Peripheral arterial disease and coronary artery disease are frequently associated. The percutaneous approach may sometimes involve additional difficulties to the coronary artery disease.
Clinical caseThe case is presented on an 82-year-old male patient with multiple cardiovascular risk factors, a Leriche syndrome and axillobifemoral bypass, who was admitted to hospital due to an inferior myocardial infarction. The procedure approach (radial, brachial, or femoral access routes for percutaneous coronary treatment) and associated complications from the procedure are discussed.
ConclusionAlthough technical improvements and/or treatment of peripheral vascular lesions may allow percutaneous coronary intervention, individual risk and benefit in each patient must be assessed.
La arteriopatía periférica y la enfermedad coronaria están frecuentemente asociadas, y plantear el abordaje percutáneo puede entrañar, en ocasiones, dificultades añadidas a la propia enfermedad coronaria.
Caso clínicoPresentamos el caso de un paciente varón de 82 años, con múltiples factores de riesgo cardiovasculares, síndrome de Leriche y bypass axilobifemoral, que ingresa por infarto de miocardio inferior. Se comentan las dificultades en las vías de acceso (radial, braquial y femoral) y las posibles complicaciones derivadas del tratamiento coronario percutáneo.
ConclusiónAunque las mejoras técnicas en el tratamiento de las lesiones vasculares periféricas, pueden permitir el tratamiento percutáneo de las lesiones coronarias, debemos valorar el riesgo y el beneficio en estos pacientes de forma individualizada.
Atherosclerosis is a systemic disease, which jointly involves several vascular territories, including peripheral artery disease, which is one of the most prevalent conditions and usually coexists with coronary heart disease.1 This potentially increases morbidity, and therefore, mortalitiy.2 It is estimated that 32% of patients with peripheral artery disease also have associated coronary or cerebrovascular disease, and 24% of them have disease in the 3 territories,3 which reflects the severity and extension of the atherosclerotic process. In fact, patients with acute coronary syndrome and peripheral artery disease have more extensive and severe heart disease and therefore a poorer inpatient and outpatient clinical outcome.4,5
Patients with peripheral vascular arteriopathy and heart disease have a poor prognosis, and treatment alternatives for them are considerably reduced; hence the importance of making an appropriate functional diagnosis, to enable the specialist to decide the invasive coronary procedures required, irrespective of the difficulties of access via the percutaneous approach.
This article describes the therapeutic management of a patient with acute coronary syndrome and peripheral vascular arteriopathy.
Clinical caseAn 82-year-old male with a history of diabetes mellitus, systemic arterial hypertension, smoker, former drinker of alcohol at toxic levels, chronic obstructive pulmonary disease and chronic kidney failure. The patient had undergone an axillobifemoral bypass due to Leriche's syndrome 7 years previously, a right hemicolectomy for ischaemic colitis 5 years previously, endoscopic argon plasma coagulation for a lower digestive tract haemorrhage, secondary to duodenal angiodysplasia 4 years previously, and 2 years previously had started treatment with: clopidogrel (75mg/24h orally), ranitidine (150mg/12h orally) for a lacunar ischaemic stroke in the territory of the right middle cerebral artery probably of atheroembolic origin.
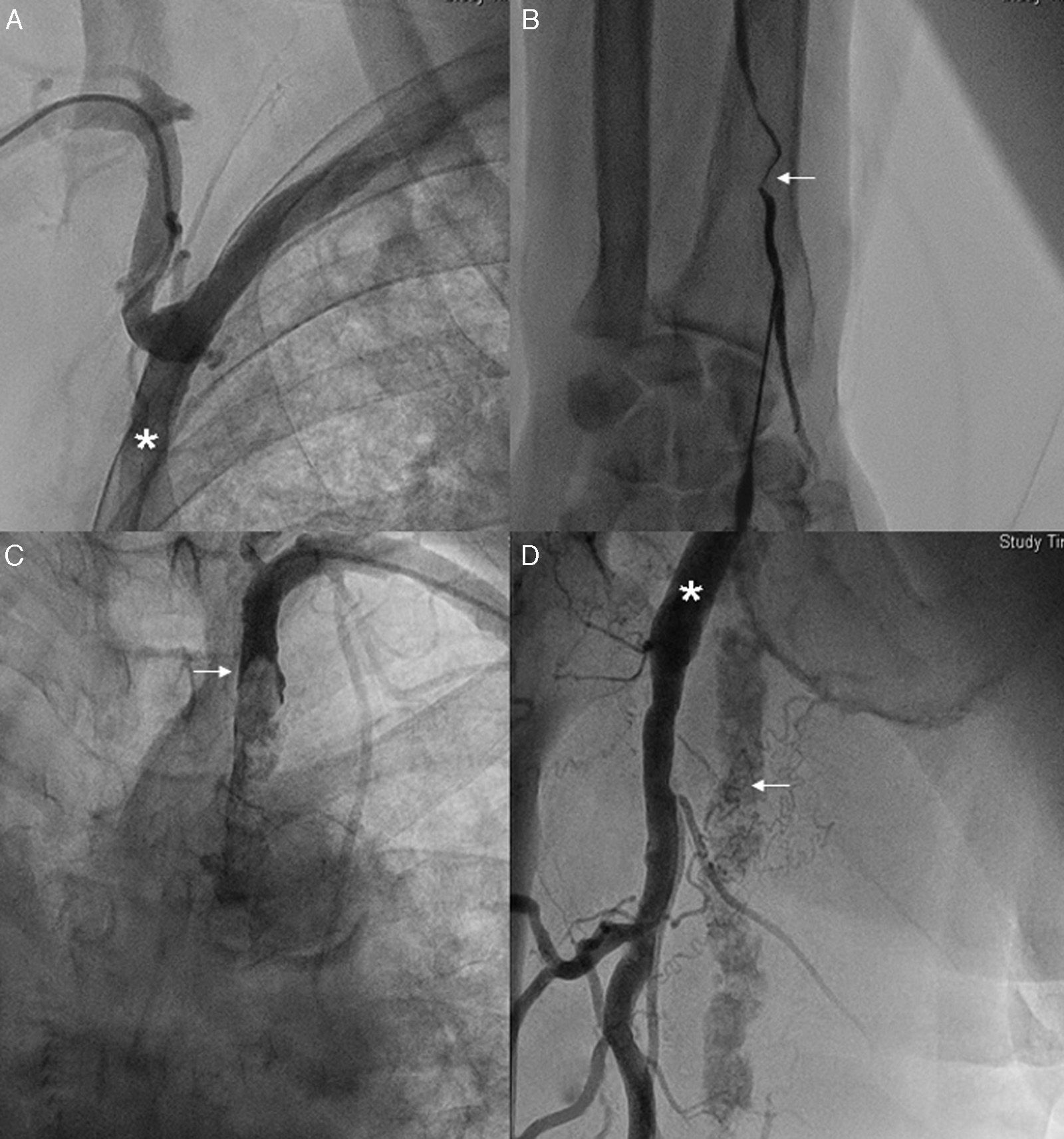
Days before he was admitted to hospital he presented symptoms compatible with melena. On admission he reported epigastralgia and vegetative reactions, over 10h, electrocardiogram revealed ST elevation of 2mm on the bottom side, and therefore he was given a loading dose of acetylsalicylic acid (300mg) and clopidogrel (300mg) orally, an intravenous bolus of heparin sodium (5000IU) and intravenous nitroglycerin in continuous perfusion. However, due to the recent picture of digestive tract bleeding, fibrinolysis was decided against, and a primary angioplasty was performed. Initially the approach was through the right radial artery but it was not possible to reach the ascending aorta, due to the high angulation of the right subclavian artery after the axillobifemoral bypass outlet (Fig. 1A). Due to the impossibility of right-sided access, entry through the left radial artery was attempted unsuccessfully, due to stenosis at this level (Fig. 1B). For this reason the left brachial artery was cannulated, without managing to reach the aorta due to a sub-occlusion at proximal level of the left subclavian artery (Fig. 1C). Finally, an attempt was made to cannulate the femoral arteries, beneath the axillobifemoral bypass connection, and avoid puncturing them. It was not possible to cannulate the femoral artery (Fig. 1D).
(A) Evidence of high angulation of the right subclavian artery after the axillobifemoral bypass outlet (asterix). (B) Stenosis of the left radial artery (arrow). (C) Sub-occlusion at the level of the proximal third of the left subclavian artery (arrow). (D) High angulation at the level of the superficial femoral artery (arrow) with axillofemoral bypass (arrow) connected to the deep femoral artery.
Due to the course of the infarction, the patient's stability, poor electrocardiographic expression and the risk of puncturing the bypass in an anticoagulated patient, with double antiaggregation on admission, it was decided to opt for conservative treatment. However, 12h later, the patient presented a complete atrioventricular block, with haemodynamic repercussions. For this reason, an attempt was made to place a temporary transvenous pacemaker, using Seldinger's technique, without managing to advance the guide. A few minutes later, the patient entered asystole. Despite advanced cardiopulmonary resuscitation manoeuvres, the patient died.
DiscussionPatients with extracardiac vascular disease are doubly at risk of presenting more extensive and severe heart disease, which increases their chances of fatal reinfarction.2 This reflects the severity and extension of the atherosclerotic process, and added to this is the fact that effective therapeutic interventions, such as the use of glycoprotein IIb/IIIa inhibitors, beta blockers or early coronarography are used less frequently.6
With reference to percutaneous vascular access in patients with peripheral artery disease, we should bear in mind the difficulty and complexity that these procedures occasionally entail.6 In fact, the co-existence of peripheral artery disease can force a change of initial access route or oblige acting percutaneously on the vascular lesion which is impeding access,7 as occurred in the case we present; despite the fact that the use of hydrophilic guidewires or long sheath introducers has greatly improved percutaneous access in these patients.
With regard to puncturing the axillofemoral bypass, previous studies document that direct puncture of a vascular graft8 is safe and preferable to the transaxillary route.9,10 However, we should bear possible complications in mind, which include: uncontrollable bleeding due to the nonvascular nature of the graft, interruption of the anastomotic suture with the consequent formation of a pseudo aneurysm, infection of the graft or interruption of pseudointima with the consequent tendency towards thrombosis.
ConclusionNonetheless, with the diversity of catheters and hydrophilic material available for treating peripheral vascular lesions, which can potentially enable vascular access, we should make a cost–benefit evaluation in these patients and individually assess possible complications in each case.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
FundingNone of the authors have received funding.
Authors’ contributionAll the authors have participated in interpreting the data, drafting the article and the final approval of the version for publication.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Martínez-Quintana E, Rodríguez-González F. Dificultades en el abordaje percutáneo del síndrome coronario agudo con bypass axilobifemoral. Cir Cir. 2016;84:405–408.