New Delhi metallo-β-lactamase producing Enterobacteriaceae are a serious threat to the public health sectors worldwide. NDM producing pathogens generally display resistance against several different classes of antibiotics including carbapenems; considered last resort to treat infections caused by such pathogens.1,2 Until now 19 NDM variants (NDM-1 to NDM-19) have been identified from different parts of the world http://www.lahey.org/Studies/other.asp. NDM-4 differs from NDM-1 by a single point mutation at position 154 (M–L) and is associated with high carbapenemase activity.3 We are first time reporting the description of NDM-4 producing Escherichia coli isolated from urine sample in Pakistan.
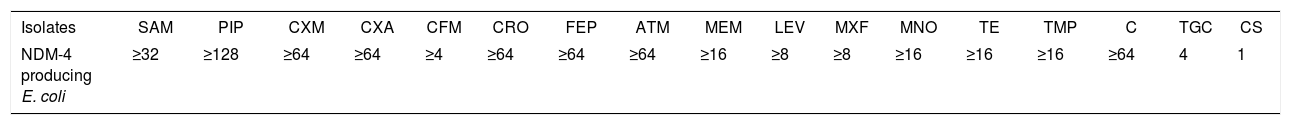
A 4-year-old female patient was hospitalized in a tertiary care hospital Lahore, Pakistan in March 2014. After admission, her urine culture revealed the presence of E. coli which was confirmed by VITEK® 2 system (bioMerieux, France) and MALDI-TOF (Bruker, Germany). Isolate was also carbapenemase and metallo-β-lactamase producer identified by modified Hodge's test and double disk synergy method respectively.4 Minimum inhibitory concentration (μg/mL) of antibiotics using GN XN05 card in VITEK® 2 compact system (bioMerieux, France) displayed pan-drug resistance to commonly used antibiotics including meropenem and only effective drug was colistin. Furthermore, colistin susceptibility was determined by broth microdilution assay in 96 microtiter Plate5 (Table 1). A previous study reported that NDM-4 producing bacteria has higher MIC (μg/mL) and hydrolytic activity as compared to NDM-1 producing bacteria.3 Genotyping of blaNDM-4 was accomplished by PCR (NDM-F-TGGCTTTTGAAACTGTCGCACC, NDM-R- CTGTCACATCGAAATCGCGCGA) and DNA sequence analysis. Plasmid characterization was performed as previously reported.4 S1 nuclease pulse field gel electrophoresis and in gel DNA hybridization revealed the presence of blaNDM-4 on 120kb of plasmid (data not shown). As per Carratoli6 procedure of plasmid typing, the isolate contained the Incompatible FII group of plasmids. Multilocus sequence typing (MLST) was performed as described earlier and E. coli belonged to the sequence type (ST) 405.7 ST405 NDM producing E. coli has also been isolated from two inpatients in Italy.8 It is documented that the Indian sub-continent is the main reservoir and source of NDM producing bacteria globally. Present study also supported this fact in that the patient had no previous travel history. Moreover, NDM-4 producing E. coli has also been reported from different parts of the world including India and Italy.3,8 This study indicates, the emergence of NDM-4 producing E. coli ST405 which can lead to therapeutic failure and deaths particularly in children. This isolate could be transferred through risk factors such as bed sharing, substandard infection control practices and most importantly urinary catheters.
MIC (μg/mL) of NDM-4 producing Escherichia coli.
| Isolates | SAM | PIP | CXM | CXA | CFM | CRO | FEP | ATM | MEM | LEV | MXF | MNO | TE | TMP | C | TGC | CS |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| NDM-4 producing E. coli | ≥32 | ≥128 | ≥64 | ≥64 | ≥4 | ≥64 | ≥64 | ≥64 | ≥16 | ≥8 | ≥8 | ≥16 | ≥16 | ≥16 | ≥64 | 4 | 1 |
SAM: ampicillin/sulbactam, PIP: piperacillin, CXM: cefuroxime, CXA: cefuroxime axetil, CFM: cefixime, CRO: ceftriaxone, FEP: cefepime, ATM: aztreonam, MEM: meropenem, LEV: levofloxacin, MXF: moxifloxacin, MNO: minocycline, TE: tetracycline, TMP: trimethoprim, C: chloramphenicol, TGC: tigecycline, CS: colistin.
The blaNDM containing IncFII plasmids might have become the common vehicle for the spread of various NDM alleles among Enterobacteriaceae. Furthermore, they could also play a relevant role in the spread of such strains and other resistance genes, especially if the isolate is present as part of the dominant microbiota and the hygienic conditions are suboptimal particularly in low-resource settings.
Nucleotide sequence accession number: The nucleotide sequence of blaNDM-4 producing E. coli strain has been deposited in the BankIt/GenBank/NCBI data base under accession number KY912035.
FundingWe are thankful to Higher Education Commission (HEC), Pakistan for approving research grant (Number: 20-3742/NRPU/R&D/HEC/14/430) and International Research Support Initiative Program (IRSIP) fellowship for School of Medicine, Cardiff University, Cardiff, United Kingdom.
Conflicts of interestAll authors declared that there is no conflict of interest.