Most surgeons have rapidly accepted the use of minimally invasive surgical approaches for the treatment of primary hyperparathyroidism. The role of the endoscope in neck surgery is still being discussed due to its technical difficulty and complex patient selection criteria.
Materials and methodsA prospective study was conducted between April 2010 and April 2013. It included patients diagnosed with sporadic primary hyperparathyroidism by locating a single adenoma using ultrasound and sestamibi scintigraphy imaging. All patients agreed to be included in the study. Experienced endocrine surgeons that had been trained in endocrine minimally invasive surgery performed the procedure. The same surgical technique was used in all of the cases. The demographic and clinical variables were evaluated. A descriptive analysis was performed on the data measuring mean, standard deviation, and range.
ResultsA total of 28 endoscopic lateral parathyroidectomies were performed. All patients were diagnosed with sporadic primary hyperparathyroidism. The mean age was 68 years (59–89). No intraoperative complications were registered. Postoperative morbidity was comparable to that reported in the classical approach. A favourable outcome was observed in 27 of the 28 patients (96%) after a mean follow-up time of 22 (9–53) months.
ConclusionsAn endoscopic approach for sporadic primary hyperparathyroidism is feasible and reproducible, and it obtains comparable results to the classical open surgery. Several factors make this technique suitable for highly specialised hospitals with a high patient volume and specialised endocrine surgery units.
La mayoría de los cirujanos han aceptado de una manera rápida, la realización de miniprocedimientos abiertos para el tratamiento del hiperparatiroidismo primario. Sin embargo, la utilización de la endoscopia cervical sigue siendo discutible por su dificultad técnica y la estricta selección de los pacientes.
Material y métodosEntre los meses de abril del 2010 y del 2013, se incluyó a pacientes con hiperparatiroidismo primario esporádico, que además tenían un adenoma único tanto por ecografía y exploración con sestamibi, y que aceptaron participar en el estudio. Los pacientes fueron operados por cirujanos especialmente entrenados en este tipo de cirugía, utilizando la misma técnica quirúrgica en todos ellos. Se recogieron variables demográficas y características clínicas de los pacientes. Una vez finalizada la recolección de información se procedió al análisis descriptivo de las variables: mediana, desviación estándar y, rango.
ResultadosRealizamos un total de 28 paratiroidectomías mediante el abordaje de paratiroidectomía lateral endoscópica. La edad media de los pacientes fue de 68 años (59-89). Todos los pacientes tuvieron un hiperparatiroidismo primario esporádico. No se detectaron complicaciones intraoperatorias. La morbilidad fue comparable con la que muestran series publicadas en técnica abierta. Tras una mediana de seguimiento de 22 (9-53) meses, hemos detectado que el éxito de la intervención ha sido de 27/28 (96%).
ConclusionesEl abordaje endoscópico del primario esporádico resulta factible, reproducible y ofrece unos resultados comparables al abordaje clásico abierto, diversos factores hacen poco recomendable su realización fuera de hospitales con alto volumen de pacientes y unidades diferenciadas de Cirugía Endocrina.
When Félix Mandel published the first case of conventional parathyroidectomy in 1925,1 this procedure was rapidly accepted by the surgical community for its excellent clinical results and because the steps to perform it correctly were clearly established from the start.
Until the present day, it has been considered that the intervention proposed by Mandel results in surgical success in more than 95% of patients operated for primary hyperparathyroidism, when the 4 glands are explored via a transverse cervicotomy.2 Five percent of therapeutic errors have been observed in patients with multigland disease, supernumerary glands, major ectopia or, exceptionally, a carcinoma. With conventional parathyroidectomy not only can we expect very low morbimortality and a hospital stay of under 48h, it also offers excellent aesthetic results in the majority of patients. However, in recent years new technologies have been implemented, along with new approaches to parathyroidectomy: the unilateral approach,3–5 radio-guided surgery,6,7 minimally invasive open techniques (mini-incisions with or without local anaesthesia),8–10 and minimally invasive endoscopic techniques, video-assisted or fully endoscopic.11–19 The common objectives of all these techniques have been: a smaller incision, compared to the traditional open approach (transverse cervical incision) and performing targeted surgery to one of the glands specifically, in order to reduce aggression to the patient, and ensure more rapid recovery, as usually the excision of a small benign tumour is sufficient, without the need for sutures or surgical flaps.
The development of these minimally invasive approaches has been associated with three things in the main: first, the availability of imaging techniques which would enable us to accurately locate the adenoma that needs to be excised; second, intraoperative determination of parathormone, which will confirm resection of the diseased gland (and thus avoid examination of the other glands), and finally, the application of technological advances, which have already been applied in other fields, such as mini-instruments, sealing devices and optics and small-diameter cameras, to perform this type of surgery. And furthermore, patients increasingly want a less visible scar on their necks for aesthetic reasons.
Despite the fact that our group were pioneers in the development of this type of approach, since 1999 this endoscopic parathyroidectomy technique was used occasionally in our centre, and in 2010 we again included this technique in the routine therapeutic arsenal as an option that we offer to some of our patients with a diagnosis of primary hyperparathyroidism.
Materials and methodsA prospective, descriptive study was carried out with patients aged over 18 who were attended in the General and Endocrine Surgery Unit of the Hospital Clínic in Barcelona, with a diagnosis of primary hyperparathyroidism.
All the patients were included consecutively during the period between 1 April 2010 and 30 December 2013.
The diagnosis of primary sporadic hyperparathyroidism was based on the clinical history and physical examination of the patient, which was complemented with laboratory tests (blood samples chest and abdomen X-rays; and a cervical ultrasound with preoperative MIBI gammagraphy), to confirm the solitary nature of the lesion.
The criteria for exclusion from the study were: medical-anaesthetic (ASA) or surgical contraindications in order to perform endoscopic surgery, the presence of a large goitre, or previous thyroid or parathyroid surgery, “impossibility of locating the adenoma with imaging tests” or the presence of an adenoma of a size greater than 3cm.
This study was approved by the Surgical Department of our institution and all the patients were informed of the possibility of other therapeutic options (conventional open surgery).
All the patients were operated by the same team of surgeons, specialists in endocrinological disorders.
The patients’ demographic variables were recorded (age and gender), and their clinical characteristics (date of admission, date of discharge, surgical time, intra-operative complications, post-operative pain [visual analogue scale 0–10], the time oral diet was started, hospital stay) and cure of the disease. Once the information had been gathered, a descriptive analysis of the variables was undertaken (median and range).
Surgical techniqueThe cervical endoscopy was performed under general anaesthesia and the patient was placed in the supine position with open arms (Fig. 1). The surgeon stood on the side of the diseased gland with their assistant to their right. Our technique consisted of using a 10mm trocar and some 3mm trocars in order to achieve good vision, and two useful work channels.
The 3 trocars were positioned on the line of the anterior edge of the sternocleidomastoid muscle (SCM) (Fig. 2). The procedure was completed in 3 steps: first step or open phase: a 15mm transverse incision was made over the anterior edge of the SCM, just caudal to the cricoid cartilage. The dissection was commenced on the plane between the anterior edge of the SCM and the posterior edge of the infrahyoid muscles, and just below the omohyoid muscle. Then the fascia that connects the posterior side of the thyroid lobe with the carotid vein, was carefully divided, enough to visualise the prevertebral fascia. In order to be able to expand the working area, one or 2 damp swabs were placed deeply above and below inside the initially created space.
The transparietal route of the 3mm trocars was through the incision, from the outside to the inside. The route of the trocars needs to follow the anterior edge of the SCM, so that they can be placed in their site inside the space created initially.
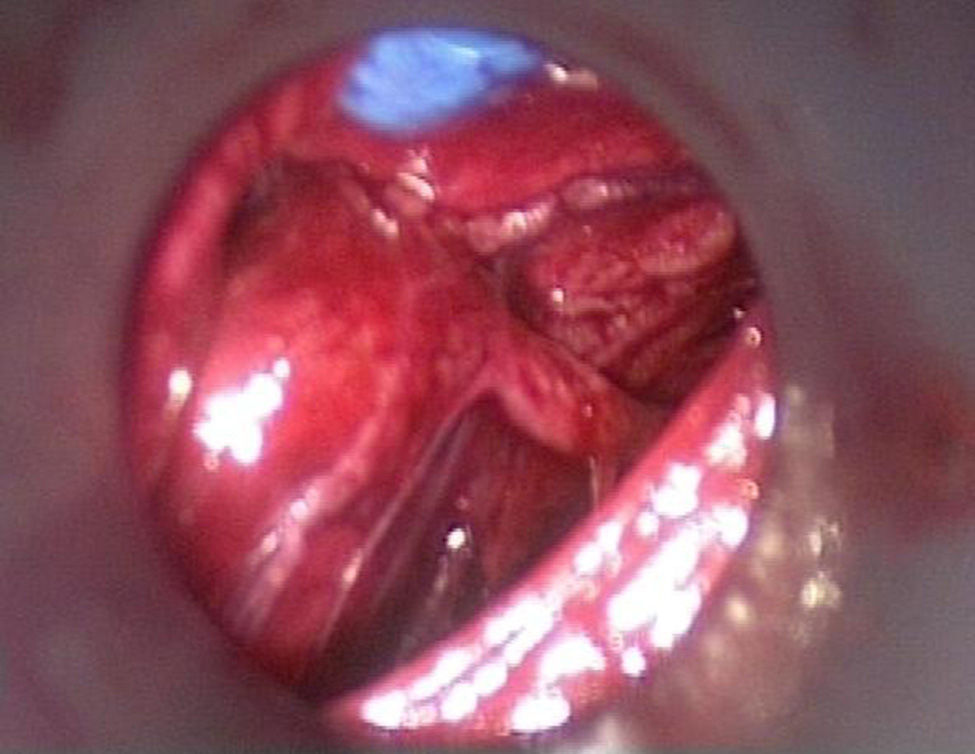
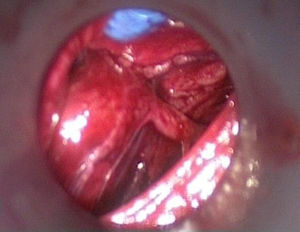
The second step of the operation is endoscopic exploration with CO2 pressure at 8mm of mercury. Immediately after introducing the camera, and making a minimal dissection, all anatomical structures should be easily identified (Fig. 3), and the recurrent laryngeal nerve should be found first; if possible the ipsilateral gland should be checked.
The adenoma is gradually dissected from the adjacent structures, and isolated, and when it is possible to isolate the pedicle it is not necessary to continue with the endoscopic dissection. After removing the 4 trocars, the third step of this procedure is performed openly, through the opening of the largest trocar when the adenoma can be seen, and its pedicle can be sealed without any difficulty.
The adenoma is directly extracted through the same incision as the trocar, and it is not necessary to place a sterile protection bag. This approach, initially proposed to all the patients, was principally used for adenomas located behind the thyroid lobe.
In our group a rapid intraoperative parathormone assay is not carried out, and instead, we perform anatomopathological analysis of the removed gland.
ResultsWe performed a total of 28 parathyroidectomies (20 women and 8 men), using the endoscopic technique. All the patients had sporadic primary hyperparathyroidism, and the mean age of the group was 68 (59–89). They were all classified as ASA I and II.
The recurrent laryngeal nerve was identified in 26 (95%) out of 28 cases, and the ipsilateral parathyroid gland in 14/28 (50%). A bilateral approach was necessary in one patient (3.5%), due to a false-negative result from imaging tests.
We were obliged to undertake 4 conversions (14%) to open surgery (through a transverse cervicotomy), because multigland disease was observed during the procedures, which was not detected by the preoperative imaging tests in one case (3.5%), capsular rupture of the adenoma in another case (3.5%), and difficulties in the appropriate progression of the operation, in the first 2 cases (7%). The surgical time was 61.2 (40–90)min and no intraoperative complications were detected. The mean weight of the tissue samples was 1087mg (100–7080mg).
Post-operative morbidity included permanent damage to the recurrent laryngeal nerve in one patient, one case of haematoma of the sternocleidomastoid muscle, and a capsular rupture which required conversion; the rupture case was probably due to the presence of a large, friable adenoma.
All the patients started an oral diet within the first 12h post surgery. Pain 24h after the intervention was 2 (1–3) according to the visual analogue scale. The mean hospital stay was 1 (1–3) days.
The wounds had an excellent appearance 7 days after surgery, and were almost “invisible” 3 months after the intervention (Fig. 4).
After median follow-up of 22 (9–53) months, 2 patients continued to have hypercalcaemia after ablation of an adenoma (7%); the presence of a second ectopic adenoma was found in one patient, at the level of the mediastinum, and in the second patient, the cause of hypercalcaemia was not related to the base disease, and therefore we consider that the success of the intervention was 27/28 (96%).
DiscussionMany advantages have been demonstrated of surgical interventions performed in the peritoneal cavity via endoscopy compared to the same performed as open surgery. These results have generated an interest in developing increasingly less invasive procedures in other anatomical territories, and the first application of endoscopy in parathyroid surgery to remove the parathyroid adenomas located in the mediastinum by thoracoscopy13 was described in 1994; this avoids opening the thorax and offers the patient important advantages in these rare cases of ectopia. However, it is difficult to demonstrate the same advantages with cervical approaches, despite the wide series published by Henry et al. in the nineties14 and Miccoli et al.15 We only found 2 studies in recent medical literature which compared conventional parathyroid surgery to endoscopic techniques, and these demonstrated less post-operative pain, and better aesthetic results with the endoscopic techniques.16,17 From our experience, we believe that the use of endoscopic techniques could be better compared to the conventional approach, as it allows better quality visualisation of the surgical field (Full-HD), and greater magnification of all the anatomical structures, compared to open surgery. It is probably more difficult to achieve an adequate view of the anatomical structures through a mini-incision than with endoscopic vision.
In our study, one patient presented a permanent lesion to the recurrent laryngeal nerve in the post-operative period. We believe that the mechanism of the lesion probably occurred during the process of removing the adenoma, as the nerve was appropriately identified during the initial endoscopic dissection around the adenoma.
According to the experience of groups such as that of Marsella,14 and our experience, only some patients with primary sporadic hyperparathyroidism are candidates for this type of surgery. Patients need to be strictly selected, and it is essential to evaluate the absolute contraindications which are: large goitre, previous surgery to the area near the parathyroid, suspicion of multigland disease and difficulty in localising the adenoma on imaging tests. According to some authors, more than 60% of patients with primary hyperparathyroidism could be candidates for video-assisted parathyroidectomy.15,16 In their publication in the journal Surgery in 2001 Henry et al.18 pointed out, that the contraindications can be relative as they depend on the experience of the surgeon of the surgical technique used, thus broadening the spectrum of possible candidates for endoscopy. We shall continue to strictly select patients, and evaluate absolute contraindications, since we have no hospitals designed for the surgical treatment of endocrinological disorders and, therefore the number of patients available to us is clearly lower than that reported in the various published studies.
We had a case of glandular rupture which required conversion, probably owing to the presence of a large, friable adenoma. In the abovementioned series, large adenomas (>3cm) were not considered an absolute contraindication, especially if located in the postero-superior mediastinum,16 although surgeons with little experience might encounter difficulties when dissecting large adenomas, which might result in capsular rupture, and local dissemination of adenomatous parathyroid cells14,15; and therefore we recommend excluding adenomas over 2cm. In the case where this complication occurred we have not observed any sign of recurrence to date.
The lateral approach also enables full exploration of all the anatomical elements of the retro-thyroid area, from the upper pedicle to the postero-superior mediastinum, and therefore we consider that this procedure also applies to the cases where the parathyroid lesion is posteriorly located. In other words, the growth of the upper parathyroid glands pushes them to migrate posteriorly and slide over the paravertebral plane near to the lateral edge of the oesophagus.
According to the studies published by Henry et al.,14 amongst other authors,12,15,18 the lateral approach is also ideal for parathyroid glands located posterior to the lower poles of the thyroid lobe and, in cases where it is important to have a lateral view to enable the recurrent laryngeal nerve to be located which is in intimate contact with the adenoma and only thus can it be safely dissected; however, for lower peri-thymic locations the central approach might be preferable.
In this cohort of 28 patients who underwent lateral endoscopic parathyroidectomy sensitivity to cervical ultrasound was 95%, and 98% for MIBI nuclear-scan. We know that the result of the ultrasound is dependent on the operator and that the MIBI scan was a strong determinant of the success of the endoscopy, and therefore could explain biased results from the selection process. After overall analysis of the imaging tests, we found that half of the conversions were caused by erroneous results, one case of multigland disease which went undetected, and one case due to underestimating the size of the adenoma on ultrasound.
Unfortunately, we cannot compare our results from the patients operated using endoscopy vs the patients in whom an open approach was used, as in our case they were considered to be different groups of patients; however, our results are similar to those reported by the series published to date.15–19 Unlike open surgery where only the confidence of the surgeon in his or herself is sufficient to achieve a successful result in more than 95% of cases, a video-assisted surgeon will rely on multiple technologies, especially surgical instruments and location studies of preoperative imaging.
Amongst the minimally invasive techniques which apply to parathyroidectomy, the video-assisted technique has the important advantage of offering a magnified view, which enables precise and careful dissection thus minimising risk. In our experience, in the right setting, cervical endoscopy and open surgery could be complementary techniques.
It is very early to evaluate what the recurrence rate will be with these new techniques, and it would have to be compared with a very low rate of recurrence of the primary hyperparathyroidism after the open approach for solitary lesions.
ConclusionAlthough the endoscopic approach for sporadic primary hyperparathyroidism is feasible and reproducible, and offers results that are comparable with the traditional open approach, the technical difficulty in using this approach, which requires intensive training, together with the scarcity of clearly selectable patients (as a result of the dispersion of cases throughout the different national health service hospitals), make its use not very advisable outside hospitals with a high number of patients and different endocrine surgery departments, in which case it would form part of the range of surgical approaches which can be offered to each individual patient.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Vidal-Pérez O, Valentini M, Baanante-Cerdeña JC, Ginestà-Martí C, Fernández-Cruz L, García-Valdecasas JC. Paratiroidectomía lateral endoscópica en el manejo de pacientes con hiperparatiroidismo primario. Cirugía y Cirujanos. 2016;84:15–20.