Simple nephrectomy is the procedure of choice in the treatment of excluded kidneys. The purpose of this study was to describe and compare surgical results in open simple retroperitoneal nephrectomies in patients with and without nephrostomy.
Methodology58 patients were analyzed. The demographic parameters of patients with nephrostomy were compared to patients without nephrostomy (age, gender, weight, lithium localization, transoperative variables (surgical time, transoperative bleeding) and postoperative variables (need for intensive care, need for transfusion, surgical wound infection and hospital stay days)
ResultsStatistically significant differences were found for the variables of operative bleeding (p=0.0442), surgical time (p=0.0093), hospital stay days (p=0.0040), and transfusion requirements (p=0.0170). There were no differences in the need for intensive care (p=0.6314), transoperative complications (p=0.7414) and surgical wound infection (p=0.2762).
ConclusionsThe presence of a nephrostomy catheter in patients undergoing open simple nephrectomy leads to an increased risk of morbidity, with increased bleeding, surgical time, need for transfusion, and hospital stay days.
La nefrectomía es el procedimiento de elección en el tratamiento de riñones excluidos. La nefrostomía percutánea es una herramienta que permite desobstruir la vía urinaria, asociada a una mayor fibrosis e inflamación perirrenal; el objetivo de este estudio fue describir y comparar los resultados quirúrgicos en nefrectomías retroperitoneales simples abiertas en pacientes con nefrostomía y sin nefrostomía.
MetodologíaSe analizaron 58 pacientes. Los parámetros demográficos de los pacientes con nefrostomía fueron comparados con los pacientes sin nefrostomía (edad, género, peso, localización del lito, variables transoperatorias [tiempo quirúrgico, sangrado transoperatorio]) y variables posquirúrgicas (necesidad de terapia intensiva, necesidad de transfusión, infección de herida quirúrgica y días de estancia hospitalaria)
ResultadosSe encontraron diferencias estadísticamente significativas para las variables de sangrado transoperatorio (p=0.0442), tiempo quirúrgico (p=0.0093), días de estancia hospitalaria (p=0.0040) y necesidad de transfusión (p=0.0170). No existieron diferencias para necesidad de terapia intensiva (p=0.6314), complicaciones transoperatorias (p=0.7414) e infección de la herida quirúrgica (p=0.2762).
ConclusionesLa presencia de un catéter de nefrostomía en pacientes sometidos a nefrectomía simple abierta lleva a un mayor riesgo de morbilidad, con un mayor sangrado, tiempo quirúrgico, necesidad de transfusión y días de estancia hospitalaria.
The first nephrectomy on human beings was performed by William Hingston in the Hotel Dieu Hospital, Montreal, Canada in 1868. However, the results were not published due to an error during the operation which resulted in the patient's death in the operating theatre.1
The first nephrectomy with a good outcome was performed in Heidelberg, Germany, in 1869.1–3 This procedure was better accepted at the beginning of the 19th century. However, it continued to entail high morbidity and mortality, rates as high as 50% were reported.4,5 At the end of the 19th century, with the introduction of asepsis techniques and latex gloves, the number of complications and mortality reduced considerably.6–8 The indications for the placement of a nephrostomy catheter are pyonephrosis, obstruction secondary to lithiasis, urinary tract or metastatic tumours, extrinsic compression, ureteral stenosis or secondary to iatrogenic problems (ureteral ligature). Pyonephrosis secondary to lithiasis can progress rapidly and place the life of the patient in danger, resulting in sepsis and multiple organ failure, requiring immediate drainage and broad antibiotic coverage.9,10
Placement of a nephrostomy catheter creates a connection between the urinary and vascular system, and drains the purulent material from the renal cavities into the perirenal space, which causes sepsis and major local inflammatory response.11 Chronic obstruction of the urinary tract causes a gradual loss of renal function until kidney exclusion occurs, secondary to obstruction of urinary flow and recurrent infections.9
The current treatment of choice to treat an excluded kidney is a simple nephrectomy using the retroperitoneal approach because, since the beginning of the 20th century, it has been recorded that this type of approach carries a lower incidence of complications and mortality.12,13 In our institution open simple nephrectomy using the retroperitoneal approach plays an important role in the treatment of patients with a diagnosis of excluded kidney, of whom a large number have a history of placement of a nephrostomy catheter to treat their obstruction and pyonephrosis.
ObjectiveTo describe the outcomes of open simple nephrectomies using a retroperitoneal approach secondary to lithiases in the Hospital General de México Dr. Eduardo Liceaga and to determine whether patients with a nephrostomy subsequent to nephrectomy have greater surgery time, transoperative bleeding, complications (according to the Clavien-Dindo classification),14 need for transfusion, hospital stay, need for intensive therapy and surgical wound infection than patients without a nephrostomy.
MethodologyThe information used to undertake this study was gathered in a third-level hospital of Mexico City. A search was performed of records from the clinical archive that matched the ICD-9 code for nephrectomy, in the period between January 2010 and May 2016. The data contained in the clinical records was reviewed and gathered. A total of 110 records of patients who had undergone open nephrectomies were assessed, of whom 52 were excluded because they did not have a diagnosis of lithiasis. A total of 58 patients were included with a diagnosis of excluded kidney confirmed by renal scintigraphy, who had undergone a simple nephrectomy in the same institution performed by a group of renal lithiasis specialist surgeons. The retroperitoneal approach by lumbotomy was used in all the patients, and they all received antibiotic cover at the time of surgery.
A descriptive, cross-sectional and comparative study was performed. The selected patients were divided into those with a nephrostomy catheter and those without a nephrostomy catheter. The demographic parameters of the patients with a nephrostomy were compared with those without (age, gender, weight and site of stone), transoperative variables (surgery time and transoperative bleeding) and postoperative variables (need for intensive care, need for transfusion, surgical wound infection and hospital stay), using a Chi-square test with Yates correction for the non-parametric data.
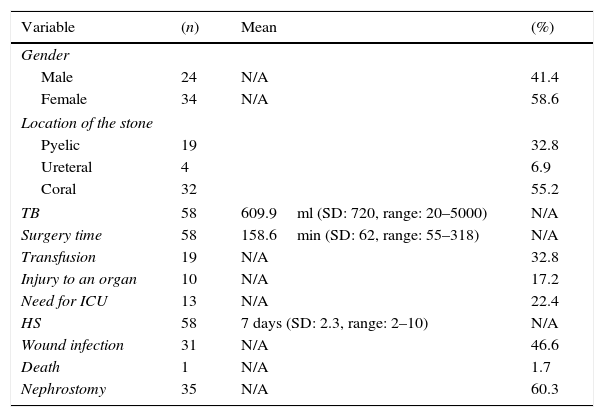
ResultsA total of 58 patients with a history of open simple nephrectomy were included. There were 24 males (41.4%) and 34 females (58.6%). The mean age was 46 years (SD: 14.1). The location of the stones was pyelic in 32%, ureteral in 6.9% and coral in 55.2%. Regarding the transoperative variables, the mean transoperative bleeding was 604.9ml (SD: 720, range: 20–5000ml) and the mean surgery time, from the skin incision to wound closure, was 158.6min (SD; 62, range: 55–318). The postoperative variables were as follows: 19 patients required a transfusion (32.8%) (Clavien-Dindo II), 10 patients had a vascular injury or injury to a solid organ during the operation (17.2%) (Clavien-Dindo IIIb), 13 patients were admitted to the intensive care unit (22.4%) (Clavien-Dindo IV), the mean hospital stay was 7 days (SD: 2.3, range: 2–10), 31 had a surgical wound infection (46.6%) (Clavien-Dindo II) and one patient died (1.7%) (Clavien-Dindo V) (Table 1).
Descriptive statistics for 58 patients following a simple nephrectomy using the retroperitoneal approach secondary to lithiasis.
| Variable | (n) | Mean | (%) |
|---|---|---|---|
| Gender | |||
| Male | 24 | N/A | 41.4 |
| Female | 34 | N/A | 58.6 |
| Location of the stone | |||
| Pyelic | 19 | 32.8 | |
| Ureteral | 4 | 6.9 | |
| Coral | 32 | 55.2 | |
| TB | 58 | 609.9ml (SD: 720, range: 20–5000) | N/A |
| Surgery time | 58 | 158.6min (SD: 62, range: 55–318) | N/A |
| Transfusion | 19 | N/A | 32.8 |
| Injury to an organ | 10 | N/A | 17.2 |
| Need for ICU | 13 | N/A | 22.4 |
| HS | 58 | 7 days (SD: 2.3, range: 2–10) | N/A |
| Wound infection | 31 | N/A | 46.6 |
| Death | 1 | N/A | 1.7 |
| Nephrostomy | 35 | N/A | 60.3 |
HS: hospital stay; TB: transoperative bleeding; ICU: intensive care unit.
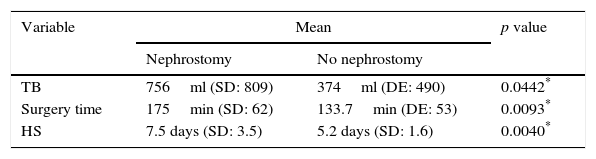
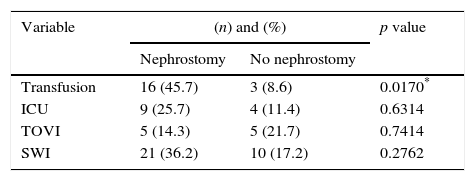
The patients were divided into 2 groups, those with a nephrostomy catheter (group 1) and those without a nephrostomy catheter (group 2). Of the cases reported, 35 patients had a nephrostomy catheter (60.3%) and 23 did not (39.7%); one patient in group 1 died (Clavien-Dindo V) in the immediate postoperative period. On comparing the two groups, there was a mean transoperative bleeding in group 1 of 756ml (SD: 809, range: 100–5000), and in group 2 of 374ml (SD: 490, range: 20–1700). Surgery time in group 1 was a mean of 175min (SD: 62, range: 75–318) and in group 2133.7min (SD: 53, range: 55–230). The mean hospital stay in group 1 was 7.5 days (SD: 3.5, range: 2–15) and for group 2 it was 5.2 days (SD: 1.6, range: 4–10). Sixteen patients in group 1 required a transfusion (45.7%) and 3 patients in group 2 (8.6%). Nine patients in group 1 required intensive care in the intensive care unit (25.7%) and 4 patients in group 2 (11.4%). Five patients in group 1 had a vascular injury or injury to an organ (14.3%) as did 5 patients in group 2 (21.7%). Twenty-one patients had a surgical wound infection in group 1 (36.2%) and 10 patients (17.2%) in group 2 (Tables 2 and 3).
Comparison of the parametric variables in the 2 groups.
| Variable | Mean | p value | |
|---|---|---|---|
| Nephrostomy | No nephrostomy | ||
| TB | 756ml (SD: 809) | 374ml (DE: 490) | 0.0442* |
| Surgery time | 175min (SD: 62) | 133.7min (DE: 53) | 0.0093* |
| HS | 7.5 days (SD: 3.5) | 5.2 days (SD: 1.6) | 0.0040* |
HS: hospital stay (days); TB: transoperative bleeding; surgery time: from skin incision to wound closure.
Comparison of nonparametric variables in the 2 groups.
| Variable | (n) and (%) | p value | |
|---|---|---|---|
| Nephrostomy | No nephrostomy | ||
| Transfusion | 16 (45.7) | 3 (8.6) | 0.0170* |
| ICU | 9 (25.7) | 4 (11.4) | 0.6314 |
| TOVI | 5 (14.3) | 5 (21.7) | 0.7414 |
| SWI | 21 (36.2) | 10 (17.2) | 0.2762 |
SWI: surgical wound infection; TOVI: transoperative organ or vascular injury; ICU: need for care in intensive care unit.
On comparing the 2 groups statistically significant differences were found for the variables of transoperative bleeding (p=0.0442), surgery time (p=0.0093), length of hospital stay (p=0.0040) and need for transfusion (p=0.0170). There were no differences in the need for intensive care (p=0.6314), transoperative complications (p=0.7414) and surgical wound infection (p=0.2762).
DiscussionMost of the patients who underwent a nephrectomy had a nephrostomy catheter (60.3%), which was placed secondary to obstruction of the urinary tract with or without pyonephrosis. The mortality reported in our series was one patient, which is low compared to series of open nephrectomies due to renal exclusion reported in the literature.5 This might be due to better quality of perioperative care and expert surgical technique.
The patients with a nephrostomy catheter on average had greater bleeding (756ml vs 756ml) and longer surgical time (175min vs 133.7min), which was statistically significant (p=0.0442 and p=0.0093), and at the same time presented a greater need for transfusion, with a statistically significant difference (45.7% vs 8.6%, p=0.0170). This might reflect greater technical difficulty and greater loss of anatomical structures, with the presence of more fibrosis, secondary to the inflammation and chronic infection presented by patients with a nephrostomy. There are no studies that have examined this association previously.
The hospital stay was significantly longer in patients with a nephrostomy catheter (7.5 days vs 5.2 days p=0.0040), the longer hospital stay was a result of persistently elevated leucocyte levels and pain at the surgical site in most cases.
No differences were found on comparing the 2 groups in terms of need for intensive care (25.7% vs 11.4%), surgical wound infection (36.2% and 17.2%) and transoperative injury to an organ (14.3% vs 21.7%), even so these were highly prevalent in our population in both groups, which demonstrates the great technical difficulty of simple nephrectomy in lithiasic disease.
A team studied the association between surgical wound infection in nephrectomy patients with and without nephrectomy.15 They reported a series of 31 patients, and found that 77.7% of the patients with nephrostomy presented a surgical wound infection, whereas only 31.8% in the group without a nephrostomy catheter did so. This was a statistically significant difference. They concluded that the patients with a nephrostomy that was placed due to pyonephrosis or to alleviate an obstruction, who underwent a simple nephrectomy due to irreversible kidney damage, had earlier and more frequent wound infections than patients who underwent the same procedure without a nephrostomy.
There are very few studies in the literature that compare the results of open simple nephrectomies in patients with and without nephrostomy. This is very probably because the open nephrostomy technique is no longer used in industrialized countries and has been replaced by the new laparoscopic and robotic procedures. However, in our population this technique still plays a fundamental role in the treatment of our patients, and our work found valuable information for the urologists who continue to perform the procedure.
ConclusionsAn open simple nephrectomy using a retroperitoneal approach secondary to lithiasis in patients with a nephrostomy poses a challenge to surgeons, since it increases the technical difficulty due to greater transoperative bleeding and longer surgery time, with a higher incidence of transfusions, resulting in a longer hospital stay compared to patients without a nephrostomy catheter. All these factors increase costs and morbidity and mortality.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that the procedures followed were in accordance with the regulations of the relevant clinical research ethics committee and with those of the Code of Ethics of the World Medical Association (Declaration of Helsinki).
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Carrillo-Córdova LD, Jiménez-Villavicencio JM, Vitar-Sandoval J, Sarabia-Estrada RC, Rivera-Astorga H, Lemus-Mena GR, et al. Comparación de los resultados de la nefrectomía simple abierta secundaria a litiasis en pacientes con y sin nefrostomía. Cir Cir. 2017;85:325–329.