Painful shoulder impingement syndrome is one of the first reasons for care in rehabilitation centres. As the evidence regarding the effectiveness of physical measures as adjuvant treatment is limited, the aim of this study was to determine the effectiveness of physiotherapy on shoulder pain.
Material and methodsA retrospective and analytical study was conducted using the medical records of patients with shoulder pain who attended in a rehabilitation centre from October 2010 to September 2011. The demographic and clinical data were collected, and the clinical improvement was determined as: complete, incomplete, or no improvement. Statistical analysis: Chi squared was used to determine whether there were differences between the different modalities of physiotherapy, as well as the level of improvement.
ResultsThe study included a total of 181 patients, with a mean age of 54.3 years, and a mean of 4.6 months of onset of pain. The physiotherapy treatments included: warm compresses plus interferential current (60.2%), and warm compresses plus ultrasound (17.1%). Just over half (53.6%) obtained a moderate recovery, 36.4% slight improvement, and 9.9% no improvement. No significant differences were found between the different forms of therapy.
ConclusionsThe supervised rehabilitation programme consists of 9 sessions of physiotherapy. A functional improvement of 90% was obtained, without finding any statistical differences between the therapies used.
El síndrome de abducción dolorosa de hombro es de las primeras causas de atención en las unidades de rehabilitación; sin embargo, la evidencia en la efectividad de los medios físicos como coadyuvante del tratamiento es limitada.
El objetivo de este estudio fue identificar la efectividad de los medios físicos como coadyuvante del tratamiento en el síndrome de abducción dolorosa de hombro.
Material y métodosSe realizó un estudio retrospectivo y analítico en el que se revisaron los expedientes clínicos de los pacientes con el diagnóstico de síndrome de abducción dolorosa de hombro, en un centro de rehabilitación desde octubre de 2010 a septiembre de 2011. Se recabaron: datos clínicos y demográficos; se determinó la mejoría clínica como: mejoría moderada, mejoría leve o sin mejoría. Análisis estadístico: para buscar diferencias entre las modalidades de terapia física y mejoría se utilizó la prueba de χ2.
ResultadosSe incluyeron 181 pacientes con una edad media de 54.3 años; el tiempo de evolución fue de 4.6 meses en promedio. Las modalidades de terapia física más utilizadas fueron: compresas húmedo-calientes más corrientes interferenciales (60.2%) y compresas húmedo-calientes más ultrasonido (17.1%). El 53.6% obtuvo una mejoría moderada, el 36.4% una mejoría leve, y el 9.9% no tuvo mejoría. No se encontró diferencia estadística significativa entre las diferentes modalidades de terapia física.
ConclusionesEl programa de rehabilitación supervisada consistió en 9 sesiones de fisioterapia; se obtuvo una mejoría funcional del 90%, sin encontrar diferencia estadística entre los diferentes medios físicos empleados.
Painful shoulder impingement syndrome is a set of signs and symptoms associated with a disorder of the soft tissues of the shoulder. The symptoms can be divided into different diagnostic categories: subacromial impingement, tendinopathies, bursitis, adhesive capsulitis, calcium deposits and myofascial lesions.1–3
The prevalence of painful shoulder impingement syndrome in the adult population varies from 31% when subjects are questioned to 48% when they are shown a diagram with the area of the shoulder highlighted.4 In a sample of the general population in England a prevalence of 34%5 was found, and 30% was reported in Sweden.6
In Mexico it is a common problem, and in a study which included 466 women aged from 18 to 40, a prevalence of 29% was found.7 In rehabilitation centres this condition takes up almost 10% of outpatient consultations, principally affecting people of working age, and results in high costs for the healthcare institutions and society.8
Conservative management based on analgesics, non-steroidal anti-inflammatory drugs, local injections with steroids and rehabilitation is effective for most patients with painful shoulder impingement syndrome.9–11
The objective of physical rehabilitation is to restore the shoulder's functional range of movement and to reduce pain, in order to enable the patient to resume work and return to their daily routines.9 Rehabilitation involves therapeutic exercises (stretching, strengthening and progressive resistance training) joint movement, manipulation, education and the application of physical measures. However, evidence of the effectiveness of physical measures as adjuvant treatment in the rehabilitation of patients with painful shoulder is not documented.
The objective of this study is to identify the effectiveness of physical measures as adjuvant therapy for the functional recovery of patients with painful shoulder impingement syndrome.
Material and methodsA descriptive, retrospective and analytical study was undertaken, the clinical records of patients diagnosed with painful shoulder impingement syndrome, in the Physical Medicine and Rehabilitation Unit of the Instituto Mexicano del Seguro Social, between 1 October 2010 and 30 September 2011, after authorisation from the Local Research Committee.
Only patients aged over 18 who had been attended for the first time in the rehabilitation department and who needed to enter a supervised rehabilitation programme were included in the study. Incomplete clinical records, patients who had received surgical treatment, and patients still undergoing rehabilitation treatment were excluded from the study.
The information obtained from the clinical records was: age, sex, level of education, civil status, time from onset of the disorder, comorbidities, drug addition, history of surgery, date of admission to supervised rehabilitation, physical measures used, number of sessions, whether or not the patient was working, and, finally, the type of improvement. When the patient presented a reduction in their pain at the end of the treatment of more than 50% compared to their pain on admission, and with functional recovery of the shoulder's range of motion, this was considered moderate improvement. Slight improvement was when the pain at the end of treatment did not reduce by more than 50%, but the patient achieved functional ranges of movement of the shoulder. There was considered to be no improvement if the patient presented no reduction in pain greater than 50% and did not achieve functional ranges of movement of the shoulder. The functional range of movement of the shoulder was taken as abduction and flexion of more than 120°.12
Statistical analysisFor the quantitative variables (age, time from onset, and number of sessions) the mean was used as the central tendency measure and standard deviation was used as the measure of dispersion, by presenting normal distribution demonstrated using the Kolmogórov–Smirnov test. The qualitative variables (gender, civil status, level of education, worker, disabled, comorbidities, drug addiction, shoulder surgery, admitted for supervised rehabilitation, physiotherapy modality and improvement) were presented as absolute and relative frequencies in contingency tables. The χ2 test was used to compare the difference between the type of physical measure used and the degree of clinical improvement, considering a p value <0.05 as statistically significant.
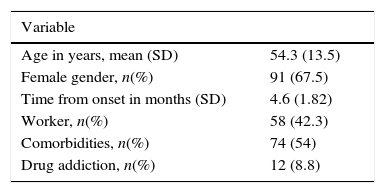
ResultsA total of 181 clinical records were obtained of patients with painful shoulder impingement syndrome who met the inclusion criteria. The mean age was 54.3, the female gender prevailed, and the time from onset was greater than 4.6 months (Table 1).
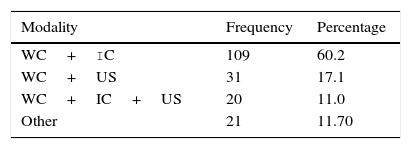
All the patients were told to do Codman's pendular exercises, stretching exercises and exercises to gradually strengthen the muscle groups of the shoulder according to the patients’ level of tolerance; the most frequently used physiotherapy was warm compresses plus interferential current (60.2%) (Table 2).
A moderate improvement was achieved in 53.6% (97 patients), slight improvement in 36.4% (66 patients), and no improvement with referral to orthopaedics for reassessment in 9.9% (18 patients).
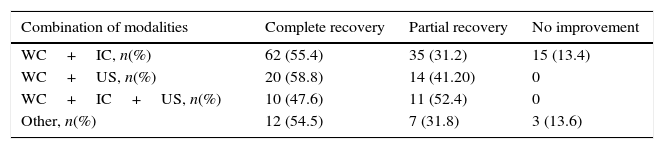
The comparison of the combination of the different physiotherapy modalities was made and the levels of recovery; no statistically significant differences were found (Table 3).
Physiotherapy modalities associated with functionality.
| Combination of modalities | Complete recovery | Partial recovery | No improvement |
|---|---|---|---|
| WC+IC, n(%) | 62 (55.4) | 35 (31.2) | 15 (13.4) |
| WC+US, n(%) | 20 (58.8) | 14 (41.20) | 0 |
| WC+IC+US, n(%) | 10 (47.6) | 11 (52.4) | 0 |
| Other, n(%) | 12 (54.5) | 7 (31.8) | 3 (13.6) |
WC: warm compress; IC: interferential current; US: therapeutic ultrasound.
Painful shoulder impingement syndrome is one of the main reasons for medical care in the general population and is one of the principal causes for consulting the rehabilitation services.3–7,9 In this study it was the third principal reason for outpatient rehabilitation consultations in 2011.
The characteristics of our sample included a mean age of 54.3, the disorder chiefly affected females (67.5%); these findings are similar to those reported in the literature.8 The mean time from onset was 4.6 months, which coincides with cases reported in other rehabilitation departments, where the patients with painful shoulder impingement syndrome generally consult more than 3 months after the onset.8 The Clinical Practice Guidelines Diagnosis and treatment of painful shoulder impingement syndrome at primary care level13 state that patients should start a supervised exercise programme or a programme at home to reduce their shoulder pain. However, in routine practice the exercise programme is not prescribed by general practitioners and patients are referred to rehabilitation when there is functional limitation of the shoulder. Similarly, the clinical practice guidelines recommend referral to rehabilitation only if discomfort persists after 2 or 3 weeks despite the general recommendations, analgesics and limited mobilisation of the shoulder.14
In a systematic review that assessed the physical measures used in patients with subacromial impingement syndrome, it was found that the use of ultrasound compared to a placebo did not show clinically significant differences.9 And in a systematic review which included 8 clinical trials with a total of 586 patients with calcifying tendinopathy, supraspinatus tendinopathy, tendinopathy of the biceps, shoulder pain, subacromial bursitis and adhesive capsulitis, only 2 of the studies demonstrated a benefit in patients with calcifying tendinopathy; 5 studies assessing pain found no significant differences, and of 4 studies which assessed ranges of mobility, only one reported a benefit.15
With regard to interferential current, there is evidence of its limited effectiveness in reducing pain and in improving the function of the shoulder, as demonstrated by Van der Heijden et al.16 in a clinical trial in which they compared the use of bipolar interferential currents to complement exercise compared to exercise alone; 12 treatment sessions were given over 6 weeks, without finding any statistically significant differences.
Laser treatment is another means used in patients with subacromial impingement. However, the evidence available to-date is mixed and most studies do not show a beneficial effect in patients with painful shoulder impingement syndrome.17–20
One of the essential components in the rehabilitation programmes for patients with painful shoulder impingement syndrome is therapeutic exercise, which at the moment is considered an effective intervention for this disorder.13,21–23 One of these exercise programmes is described in detail in the Clinical Practice Guidelines Diagnosis and treatment of painful shoulder impingement syndrome at primary care level,13 and in the literature there is also a self-managed therapeutic exercise programme.24 These programmes have been created in an attempt to avoid the patient having to wait until they can attend the rehabilitation department in order to start their treatment, which on average in our unit is over 3 months from onset of the disorder, therefore we recommend that general practitioners should receive training on the early indication for these exercises and thus improve the shoulder function of these patients.
Despite the limited evidence of the effectiveness of physical measures, the results of our rehabilitation programme showed clinical improvement in 90% of cases, and moderate clinical recovery was achieved in 56%. The available evidence shows that more than the physical measures used, exercise is the most important element in the functional recovery of patients with painful shoulder impingement syndrome, and Kooijman et al.,8 when they studied the effectiveness of physiotherapy in patients with painful shoulder impingement syndrome, found clinical improvement in 64% of their patients.25 For this reason, therapeutic exercise should be applied at primary care level for patients with painful shoulder impingement syndrome, enabling greater possibilities of improvement and fewer complications.
The limitations of the study included there being no specific evaluation scale to assess shoulder function such as, Disabilities of the Arm, Shoulder and Hand, American Shoulder and Elbow Surgeons or the Dutch Shoulder Disability Questionnaire, and the lack of knowledge about the extent to which home treatment is adhered to, and although the exercise programme has established stages (warm-up, stretching, progressive strengthening), it can vary according to the dedication and interest of each therapist. Another limitation is the lack of information on the dosage of the physiotherapy.
Due to all of the above, it is recommended that future clinical trials of high methodological quality are carried out in order to identify clinically effective, therapeutic rehabilitation interventions in order to establish specific treatment protocols as proposed in the self-managed exercise programme for patients with rotator cuff tendinopathy.24
ConclusionsThe supervised rehabilitation programme for the management of painful shoulder impingement syndrome comprises, on average, 9 sessions of physiotherapy, the most frequently-used method being warm compresses plus interferential current. In our study, functional improvement was achieved in 90% of cases, with no statistically significant difference found in effectiveness between the different physical measures used; therefore, we recommend that more emphasis should be placed on education and on the time spent on therapeutic exercise.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Gomora-García M, Rojano-Mejía D, Solis-Hernández JL, Escamilla-Chávez C. Efectividad de los medios físicos en el síndrome de abducción dolorosa de hombro. Cirugía y Cirujanos. 2016;84:203–207.