Testicular germ-cell carcinoma is the most frequent neoplasm in males aged 15–35 years old. It is bilateral in 2–3%, and synchronous in 20–25% of the cases.
Clinical caseThe case is presented of a 19 year-old male, with abdominal pain. Physical examination revealed abdominal mass in the umbilical region, and the computed tomography scan showed a retroperitoneal tumor, with α-fetoprotein, lactate dehydrogenase, and human chorionic gonadotropin above limits. Testicular ultrasound showed bilateral lesions. Exploratory laparotomy was performed, identifying an unresectable retroperitoneal tumor. Biopsies were taken, reporting mixed germ cell tumor composed of choriocarcinoma and embryonal carcinoma. Six cycles of chemotherapy were given, based on bleomycin, etoposide and cisplatin, with partial tumor response. Later on, the patient underwent bilateral radical orchiectomy, with pathology reporting a synchronous bilateral testicular teratoma. A second line of chemotherapy was given, based on vincristine, etoposide, ifosfamide and cisplatinum. Nevertheless, the disease progressed, with metastatic dissemination and the patient died.
DiscussionGerm cells tumors can be presented in primary extra-gonadal locations. It is difficult to distinguish a retroperitoneum primary germ cell tumor from metastatic disease of a clinically undetected gonadal tumor or one that has regressed, like the situation described in the case presented.
ConclusionsNinety percent of patients diagnosed with germ cell tumors can be cured. However, delay in diagnosis correlates with an advanced clinical stage and poor prognosis.
El cáncer testicular de células germinales es la neoplasia más frecuente en hombres de 15 a 35 años de edad; es bilateral en el 2 al 3%, y sincrónico en el 20 al 25% de los casos.
Caso clínicoMasculino de 19 años de edad, con dolor abdominal y tumor palpable en mesogastrio. En la tomografía se encontró un tumor retroperitoneal, y por laboratorio se detectó elevación de α-fetoproteína, deshidrogenasa láctica y gonadotropina coriónica humana. En el ultrasonido testicular se identifican lesiones bilaterales. Se realizó laparotomía exploradora, identificándose tumor retroperitoneal irresecable, y se tomaron biopsias incisionales compatibles para tumor de células germinales mixto, con áreas de coriocarcinoma y carcinoma embrionario. Se administraron 6 ciclos de quimioterapia con bleomicina, etopósido y cisplatino, obteniéndose una respuesta tumoral parcial. Posteriormente se realizó orquiectomía radical bilateral, con reporte patológico de teratoma bilateral sincrónico. Se inició segunda línea de quimioterapia con vincristina, etopósido, ifosfamida y platino; sin embargo, la enfermedad progresó, presentando diseminación metastásica y provocando el deceso del paciente.
DiscusiónLos tumores de células germinales pueden presentarse en sitios primarios extragonadales. Es difícil distinguir un tumor de células germinales primario del retroperitoneo, de una enfermedad metastásica derivada de un tumor gonadal no detectado clínicamente, o que ha involucionado, situación que se describe en el caso clínico presentado.
ConclusiónEl 90% de los pacientes diagnosticados con tumor de células germinales pueden ser curados; sin embargo, un retraso en el diagnóstico se correlaciona con una etapa clínica más avanzada y un pronóstico desfavorable.
Testicular germ-cell carcinoma is the most frequent neoplasm in males aged 15–351; it is bilateral in 2–3%, and synchronous in 20–25% of cases.2 Approximately 80% of tumors are seminomas, and the remaining 20% have been identified as mixed teratomas, yolk sac tumors and both pure and mixed embryonal cell carcinomas.3 Most synchronous tumors are of the same histological type.4
Medical records and physical examination are used in the diagnosis of testicular tumors. Generally the tumors present as a painless increase in intrascrotal volume, although 10% of patients present with acute pain. Diagnosis is commonly delayed due to the patient's reluctance to seek medical advice. Scrotal ultrasound testing is the most useful diagnostic tool, with tumor sensitivity in almost 100% of cases.5,6
α-Fetoprotein, lactate dehydrogenase and human chorionic gonadotropin tumor markers both assist diagnosis and enable tumor staging whilst simultaneously serving to aid follow-up and prognosis. They should be determined prior to orchiectomy, one week after surgery, and subsequent to the administration of chemotherapy, due to their kinetics and mean life span.7
Tumor staging is the cornerstone to testicular cancer treatment. Computed tomography should therefore be used to assess probable metastases sites, sensitivity ranges from 70% to 80%.8 10% of patients present with metastasis at the time of diagnosis.9
The aim of this article is to report a case of bilateral synchronous testicular teratoma, the first manifestation of which was a retroperitoneal tumor.
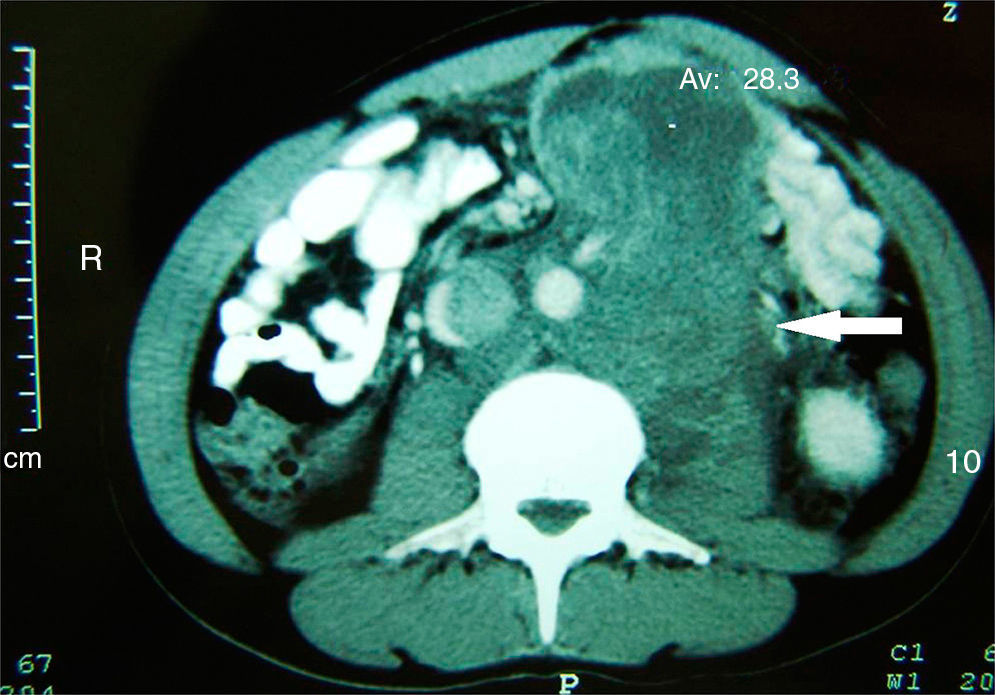
Clinical caseA 19 year-old male, with a family history of testicular cancer presented with sudden abdominal pain in the upper left quadrant. This was a moderate to severe, transfixing pain coming from the left iliac fosse, and was accompanied by repeated bouts of nausea and vomiting. Physical examination revealed a voluminous mesogastrium tumor which extended into deeper locations, and was accompanied by slight pain and no peritoneal irritation; the testicles were clinically with no palpable tumor activity. Abdominal X-rays showed the presence of the tumor and from the contrast-enhanced CT scan of the abdomen and pelvis we were able to determine its retroperitoneal location (Fig. 1).
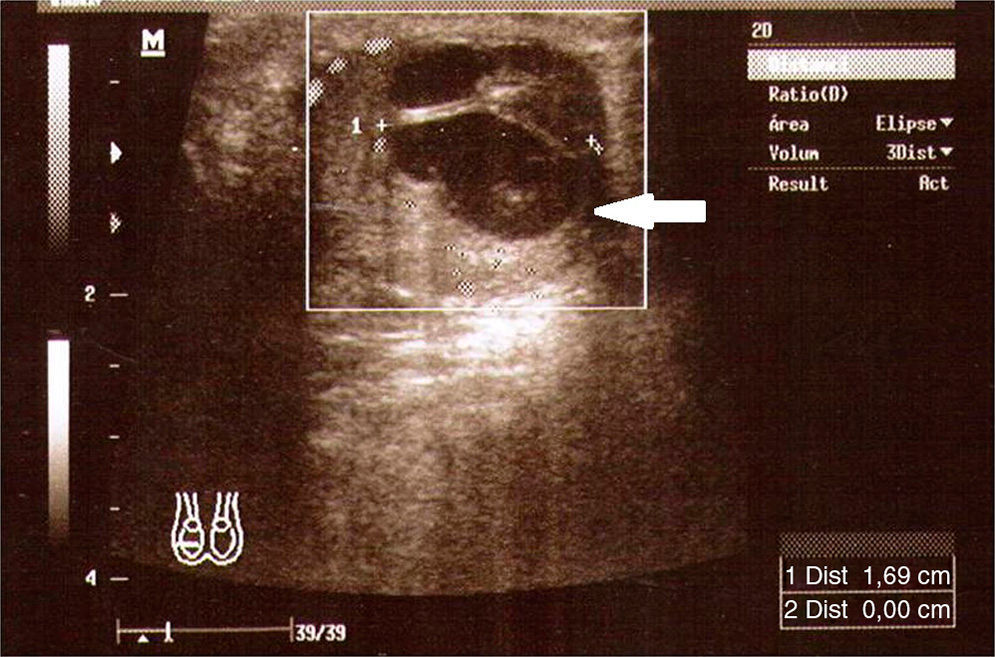
Tumor markers presented with a significantly elevated α-fetoprotein of 32,108.6ng/ml, lactate dehydrogenase of 1184U/l and fractionβ of human chorionic gonadotropin of 10,728mIU/ml. Testicular ultrasound showed a complex bilateral lesion in the right testicle of 20mm, and a solid, hypervascularised lesion of 19mm×15mm (Fig. 2) in the left testicle.
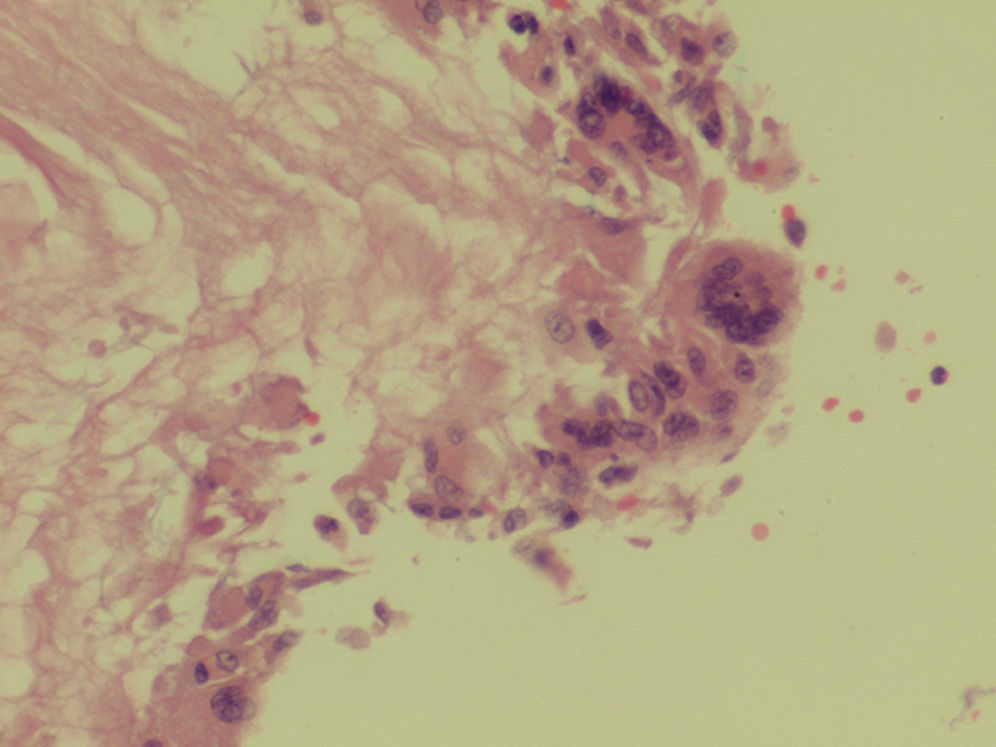
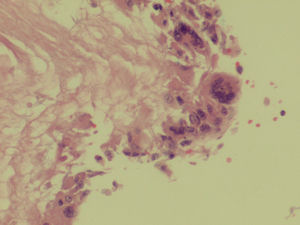
Exploratory laparomoy was performed which revealed highly vascular, retroperitoneal malignancy, which had infiltrated the mesenterium and displaced all intestinal loops. Incisional biopsies were taken of the tumor, reporting mixed germ-cell tumor, with areas of choriocarcinoma and embryonal carcinoma (Fig. 3).
Systemic treatment was initiated and 6 cycles of chemotherapy were administered with bleomycin, etoposide and cisplatin, with partial tumor response. After terminating chemotherapy the patient subsequently underwent bilateral radical orchiectomy with pathology reporting the presence of bilateral synchronous testicular teratoma. Unresectible retroperitoneal disease persisted (Fig. 4).
The patient was administered a second line of chemotherapy, based on vincristine, etoposide, ifosfamide and cisplatinum. Nevertheless, the disease progressed, spreading to the liver and lung, and the patient died 2 years after diagnosis (Fig. 5).
DiscussionGerm cell tumors represent 95% of testicular cancers.10 They are rare diseases which mainly affect young adults and teenagers.11 An estimated 8,590 new cases are detected annually in the United States, with a survival rate of up to 5 years in 96%.12 Malignant testicular tumors rank twelfth in the number of hospital discharges for malignant tumors, according to the data base of the Registro Histopatológico de Neoplasias Malignas in Mexico.13
Identifiable risk factors which predispose the development of germ cell tumors include: a prior history of testicular tumor; a family history of the disease; undescended testicles; testicular dysgenics, and Klinefelter syndrome.14 A change in the short arm of chromosome 12; i(12p) has been identified as a possible cause, and a mutation in gene DAD-R (apoptosis-inducing agent) has also been reported.).15,16
Primary presentation of these tumors may be extra-gonadal in location, due to embryonic origin and testicular descent. It is difficult to distinguish a retroperitoneum primary germ cell tumor from metastatic disease of a clinically undetected gonadal tumor or one that has regressed. This clinical condition is known as tumor burn-out.14 It is important to recall that initial signs of these tumors may be voluminous abdominal metastases, with no primary testicular tumor having been detected. This therefore delays diagnosis and treatment; examination and ultrasound imaging of the testicles are therefore important.
In the clinical case presented, there was no palpable tumor on examination but the doppler ultrasound scan revealed a complex, highly vascular cystic lesion in both testicles. This situation is considered infrequent, given that bilateral synchronous testicular cancer is extremely rare.11,17
Based on the American Joint Committee on Cancer (AJCC) classification scale we could state that our case was a stage IIIC (pTXN3MOS3) when diagnosed.18 There is a risk classification scale for the patient with advanced disease, from the Grupo Colaborativo Internacional de Cáncer de Células Germinales. This classification takes several prognostic factors into account, including histological prognosis, the spread of the disease and the serum levels of the tumor markers, from which 3 risk groups are established: low, intermediate and high.19 In accordance with this classification our patient was in the high risk category.
The presence of an active tumor in the testicles after chemotherapy is a clearly proven fact, with the result that surgical exploration of the testicles and even orchiectomy are options to consider whilst taking into account individual patient characteristics.20 In our case inguinal extraction from the testicle was performed and transoperative tested biopsies were taken. Pathology reported testicular tumor, and we therefore decided to perform bilateral radical orchiectomy.
ConclusionsStatistics show that approximately 90% of patients diagnosed with germ cell tumors can be cured. However, delay in diagnosis correlates with an advanced clinical stage and poor diagnosis.
The clinical evolution of the patient was slow, given the aggressive biological nature of the tumor, and late stage diagnosis. Despite treatment with chemotherapy and bilateral orchiectomy, the disease progressed and the patient died as a result.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Matabuena-Tamez P, Canepa-Fernández P, Valencia-García LC, Gutiérrez-Samperio C, Gallegos-Corona MA. Teratoma testicular bilateral sincrónico: reporte de un caso y revisión de la literatura. Cirugía y Cirujanos. 2015;83:527–531.