To identify the prevalence of metabolic syndrome in children with overweight risk, overweight or obesity.
MethodsOverweight risk, overweight and obesity were determined using body mass index for age, based on the WHO cut-off values. Metabolic syndrome was diagnosed using the modified Adult Treatment Panel III (ATP III) criteria for adolescents. Children were selected from public elementary schools in the south of Mexico City. A total of 398 children with a mean age of 11.7 (±0.9) years participated.
ResultsThe proportions of children with overweight risk, overweight and obesity were 23.8%, 17.5% and 3.5%, respectively. Although a higher percentage of girls than boys showed overweight risk, there were more boys than girls in the overweight and obese categories (P<.001). Overall, 22.6% of children exhibited metabolic syndrome, with a higher percentage of boys than girls (28.3% vs. 17.1%) (P<.001); 24.8% of the schoolchildren met two of the metabolic syndrome criteria and were classified as being at risk for metabolic syndrome. A higher percentage of girls than boys (28.5% vs. 20.9%) (P<.001) were in this category. Among children at risk of overweight, overweight and obese, 21.8%, 30.6% and 44.4%, respectively, had metabolic syndrome, and 25.4%, 30.6% and 55.5% (P<.001) respectively, were at risk of metabolic syndrome (P<.001). Children who were of normal weight did not have metabolic syndrome nor were at risk for the syndrome.
ConclusionsHigher body mass index was associated with a higher prevalence of metabolic syndrome. The deleterious consequences of metabolic syndrome highlights the need for intervention programs for overweight and obese children with particular emphasis on male population.
Identificar la prevalencia de síndrome metabólico en niños con riesgo de sobrepeso, sobrepeso y obesidad.
MétodosEl riesgo de sobrepeso, sobrepeso y obesidad fueron determinados con el índice de masa corporal para la edad, con base en los puntos de corte de la OMS. El síndrome metabólico fue diagnosticado usando los criterios del Adult Treatment Panel III (ATP III) modificados para niños y adolescentes. Los niños fueron seleccionados de escuelas primarias públicas en el sur de la Ciudad de México. Se incluyeron 398 niños con una edad promedio de 11.7 (± 0.9) años.
ResultadosLos porcentajes observados de niños con riesgo de sobrepeso, sobrepeso y obesidad fueron 23.8%, 17.5% y 3.5%, respectivamente. Un mayor porcentaje de niñas presentaron riesgo de sobrepeso que los niños (p < 0.001); en el sobrepeso y la obesidad tuvieron los niños prevalencia más alta que las niñas (p < 0.001). 22.6% de los niños exhibieron síndrome metabólico, con mayor prevalencia en hombres que en mujeres (28.3% vs 17.1%) (p < 0.001). 24.8% de los escolares mostraron dos criterios de SM y fueron clasificados en riesgo de síndrome metabólico, con porcentajes más altos en las niñas (28.5%) que los niños (20.9%) (p < 0.001). Se observó que en el grupo de niños con riesgo de sobrepeso, sobrepeso y obesidad 21.8%, 30.6% y 44.4%, respectivamente, presentaron síndrome metabólico y 25.4%, 30.6% y 55.5%, respectivamente, mostraron riesgo de síndrome metabólico (p < 0.001). En el grupo de niños con peso normal no se detectaron casos de síndrome metabólico ni riesgo de síndrome metabólico.
ConclusiónEl aumento del índice de masa corporal fue asociado con el aumento de la prevalencia de síndrome metabólico. Las consecuencias perjudiciales del síndrome metabólico resaltan la necesidad de programas de intervención para niños con sobrepeso y obesidad, con especial énfasis en la población masculina.
Obesity (OB) is the result of body fat accumulation and has serious health implications.1,2 Obesity is now considered a pandemic and is one of the most pressing health problems worldwide due to its rapidly increasing prevalence in recent years.3,4 In Latin America, more than two-thirds of the population has overweight (OW).3 In the USA, 23.9 million children between 2 and 19 years of age were overweight or obese; furthermore, a comparison of the prevalence of obesity in 1973-1974 and 2008-2009 showed that the proportion of obese children aged between 5 to 17 years was five-fold higher in 2008. In addition, obesity is more prevalent among children who live in families with higher unemployment, lower income and lower education levels.5 Approximately 70% of obese adolescents become obese adults.6
In Mexico, the National Health and Nutrition Survey (2012) showed that 35.0% of adolescents (35.8% of females and 34.1% of males) were OW or OB. Among female adolescents, there was a higher proportion of OW (23.7%) than among males (19.6%). The opposite is true for OB: a higher percentage of male adolescents than females are obese (14.5% vs. 12.1%).7 Currently, Mexico is ranked first worldwide in childhood obesity and second in adult obesity.8,9
This rapid increase in OB is of great concern because it is a risk factor for several chronic diseases, including type 2 diabetes, insulin resistance, hypertension, hyperlipidemia and various types of cancer.2,10,11 In Mexican adolescents with OW and OB, 0.7% have type 2 diabetes and 1.8% suffer hypertension. Both of these conditions are more common in females.7 These diseases lead to a significant loss of healthy life years and are responsible for a large proportion of premature deaths, which impose a heavy economic burden on health services and society.12
Metabolic syndrome (MS) is a complex clinical condition that is associated with insulin resistance and several cardiovascular risk factors. People with higher levels of central body fat develop MS more frequently than those with a peripheral body fat distribution. MS is characterized by hyperglycemia, dyslipidemia and high blood pressure (BP).13–15
Adults with MS have a higher risk of coronary heart disease stroke and diabetes.14,15 In addition, MS is more prevalent in the Americas and the Middle East than in Europe and the Far East. In the Americas, MS is predominantly found in Hispanic populations; it has been reported to be more common in urban areas, and it has been associated with poverty. There are several criteria for diagnosis of MS. Among the most widely used diagnostic criteria are those proposed by the Adult Treatment Panel III (ATP III), the World Health Organization (WHO) and the International Diabetes Federation (IDF). The cutoff values depend on age and sex for children and adolescents.16
The objective of the present study was to identify the prevalence of MS in schoolchildren who were at risk of being overweight (OWR), OW or obese in elementary schools in the south of Mexico City.
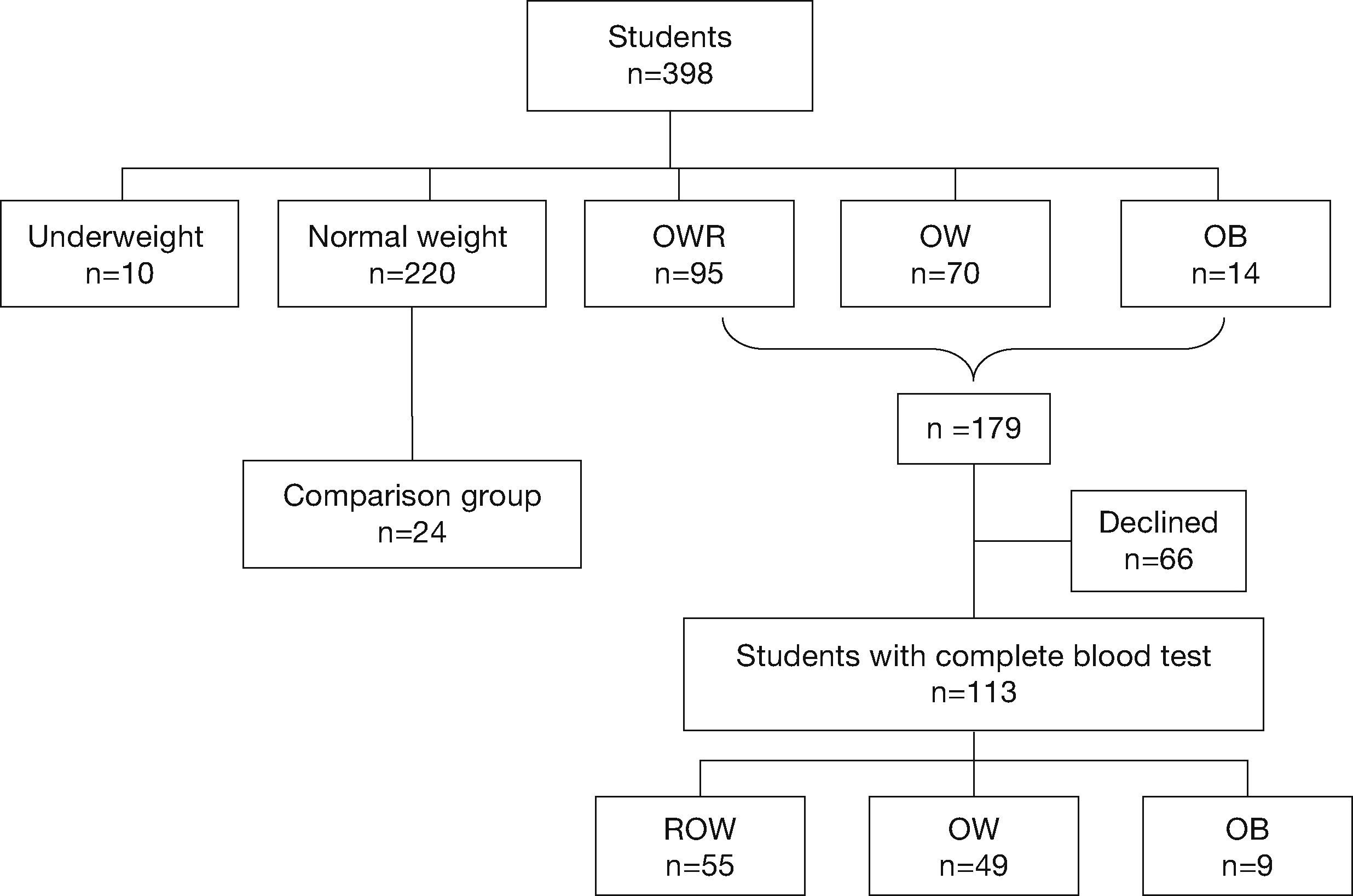
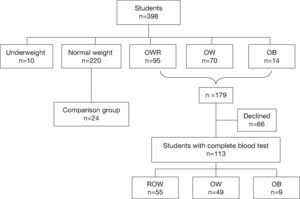
MethodsA cross-sectional study was performed from March 2013 to February 2014. Five elementary schools associated with the “Nayaritas” Community Health Center (Coyoacán, Mexico City) were selected. These schools were located in an urban area of low socioeconomic status. The heights and weights of all children enrolled in the fifth and sixth grades (n=398 children) were measured following standard techniques.17 Overall, 179 children were classified with OWR, OW or OB. Biochemical tests were conducted on 113 children. Additionally, a group of children with normal body mass index (BMI) were included in the study (n=24) (Fig. 1).
Inclusion criteria were as follows: children in fifth or sixth grade of either sex showing OWR, OW and OB, whose parents agreed to biochemical testing being carried out on their children, and who were present at school on the blood-sampling days, and for the comparison group normal weight children were included.
Exclusion criteria were as follows: presence of infectious diseases, autoimmune diseases, heart diseases, type 2 diabetes or any endocrine disease, or not having fasted for a period of 8 to 12hours prior to blood sampling.
Authorization from a parent or legal guardian was obtained before performing any evaluation on the children. The Research Ethics Committees of the Metropolitan Autonomous University Xochimilco, the Autonomous University of Campeche, and the “Nayaritas” Community Health Center and Authorities of five elementary schools approved the study protocol.
AnthropometryMedical interns were trained to perform the anthropometric evaluation; weight, height and waist circumference (WC) were recorded. Measurements were performed according to the WHO recommended techniques.17 Height was measured using a SECA 213 stadimeter (Hamburg Deutschland, Germany) with a 0.1cm precision. Body weight was recorded with a SECA Cursa 818 electronic scale (Hamburg, Deutschland, Germany) with a precision of 0.1kg. Waist circumference (WC) was measured with a SECA 201 measuring tape.
For the anthropometric analysis, the Anthro Plus program (WHO) was used to obtain the Z-score body mass index (BMI)-for-age and sex. The diagnoses of being at risk of being OW, OW and OB were obtained using the Z-score with cut-off points as proposed by the WHO.17
Biochemical variablesCapillary blood samples were used for biochemical testing; the Alere Cholestech LDX System and the Lipid profile-glucose (GLU) (Orlando, Florida, USA) were utilized to determine the concentrations of total cholesterol (TC), high-density lipoprotein (HDL), triglycerides (TG), low-density lipoprotein (LDL) and glucose (GLU). Additionally, the children's blood pressure (BP) was taken twice on the sampling day.
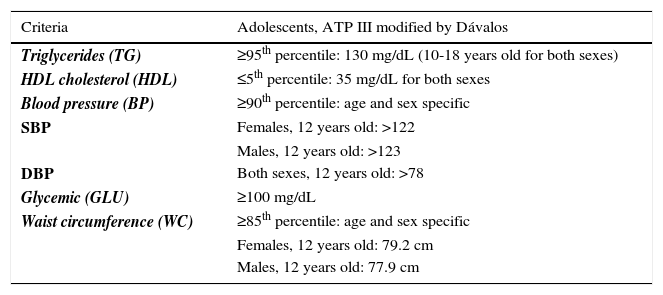
MS was diagnosed based on the National Cholesterol Education ATP III criteria modified for Mexican adolescents. Participants meeting three or more criteria were diagnosed with MS.18 Children meeting two MS criteria were listed as being at risk of MS (MSR) (Table 1).
ATP III criteria modified for adolescents
| Criteria | Adolescents, ATP III modified by Dávalos |
|---|---|
| Triglycerides (TG) | ≥95th percentile: 130 mg/dL (10-18 years old for both sexes) |
| HDL cholesterol (HDL) | ≤5th percentile: 35 mg/dL for both sexes |
| Blood pressure (BP) | ≥90th percentile: age and sex specific |
| SBP | Females, 12 years old: >122 |
| Males, 12 years old: >123 | |
| DBP | Both sexes, 12 years old: >78 |
| Glycemic (GLU) | ≥100 mg/dL |
| Waist circumference (WC) | ≥85th percentile: age and sex specific |
| Females, 12 years old: 79.2 cm | |
| Males, 12 years old: 77.9 cm |
SBP: Systolic Blood Pressure; DBP: Diastolic Blood Pressure.
Source: Dávalos.18
The data are presented as the average and standard deviation for continuous variables and as percentages for categorical variables. Pearson's chi-square test was used to compare variable categories. Analysis of variance (ANOVA) was performed and logistic models were generated to evaluate the association between the presence of MS and anthropometric and biochemical variables. A p-value <0.05 was considered statistically significant. Statistical analysis was performed using JMP software (SAS Institute Inc, USA).
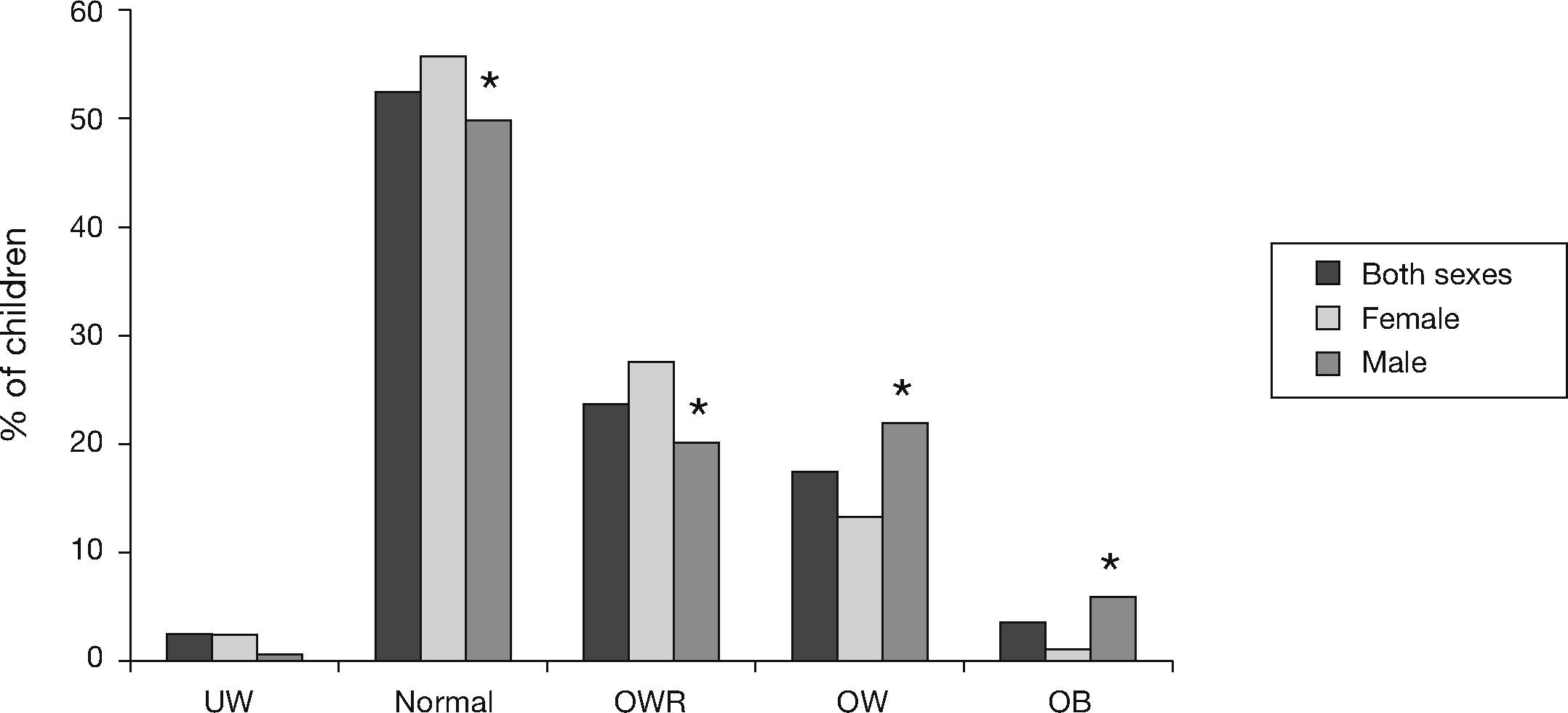
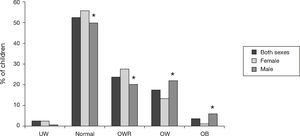
ResultsA total of 398 students participated in the first phase of the study, with an average age of 11.7 (±0.9) years; 51% were females (n=203) and 49% were males (n=195). Overall, 44.8% of the students were at risk of being OW, OW or obese. According to the BMI-for-age, 52.5% (n=209) of the children had normal weight and 23.8% (n=95) were at OWR, with a higher prevalence among girls than boys (27.6 vs. 20%; p<0.001). Of the students, 17.5% (n=70) were OW, with a higher prevalence among boys than girls (22.1 vs. 13.3%; p<0.001). OB was detected in 3.5% (n=14) of the children, with a higher percentage among boys than girls (6.7 vs. 0.5%; p<0.001). The percentage of underweight students was the same in both boys and girls (2.5%, n=10) (Fig. 2).
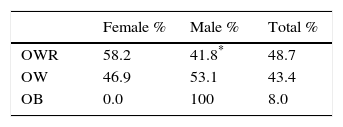
In this step, 137 students were included: 70 girls (50.4%) and 67 boys (49.6%). In children with high BMI, 48.7% (n=55) were at OWR, 43.4% (n=49) were OW and 8.0% (n=9) were obese. In the OWR group, there was a higher percentage of girls than boys (p<0.009). In contrast, for the OW group, the percentage of boys was higher than of that of girls (p<0.009), and there were only male students in the OB group (Table 2).
Nutritional status of the group that underwent biochemical testing, according to BMI for age
| Female % | Male % | Total % | |
|---|---|---|---|
| OWR | 58.2 | 41.8* | 48.7 |
| OW | 46.9 | 53.1 | 43.4 |
| OB | 0.0 | 100 | 8.0 |
OWR: overweight risk; OW: overweight; OB: obese.
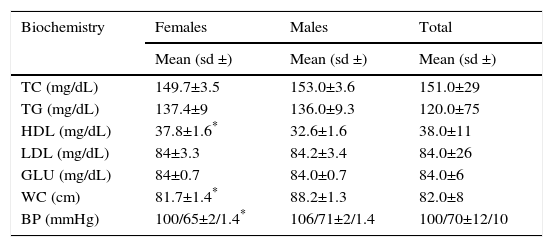
In terms of WC and BMI, 52.7% of the children who were at OWR had a WC equal to or above the 85th percentile. Overall, 85.7% of the OW and 100% of the OB children had a WC above the 85th percentile (p<0.0001). For normal weight children, 95.8% had a WC below the 85th percentile. The averages of the biochemical tests were as follows: TC: 151(±29) mg/dL; TG: 120 (±75) mg/dL; HDL: 38 (±11) mg/dL; LDL: 84 (±26) mg/dL, and GLU: 84 (±6mg/dL). The average WC was 82 (±8) cm and the average BP was 100/70 (±12/10). Significant differences were observed by sex for HDL, with higher levels in females than in males (p<0.02). Males had a larger WC than females (p<0.001). The HDL and WC variables were above normal values according to sex and age. In the case of BP, males had higher values than females (p<0.02); the BP averages were within the normal limits in males and females (Table 3).
Means of biochemical tests, waist circumference and blood pressure in Mexico City elementary schoolchildren by sex
| Biochemistry | Females | Males | Total |
|---|---|---|---|
| Mean (sd ±) | Mean (sd ±) | Mean (sd ±) | |
| TC (mg/dL) | 149.7±3.5 | 153.0±3.6 | 151.0±29 |
| TG (mg/dL) | 137.4±9 | 136.0±9.3 | 120.0±75 |
| HDL (mg/dL) | 37.8±1.6* | 32.6±1.6 | 38.0±11 |
| LDL (mg/dL) | 84±3.3 | 84.2±3.4 | 84.0±26 |
| GLU (mg/dL) | 84±0.7 | 84.0±0.7 | 84.0±6 |
| WC (cm) | 81.7±1.4* | 88.2±1.3 | 82.0±8 |
| BP (mmHg) | 100/65±2/1.4* | 106/71±2/1.4 | 100/70±12/10 |
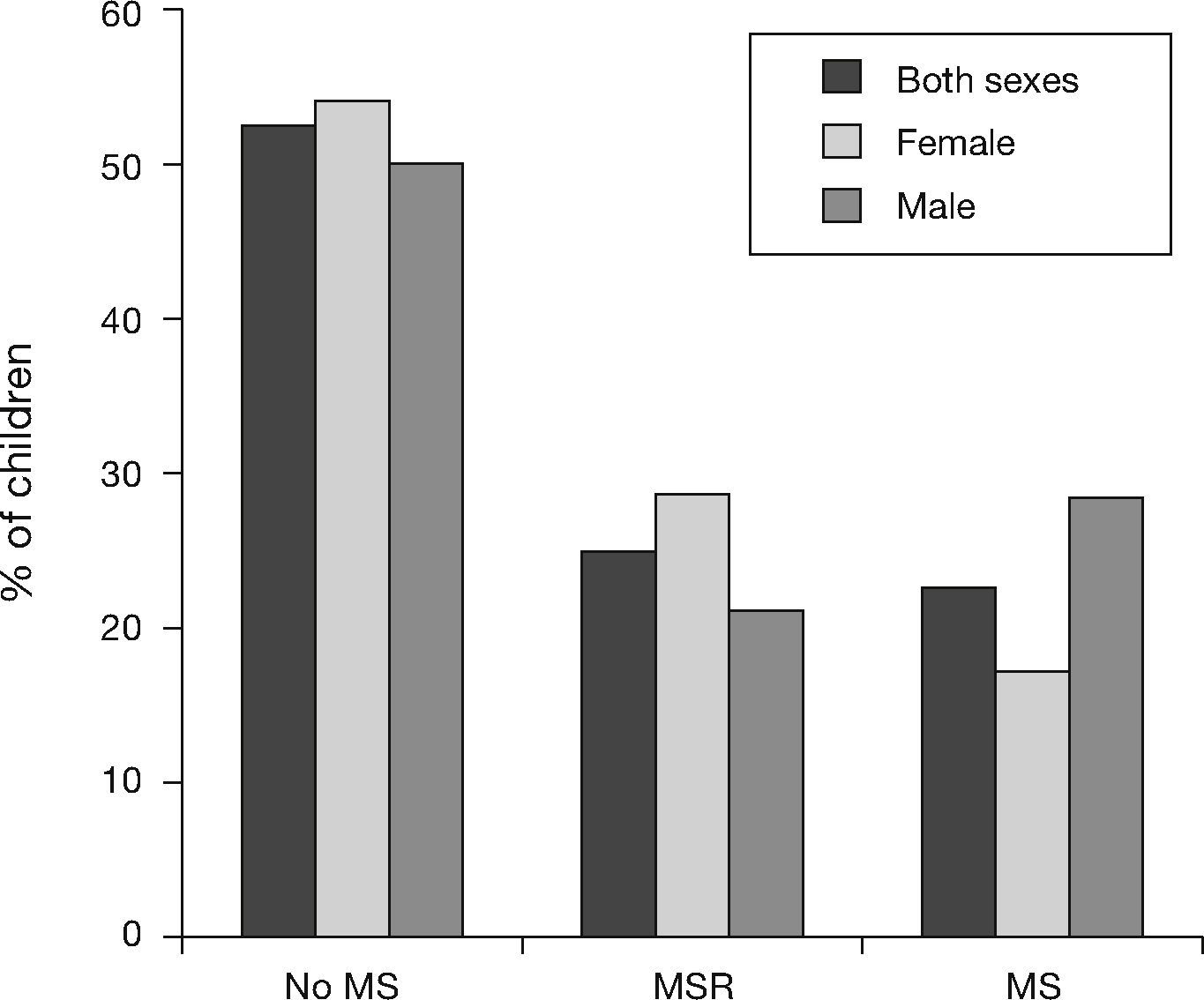
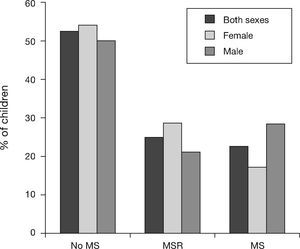
According to the ATP III criteria modified for adolescents, 52.5% (n=72) of the children did not have MS, 24.8% (n=34) of the children were at risk of MS (MSR), and 22.6% (n=31) of the children exhibited MS, in boys 28.4% and in girls 17.1%. 28.6 of the boys and 20.9% of the girls were in the MSR category, although no statistically significant differences were observed between MS categories by sex (Fig. 3).
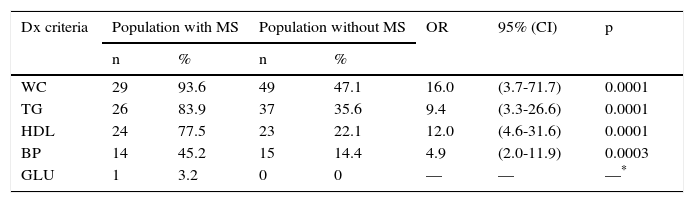
Among children with MS and those without MS, the indicators in addition to WC were high TG, low HDL and high BP. Children with MS had a WC above the 85th percentile, high TG, low HDL and high BP. All of these results were statistically significant (Table 4).
Number and percentage of children with metabolic syndrome meeting the different diagnostic criterion in Mexico City elementary schoolchildren
| Dx criteria | Population with MS | Population without MS | OR | 95% (CI) | p | ||
|---|---|---|---|---|---|---|---|
| n | % | n | % | ||||
| WC | 29 | 93.6 | 49 | 47.1 | 16.0 | (3.7-71.7) | 0.0001 |
| TG | 26 | 83.9 | 37 | 35.6 | 9.4 | (3.3-26.6) | 0.0001 |
| HDL | 24 | 77.5 | 23 | 22.1 | 12.0 | (4.6-31.6) | 0.0001 |
| BP | 14 | 45.2 | 15 | 14.4 | 4.9 | (2.0-11.9) | 0.0003 |
| GLU | 1 | 3.2 | 0 | 0 | — | — | —* |
WC: waist circumference; HDL: high-density lipoprotein; TG: triglycerides; BP: blood pressure.
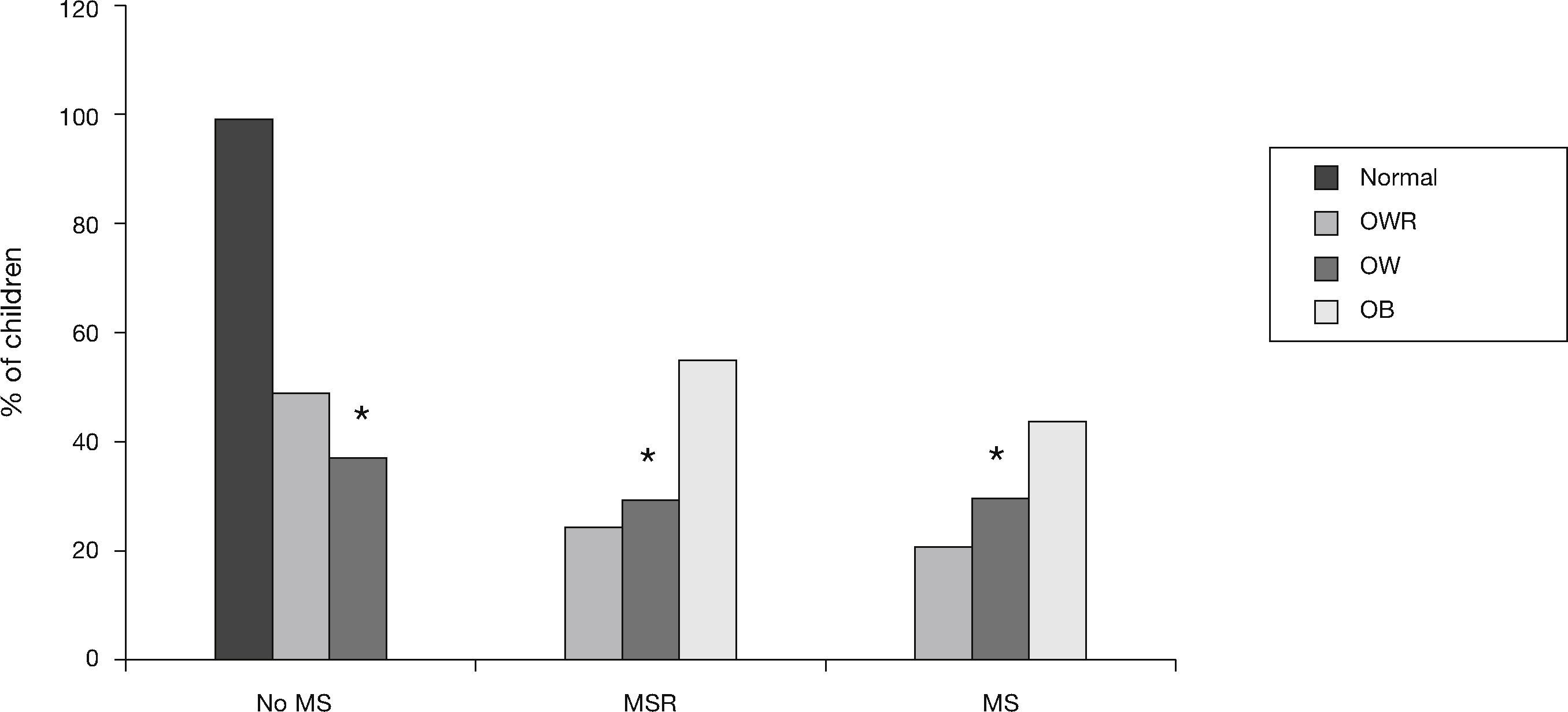
In addition, among children who were at OWR, 21.8% and 25.4% had MS and MSR, respectively. In the OW children, 30.6% exhibited MS and 30.6% exhibited MSR. Among the obese children, 44.4% had MS and 55.5% had MSR. In the group of normal weight children, none had MS or MSR. All of these results were statistically significant (Fig. 4).
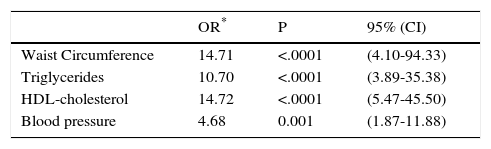
Logistic regression analysis showed that children with a WC above the normal parameters were 16 times more likely to have MS (p<0.0001). Furthermore, the children with high TG were 9.4 times more likely to have MS (p<0.0001); children with low HDL (p<0.0001) and high BP (p<0.002) were 12 and 4.9 times more likely to have MS, respectively (Table 5).
Metabolic syndrome adjusted odds ratios (OR) for age and sex and WC, TG, HDL and BP in Mexico City elementary schoolchildren
| OR* | P | 95% (CI) | |
|---|---|---|---|
| Waist Circumference | 14.71 | <.0001 | (4.10-94.33) |
| Triglycerides | 10.70 | <.0001 | (3.89-35.38) |
| HDL-cholesterol | 14.72 | <.0001 | (5.47-45.50) |
| Blood pressure | 4.68 | 0.001 | (1.87-11.88) |
The results of the present study show that a high percentage (44.8%) of children were classified as at OWR, OW, or obese. There was a higher percentage of girls than boys in the OWR category, whereas in the OW and OB groups, the percentage of girls was lower than that of boys. The sum of the percentages of OWR, OW and OB in our study is above those reported by the National Health and Nutrition Examination Survey (34.4% of children from 5 to 11 years of age). In a study performed in children from 6 to 13 years of age in Mexico City, there was a high prevalence of OW and obese children (48.5%). Regarding the OW data by sex, a higher percentage of girls than boys (20.2 vs. 19.5%) was recorded. Regarding OB, the same study found a higher percentage of boys than girls (17.4 vs. 11.8%) with this condition.19 These data agree with what we found in terms of OWR and OW, which has been previously diagnosed as OW and OB, respectively.
In OWR, OW and obese children, MS prevalence was 22.6%, with higher percentages in boys than in girls and 24.8% of the students were at risk of MS (i.e., the children had two signs of MS, established in the ATP III criteria). In a previous study performed in adolescents and young Mexican adults (7-24 years old) in the center of the country, the prevalence of MS for all subjects was 19.2%, using the ATP III criteria; in children between 10-14 years old, the prevalence of MS was higher (28.7%), with no differences by sex.20
The percentage of children 10-12 years old with MS found in our study (22.6%) was lower than that reported above. No significant sex differences were found in either the present or the aforementioned study. In another study of children and young Mexicans (10-19 years) performed in the north of the country, the prevalence of MS was lower (9.4%) than that reported in our study and no differences were found by sex. That study also used the criteria of the ATP III.21 These comparisons indicate that the trends related to MS in children and adolescents in Mexico most likely differ by geographic region, and it is related to socio-economic factors.
In a review of articles on MS covering the period 2007-2009, the prevalence of MS in the pediatric population worldwide ranged from 1.2% to 22.6%. Most likely, such variability results, at least in part, from the use of different diagnostic criteria applied in these studies. The average prevalence of metabolic syndrome in the above-mentioned studies was 11.9% in OW and 29.2% in obese children.16 It should be noted that the categories of OW and OB in the former study correspond to OWR and OW in the present study, respectively. In the present study, 21.8% of children who were at risk of being overweight had MS, along with 30.6% of overweight children and 44.4% of obese children; MS prevalence increased with higher BMI scores. These percentages are well above the average values reported internationally; however, they are similar to the values previously reported in Mexican children (33.3%), and both studies were based on the same criteria of the NCEP-ATP III.22
The high prevalence of MS among study participants suggests that children will be more likely to develop diabetes mellitus and cardiovascular diseases at a younger age.12 These increase the likelihood of disability and premature death.23
The higher prevalence of MS among boys than girls found in the present study may decrease because girls comprised the highest percentage of children in the MSR category. With time (age), the gender gap could disappear if the necessary preventive interventions are not taken.
In 3- to 13-year-old Argentine children, variations were found in the prevalence of MS according to diagnostic criteria as follows: 15% (ATP III), 18% (WHO) and 14% (European Group for the Study of Insulin Resistance, EGIR). In this work, in addition to central obesity, abnormal lipid profile, particularly hypertriglyceridemia and decreased HDL, were found.24 In another study on the prevalence of MS in obese 3 to 18-year-old Mexican children living in the northern part of the country, the frequency of metabolic syndrome was 37.1%, and it was higher for females (44.4%) than for males (32.7%). By age group, the prevalence of MS was higher in school-aged children and adolescents (38.5% and 38.9%, respectively) than in preschool children (22%). In obese children, the study showed two biochemical indicators: decreased HDL (60%) and hypertriglyceridemia (51.5%).25
In another study of MS in children in the central region of Mexico, the main signs of MS were low HDL (86.9%), high triglycerides (48.3%) and waist circumference above the 85th percentile.20 In the present study, children with MS had a waist circumference above the 85th percentile, higher triglycerides and low HDL (p<0.001). The results of this study are consistent with those of previous studies and confirmed that major changes occurring in children with MS were associated with the lipid profile.
Facing this scenario concerning the presence of metabolic syndrome in schoolchildren, health policy should be geared toward weight control and increased physical activity in children. Both objectives would facilitate lowering insulin resistance and improving glucose tolerance and other risk factors for cardiovascular disease, such as decreased triglycerides and blood pressure.13 Additionally, studies on lifestyle changes have shown that the components of metabolic syndrome could be significantly reduced, especially when applying long-term programs.26,27
ConclusionsOur results showed a high prevalence of being at risk of OW, OW and OB in children. Additionally, we observed a high prevalence of children with metabolic syndrome, and high BMI levels were strongly associated with MS. Strong measures are required to reduce BMI levels and MS due to the serious consequences that these conditions have in children from a young age and the negative impact on the loss of healthy years in the Mexican population.
Conflict of interestThe authors have no conflicts of interest to declare.
The authors acknowledge the medical doctors, Karina Ramírez Navarro and Patricia Solís Chávez, for their participation in obtaining anthropometric measurements from the students. The authors also acknowledge funding from a grant (34511059) from the Chronic Degenerative Processes (UAM-X-CA-5) Basic Sciences, Health Care Department, through the Overweight and Obesity Network, PROMEP. SEP.