Pseudomembranous colitis, caused by Clostridium difficile, has seen an increased incidence in recent years, driven mainly by the indiscriminate use of antibiotics. Although initial treatment is medical, the role of emergency surgery has gained ground due to high mortality and the emergence of increasingly virulent strains. In our country the prevalence is still low so that sometimes our experience in handling is limited.
AimTo analyze our surgical experience in treatment of this disease and to remember the role of surgery as well as some technical aspects of it.
Clinical casesWe present 2 cases of patients who have suffered a fulminant pseudomembranous colitis unresponsive to initial medical treatment and requiring urgent surgical intervention with a good response to it.
ConclusionsIt is important to keep in mind the surgical option in treatment of pseudomembranous colitis, especially when it presents as fulminant colitis, there are associated complications or failure to respond to medical treatment.
La colitis pseudomembranosa, producida por el Clostridium difficile, presenta una incidencia creciente en los últimos años, motivada principalmente por el uso indiscriminado de antibióticos. Aunque su tratamiento de inicio es médico, el papel de la cirugía de urgencias ha ido ganando terreno debido a una mortalidad elevada y a la aparición de cepas cada vez más virulentas. En nuestro medio su prevalencia aún es escasa, por lo que en ocasiones nuestra experiencia en su manejo es limitada.
ObjetivoAnalizar nuestra experiencia quirúrgica en el tratamiento de esta dolencia y recordar el rol de la cirugía, así como alguno de sus aspectos técnicos.
Casos clínicosPresentamos 2 casos clínicos de pacientes que han presentado un cuadro de colitis pseudomembranosa de presentación fulminante, sin respuesta al tratamiento médico inicial, por lo que se requiere una actuación quirúrgica urgente, con buena respuesta.
ConclusionesEs importante siempre tener en mente la posibilidad quirúrgica en el tratamiento de la colitis pseudomembranosa, sobre todo cuando se presenta de manera fulminante, existen complicaciones asociadas o falla de respuesta al tratamiento médico.
Clostridium difficile is a Gram-positive bacteria microorganism that forms part of normal intestinal flora in a few healthy individuals and hospitalised patients.1 It was first described as a microbiota in neonates, but it was not until 1978 that it was identified as a cause of pseudomembranous colitis associated with the use of antibiotics.2,3
The spectrum of diseases caused by C. difficile ranges from uncomplicated diarrhoea to serious conditions such as fulminant pseudomembranous colitis or toxic megacolon. Although the initial treatment of choice is non-surgical, if this proves ineffective, surgery should be considered.4
The epidemiology of this disease has changed considerably in recent decades. It is even suggested that it will become a global pandemic due to the indiscriminate use of antibiotics, as prophylactic treatment in the form of broad-spectrum antibiotics, and with the appearance of hypervirulent strains (ribotype 027).5
Its prevalence in Spain in the period 1999–2007 increased from 39 to 122 cases, with an annual increase of 9%. This was put down to indiscriminate use of antibiotics, the ageing population and increased inpatient comorbidity. Even so, the incidence in our country is lower than other countries such as the United States, Canada or the United Kingdom and, as yet, no cases caused by hypervirulent strains have been described.6–8
Since the discovery of this hypervirulent strain, a trend towards more severe forms of colitis has been observed with poorer outcomes. This has placed the emphasis on establishing appropriate treatment regimens, especially for refractory infections. In mild to moderate cases, oral metronidazole is considered an appropriate first line of treatment but, in the absence of an appropriate clinical response, a switch to vancomycin is required. Thus, oral vancomycin should be used as the initial therapy in severe cases or in patients who are intolerant to metronidazole. The rectal route should be reserved for supplementary therapy in severe cases. Patients who cannot tolerate oral administration should be given intravenous metronidazole or rectal vancomycin. Surgical consultation should be prompt for patients presenting colitis that is refractory to treatment or fulminant colitis, since they can require urgent surgical intervention in up to 1–3% of cases.9,10
Clinical casesCase 1A 37-year-old women with a history of acute lymphoblastic leukaemia under chemotherapy treatment. The patient started with symptoms of abdominal pain accompanied by vomiting, diarrhoea and fever which did not remit despite having been treated previously with amoxicillin/clavulanic acid, azithromycin and amphotericin. After testing positive for C. difficile toxin in her faeces, treatment was commenced with parenteral metronidazole. After an improvement in symptoms, the patient was discharged from hospital under treatment with oral vancomycin.
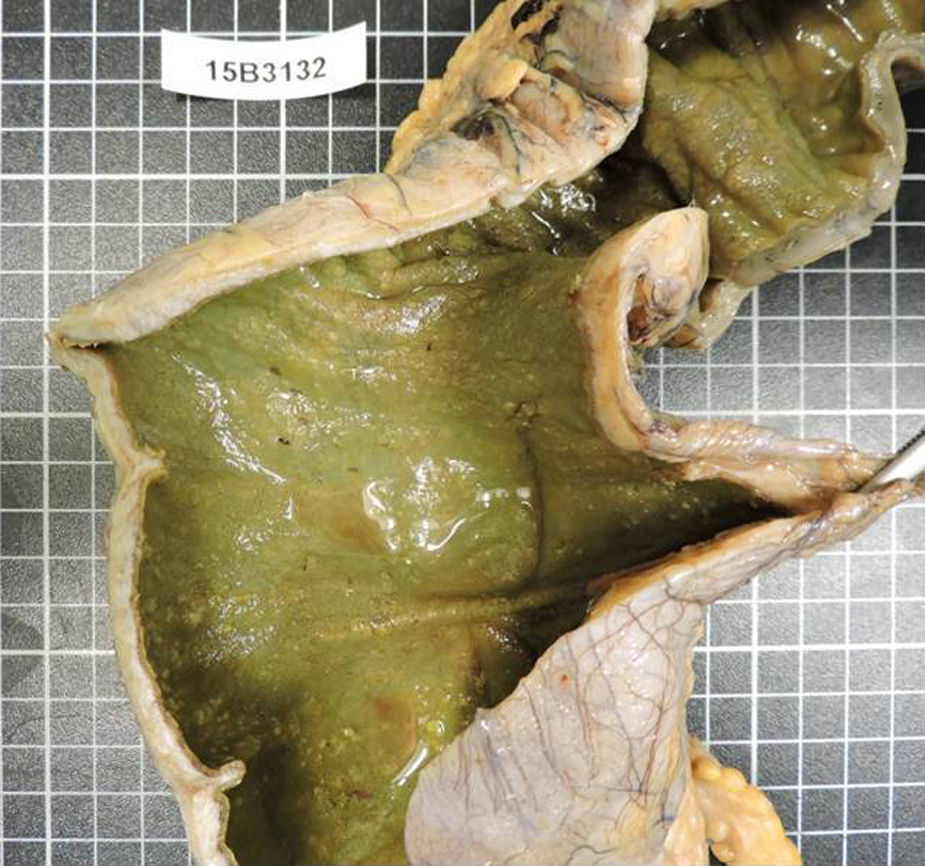
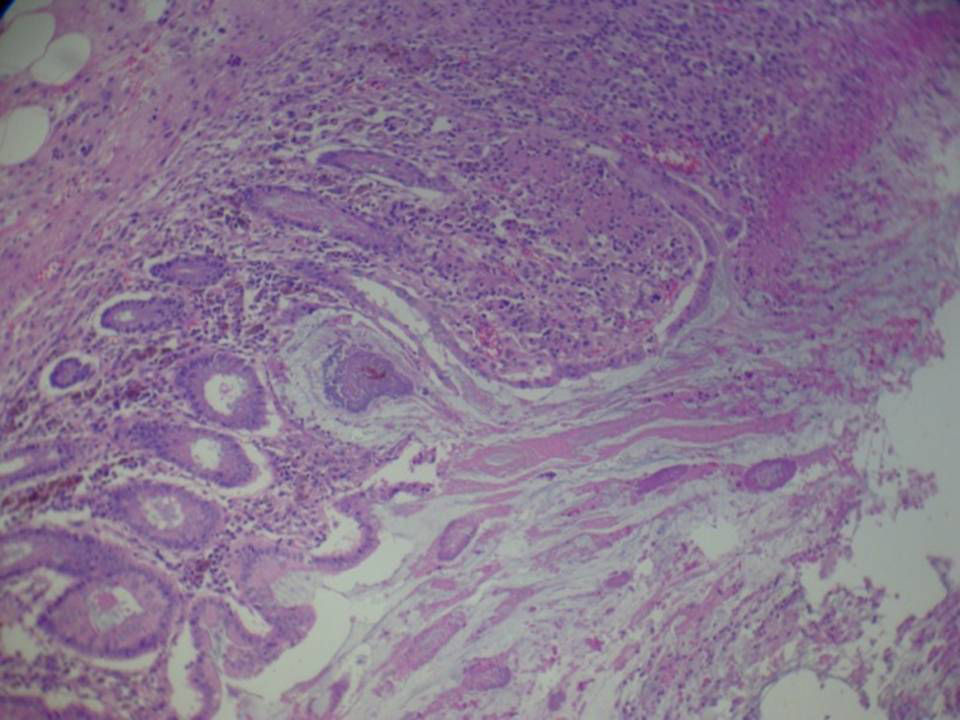
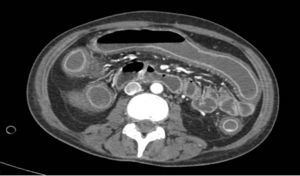
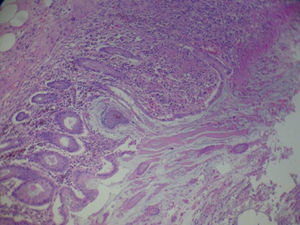
The patient returned a few days later with septic symptoms which required her to be admitted to the Intensive Care Unit, and treated with vaso-active drugs and orotracheal intubation. Due to the patient's failure to respond to treatment in the first 24h, emergency surgery was decided. A subtotal colectomy and terminal ileostomy was performed. After surgery the patient improved significantly with progressive reduction of amines until they were withdrawn, orotracheal extubation, with negativisation of toxin in faeces (Figs. 1 and 2).
A 72-year-old woman admitted to the Neurology Department due to a subarachnoid haemorrhage. She had a history of treatment with amoxicillin/clavulanic acid prior to admission.
Her symptoms became worse with abdominal pain, diarrhoea and bradypsychia. Ischaemic colitis was suspected after abdominal tomography; however colonoscopy suggested a first possible diagnosis of pseudomembranous colitis. Despite medical treatment the patient did not improve and developed septic shock and multiple organ failure. Emergency surgical intervention was decided and subtotal colectomy and terminal ileostomy performed. After surgery the patient presented clear improvement and was discharged a few days later (Fig. 3).
DiscussionFulminant colitis presents in 3–10% of cases. It involves concomitant systemic toxicity, organ malfunction with the need for vasoactive drugs or ventilatory support. Up to 20% of cases can require surgery; nevertheless there is a 35% and 80% mortality rate.11
Historically, surgery was seldom used due to the poor outcomes traditionally demonstrated. This was because the published series were small and there was no standard definition of fulminant colitis.12
It has currently been established that surgery can save lives in some cases, and that most patients require total or subtotal colectomy with terminal ileostomy. In terms of surgical technique, resection should include removal of the sigmoid colon, preserving the rectum and the pelvic tissues to enable the hypothetical posterior reconstruction of the intestinal tract.13
By contrast, some authors currently suggest minimally invasive surgery, whereby the colon is preserved, as a surgical alternative. Thus a reduction in the morbidity and mortality associated with the surgical procedure is achieved. This technique is based principally on creating an ileostomy using the laparoscopic approach, colonic irrigation and topical administration of vancomycin. The authors put this efficacy down to less aggression being caused to the critical patient and the removal of any faecal bolus, which will prevent the influx of nutrients to the intestinal flora.14 Although this technique had already been described in 1971 by Turnbull et al.,15 in cases of toxic megacolon secondary to inflammatory bowel disease as a bridging procedure to achieve improved clinical symptoms before definitive elective surgery, it was seldom performed in the past.
Surgery is indicated in the case of any of the following factors: perforation or necrosis of the colon wall, the need for vasoactive drugs, signs of sepsis, changes in mental state, leukocytosis above 50,000, lactic acid greater than 5mmol/l, or if there has been no clinical improvement after 5 days of treatment.16
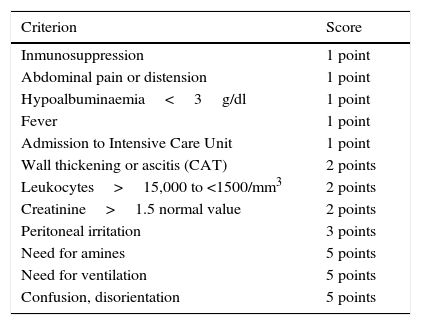
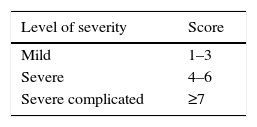
Similarly, Neal et al.17 described a specific points system for this disorder, classifying it in terms of severity according to the total factors presented by the patient: mild is from 1 to 3 points, severe from 4 to 6 points, severe, complicated ≥7 (Tables 1 and 2). However, no specific indications have been established with regard to surgery, since the score necessary to indicate it has not yet been established.
Risk factor score for pseudomembranous colitis.
| Criterion | Score |
|---|---|
| Inmunosuppression | 1 point |
| Abdominal pain or distension | 1 point |
| Hypoalbuminaemia<3g/dl | 1 point |
| Fever | 1 point |
| Admission to Intensive Care Unit | 1 point |
| Wall thickening or ascitis (CAT) | 2 points |
| Leukocytes>15,000 to <1500/mm3 | 2 points |
| Creatinine>1.5 normal value | 2 points |
| Peritoneal irritation | 3 points |
| Need for amines | 5 points |
| Need for ventilation | 5 points |
| Confusion, disorientation | 5 points |
Pseudomembranous colitis score proposed by Neal et al.17
The treatment of choice for pseudomembranous colitis is medical, reserving surgery for specific cases. Surgery is being performed increasingly promptly for this disorder and therefore is less aggressive, which has achieved better outcomes. Therefore we consider it is important to bear in mind the possibility of surgery to treat the disorder, especially when the condition is fulminant, when there are associated complications or when there is failure to respond to medical treatment.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that the procedures followed were in accordance with the regulations of the relevant clinical research ethics committee and with those of the Code of Ethics of the World Medical Association (Declaration of Helsinki).
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Tallón-Aguilar L, de la Herranz-Guerrero P, López-Ruiz JA, Sánchez-Moreno L, López-Pérez J, Padillo-Ruiz FJ. Papel de la cirugía en el tratamiento de la colitis pseudomembranosa. Cir Cir. 2017;85:330–333.