to each organ failure according to severity. Subsequently, these values are summarized in a score that corresponds to the sum of the individual scores.19
Other variables included were age, gender, days of hospitalization in the PICU, ventilation assistance, serum lactate, serum creatinine, the primary site of infection, central venous oxygen saturation (ScvO2) and AKI.
Patients who died of septic shock were considered as cases and children who survived the septic shock, as controls.
2.2Sample sizeThe sample size was estimated according to the comparison of mortality reported by Bhaskar et al.20, wherein the group of patients with septic shock and fluid overload showed a mortality of 37% and in the group with septic shock without fluid overload mortality was 3%, with an alpha of 0.05 and a statistical power (1-β) of 80%. The minimum sample size for each group was 21 cases of patients with septic shock.
2.3Statistical analysisFor the analysis of demographic and clinical variables, descriptive statistics were used. According to the non-normal data distribution, medians and interquartile ranges (IQR) or proportions were used. For comparisons between groups, the continuous variables were compared by Mann-Whitney U test for non-normal distribution variables. The unvaried analysis was performed between the dependent and independent variables. For this analysis, the categorical variables were transformed into indicator variables and the continuous variables into dichotomous variables when analyzing the best cut on the ROC (Receiver Operating Characteristic) curve. Variables with p-value ≤ 0.1 were introduced to multivariate analysis. A value of p<0.05 was considered statistically significant for all comparisons. The statistical analysis was performed with the SPSS package version 22.0.
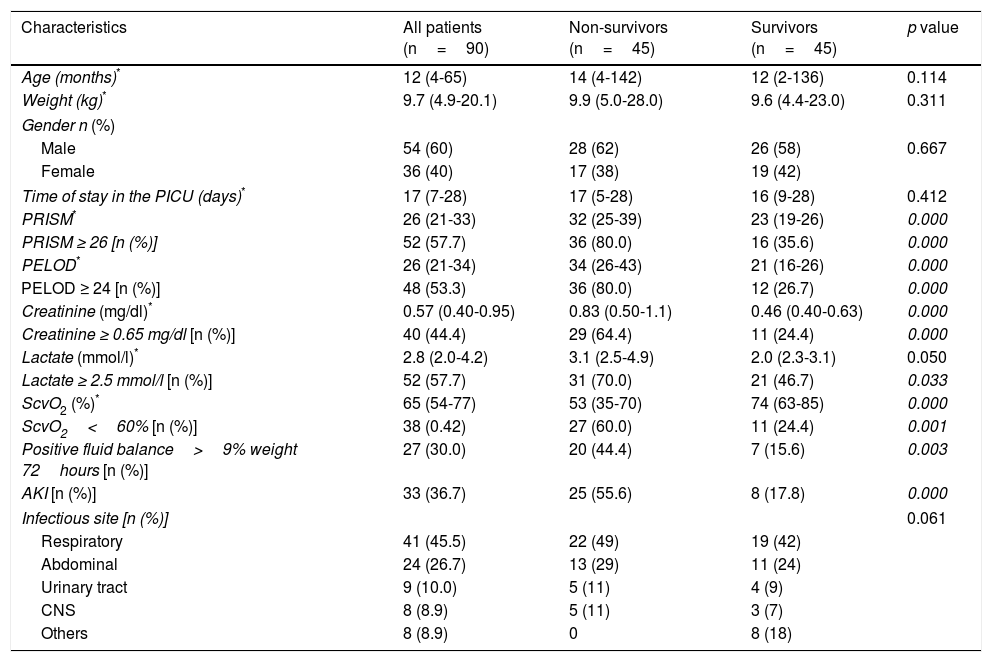
3ResultsDuring the study period, 925 patients were admitted to the PICU, of which 16.9% (157/925) were diagnosed with septic shock. Sixty-seven patients did not meet the inclusion criteria, and 90 patients were included in the final analysis: 45 cases (non-survivors) and 45 controls (survivors). The median age was 12 months [IQR (25-75) 4-65 months]. Male gender presented a frequency of 60% (54/90). The median for fluid balance at 72hours was 141ml [IQR (25-75) -99-427ml]. A percentage of 36.6% (33/90) presented acute kidney failure (Table 1). All patients received vasopressors and assistance with mechanical ventilation.
General characteristics of the patients.
| Characteristics | All patients (n=90) | Non-survivors (n=45) | Survivors (n=45) | p value |
|---|---|---|---|---|
| Age (months)* | 12 (4-65) | 14 (4-142) | 12 (2-136) | 0.114 |
| Weight (kg)* | 9.7 (4.9-20.1) | 9.9 (5.0-28.0) | 9.6 (4.4-23.0) | 0.311 |
| Gender n (%) | ||||
| Male | 54 (60) | 28 (62) | 26 (58) | 0.667 |
| Female | 36 (40) | 17 (38) | 19 (42) | |
| Time of stay in the PICU (days)* | 17 (7-28) | 17 (5-28) | 16 (9-28) | 0.412 |
| PRISM* | 26 (21-33) | 32 (25-39) | 23 (19-26) | 0.000 |
| PRISM ≥ 26 [n (%)] | 52 (57.7) | 36 (80.0) | 16 (35.6) | 0.000 |
| PELOD* | 26 (21-34) | 34 (26-43) | 21 (16-26) | 0.000 |
| PELOD ≥ 24 [n (%)] | 48 (53.3) | 36 (80.0) | 12 (26.7) | 0.000 |
| Creatinine (mg/dl)* | 0.57 (0.40-0.95) | 0.83 (0.50-1.1) | 0.46 (0.40-0.63) | 0.000 |
| Creatinine ≥ 0.65 mg/dl [n (%)] | 40 (44.4) | 29 (64.4) | 11 (24.4) | 0.000 |
| Lactate (mmol/l)* | 2.8 (2.0-4.2) | 3.1 (2.5-4.9) | 2.0 (2.3-3.1) | 0.050 |
| Lactate ≥ 2.5 mmol/l [n (%)] | 52 (57.7) | 31 (70.0) | 21 (46.7) | 0.033 |
| ScvO2 (%)* | 65 (54-77) | 53 (35-70) | 74 (63-85) | 0.000 |
| ScvO2<60% [n (%)] | 38 (0.42) | 27 (60.0) | 11 (24.4) | 0.001 |
| Positive fluid balance>9% weight 72hours [n (%)] | 27 (30.0) | 20 (44.4) | 7 (15.6) | 0.003 |
| AKI [n (%)] | 33 (36.7) | 25 (55.6) | 8 (17.8) | 0.000 |
| Infectious site [n (%)] | 0.061 | |||
| Respiratory | 41 (45.5) | 22 (49) | 19 (42) | |
| Abdominal | 24 (26.7) | 13 (29) | 11 (24) | |
| Urinary tract | 9 (10.0) | 5 (11) | 4 (9) | |
| CNS | 8 (8.9) | 5 (11) | 3 (7) | |
| Others | 8 (8.9) | 0 | 8 (18) | |
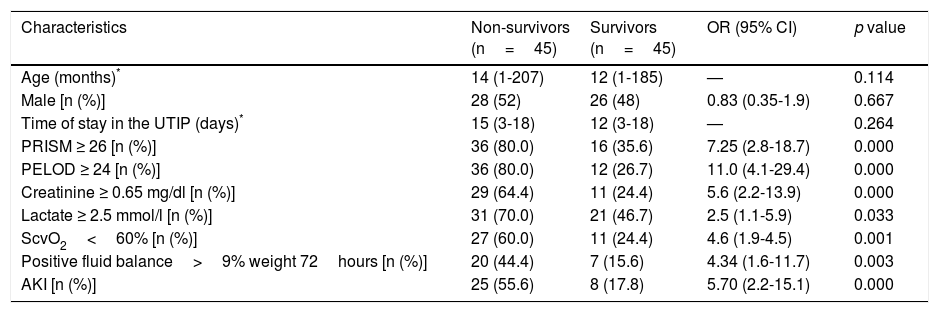
Univariate analysis showed that a PRISM ≥ 26 points (OR 7.5; 95% CI 2.8-18.7), a PELOD ≥ 24 points (OR 11.0; 95% CI 4.1-29.4), creatinine ≥ 0.65mg/dl (OR 5.6; 95% CI 2.2-13.9), lactate ≥ 2.5 mmol/l (OR 2.5; 95% CI 1.1-5.9), ScvO2<60% (OR 4.6; 95% CI 4.5-4.5), positive balance>9% of weight in 72hours (OR 4.3; 95% CI 1.6-11.7) and acute kidney injury (OR 5.7; 95% CI 2.2-15.1) were associated with mortality (Table 2).
Univariate analysis of clinical and laboratory characteristics among non-survivors and survivors septic shock pediatric patients.
| Characteristics | Non-survivors (n=45) | Survivors (n=45) | OR (95% CI) | p value |
|---|---|---|---|---|
| Age (months)* | 14 (1-207) | 12 (1-185) | — | 0.114 |
| Male [n (%)] | 28 (52) | 26 (48) | 0.83 (0.35-1.9) | 0.667 |
| Time of stay in the UTIP (days)* | 15 (3-18) | 12 (3-18) | — | 0.264 |
| PRISM ≥ 26 [n (%)] | 36 (80.0) | 16 (35.6) | 7.25 (2.8-18.7) | 0.000 |
| PELOD ≥ 24 [n (%)] | 36 (80.0) | 12 (26.7) | 11.0 (4.1-29.4) | 0.000 |
| Creatinine ≥ 0.65 mg/dl [n (%)] | 29 (64.4) | 11 (24.4) | 5.6 (2.2-13.9) | 0.000 |
| Lactate ≥ 2.5 mmol/l [n (%)] | 31 (70.0) | 21 (46.7) | 2.5 (1.1-5.9) | 0.033 |
| ScvO2<60% [n (%)] | 27 (60.0) | 11 (24.4) | 4.6 (1.9-4.5) | 0.001 |
| Positive fluid balance>9% weight 72hours [n (%)] | 20 (44.4) | 7 (15.6) | 4.34 (1.6-11.7) | 0.003 |
| AKI [n (%)] | 25 (55.6) | 8 (17.8) | 5.70 (2.2-15.1) | 0.000 |
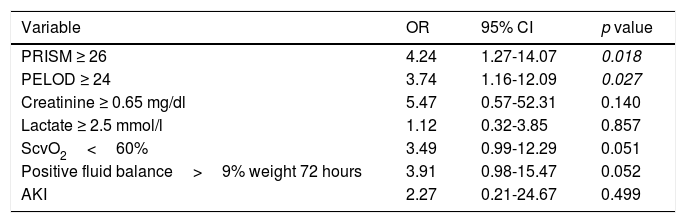
Multivariate analysis showed that a PRISM ≥ 26 points (OR 4.24; 95% CI 1.27-14.07) and a PELOD ≥ 24 points (OR 3.74, 95% CI 1.16-12.09) remained significantly associated with mortality. Variables like ScvO2 (OR 3.49; 95% CI 0.99-12.29) and positive balance>9% of weight in 72hours (OR 3.91; 95% CI 0.98-15.47) showed a tendency to be associated with mortality, while AKI was not statistically significant (Table 3).
Multivariate analysis.
| Variable | OR | 95% CI | p value |
|---|---|---|---|
| PRISM ≥ 26 | 4.24 | 1.27-14.07 | 0.018 |
| PELOD ≥ 24 | 3.74 | 1.16-12.09 | 0.027 |
| Creatinine ≥ 0.65 mg/dl | 5.47 | 0.57-52.31 | 0.140 |
| Lactate ≥ 2.5 mmol/l | 1.12 | 0.32-3.85 | 0.857 |
| ScvO2<60% | 3.49 | 0.99-12.29 | 0.051 |
| Positive fluid balance>9% weight 72 hours | 3.91 | 0.98-15.47 | 0.052 |
| AKI | 2.27 | 0.21-24.67 | 0.499 |
OR, odds ratio; 95% CI, 95% confidence interval; PICU, Pediatric Intensive Care Unit; PRISM, Pediatric Risk of Mortality; PELOD, Pediatric Logistic Organ Dysfunction; ScvO2, central venous oxygen saturation; AKI, acute kidney injury.
Septic shock is characterized by increased capillary permeability. Given the need to maintain an acceptable intravascular volume to preserve cardiac output, large quantities of fluids are administered, which contribute to fluid overload and affect multiple organs. In patients with acute lung injury, fluid overload increases the risk of morbidity and mortality.20–23 There is a limited number of pediatrics studies that evaluate fluid overload, acute kidney injury, and septic shock mortality. Bhaskar et al.20 conducted a case-control study nested in a cohort to evaluate the association between fluid overload and mortality in children going into shock. Mortality was higher in the group with fluid overload (26% in the group with overload compared to 6% in the group without fluid overload, p=0.03). In this sample, 114 patients with shock from different etiologies were included. In contrast, the present study included only children with septic shock with very similar baseline characteristics; fluid balance and overload were significantly higher, and values were statistically significant in univariate analysis in patients who did not survive.20 These findings differ with data reported by Sinitsky et al.22, who studied a retrospective cohort with 636 patients with different diagnoses. (The most prevalent were from a respiratory origin, with 59%). The purpose of this study was to explore the association of fluid overload during the first 48hours of invasive ventilation with the ventilation period and the mortality.
Fluid overload was significantly associated with patients who did not survive and had the following characteristics: PRISM with a high score, younger age, patients requiring vasopressors, patients with continuous renal replacement therapy, high oxygenation index at 48hours, and days of invasive ventilation. No significant association between the percentage of fluid overload and mortality was found. In this study, organic failure was not evaluated, and no patients with septic shock were included. Abulebda et al.15 conducted a multicenter retrospective study in 17 intensive care units to assess the association between fluid balance and mortality risk stratified into three categories (low, intermediate, and high) with a validated scale called PERSEVERE (PEdiatRic SEpsis biomarkEr Risk modEl)—in a very heterogeneous group of 317 patients with septic shock. The authors evaluated fluid balance during the first 24hours, accumulated fluid balance in 7 days and mortality within 28 days in all three categories. Fluid overload was most often associated with mortality in only the low-risk group, with a marginal result to consider it a risk (OR 1.035; 95% CI 1.004-1.066, p=0.024). Patients who did not survive were younger, with a more severe disease, renal failure, and with fluid overload and balance at 24hours. The results of this study are similar those obtained in this research, except age, which was not homogeneous in both study groups.
Sepsis and septic shock are the leading causes of AKI and this association dramatically increases mortality, especially in patients with fluid overload. Fluid overload and oliguria in patients with septic shock were important factors in the increased mortality at 28 days.24–29 Li et al.24 conducted a study in a prospective cohort for eight months in a PICU to assess the impact of fluid overload during the first 24hours of admission on the development of AKI and mortality. Among a sample of 370 patients, they reported a mortality of 15.6% to the patients with fluid overload versus 2.6% in the group of patients without fluid overload; 18.8% on patients with AKI versus 4.2% with no AKI (p<0.001). In this study, a significant sample included patients with a wide diagnostic heterogeneity. The septic patient sample was reduced: 28 patients without overload and ten patients with fluid overload. These results matched with this study at 72hours, where a statistically significant association between fluid overload and AKI was found in the univariate analysis but not in the multivariate analysis.
Liquids are the cornerstone in the treatment of patients in a critical condition. Although the benefits of acute and early fluid resuscitation in patients with septic shock and AKI have been accepted, doubts about the benefits of aggressive fluid resuscitation in these patients exist with the available information. Uncertainty lies mainly in liquid volume, its characteristics, and time of administration. An association between fluid overload and increased risk of AKI and mortality has been observed. In a study in 30 intensive care units with a sample of 2526 patients, Wang et al. reported an incidence of AKI during the first 72hours in 1172 patients (46.3%); fluid overload increased 4.5 times the risk and severity of AKI.29
The fact that fluid overload is associated with AKI does not prove a cause-effect relationship. In patients with severe sepsis, AKI and fluid overload share the same effects at the endothelial level due to an inflammatory response, an ischemic process or an ischemia-reperfusion injury; as a result, a capillary leak and multiple organ failures may present. Therefore, the patients in a more severe state have a more severe endothelial damage and develop a faster fluid overload and an AKI after the liquid administration.
The limitations of the present study are those of a retrospective study that does not guarantee the accuracy of the data from the clinical record, besides not ensuring homogeneity, representativeness and simultaneity of cases and controls. Although all patients received vasopressors and mechanical ventilation assistance, homogeneity is not guaranteed. The main limitation is that the volume and fluid balance before the admission to the PICU were not considered.
The statistical inference to other PICU is limited; the sample was not probabilistic for convenience, and although the sample size was calculated by the difference in proportions, data was obtained from a PICU with a different mortality rate. Based on the preceding, it is considered that the outcome could change onwards the statistical association between fluid balance>9% and mortality in patients with septic shock by increasing the sample size.
In conclusion, the multivariate model found a significant association between the risk of mortality and organ dysfunction, assessed by the PRISM III and PELOD, respectively, in patients who died from septic shock. Also, there is a tendency of association between ScvO2<60% and the positive fluid balance>9% at 72hours with mortality in patients with septic shock. However, no statistically significant difference was found due to the sample size.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
FundingThere was no external funding. The authors funded expenses arising from this research.
Conflict of interestsThe authors declare no conflicts of interest of any nature.
Please cite this article as: Martínez-García JJ, León-Sicairos NM, Canizalez-Román A, García-Arellano BA. Balance de líquidos y lesión renal aguda en el choque séptico. Bol Med Hosp Infant Mex. 2017;74:282–288.