Intussusception is defined as a segment of the gastrointestinal tract and mesentery within the lumen of an adjacent segment. It is a rare condition in adults that can occur anywhere in the gastrointestinal tract from the stomach to the rectum. Only 5% of all intussusceptions are presented in adults, and in 1–5% of all cases of intestinal obstruction. Inflammatory myofibroblastic tumour is rare, and is usually found in the lung, and rarely detected in some intestinal portions. It causes a variety of non-specific symptoms, with those that present as an intussusception being uncommon.
Clinical caseA female of 69 years with partial bowel obstruction secondary to intestinal intussusception due to an inflammatory myofibroblastic tumour, a rarely diagnosed condition and never published before.
DiscussionInflammatory myofibroblastic tumours are rare, and in this case with an atypical presentation that was surgically resolved satisfactorily. These entities are difficult to diagnose, with histopathology giving the definitive diagnosis. A literature review was performed to gather recent information about their diagnosis and treatment.
ConclusionsInflammatory myofibroblastic tumours require a high level of suspicion, as diagnosis prior to surgery is difficult. Surgery is considered the treatment of choice, requiring leaving free surgical edges to prevent recurrences.
La intususcepción se define como la invaginación de un segmento del tracto gastrointestinal y su mesenterio, dentro de la luz de un segmento distal adyacente, puede ocurrir en cualquier lugar del tracto gastrointestinal, desde el estómago, hasta el recto. En adultos es rara, representa el 5% de todas las intususcepciones, y en el 1-5% de los casos de obstrucción intestinal. El tumor miofibroblástico inflamatorio es una entidad patológica rara, generalmente benigna, con predominio en el pulmón, y rara vez se detecta a nivel intestinal, lo cual ocasiona una variedad de síntomas inespecíficos, por lo que es poco frecuente que se presente como una intususcepción.
Caso clínicoMujer de 69 años, con cuadro clínico de suboclusión intestinal secundaria a intususcepción, por un tumor miofibroblástico inflamatorio, rara vez diagnosticado y rara vez publicado.
DiscusiónLos tumores miofibroblásticos inflamatorios son raros, en este caso con una presentación atípica, resuelta quirúrgicamente de forma satisfactoria. Es una entidad de difícil diagnóstico, el cual es definitivo con el estudio histopatológico. Con la finalidad de recopilar la información actual sobre su diagnóstico y tratamiento, se realizó una revisión bibliográfica.
ConclusiónLos tumores miofibroblásticos inflamatorios requieren un alto nivel de sospecha para realizar un diagnóstico previo a la cirugía. El tratamiento de elección ante este tipo de tumores es la cirugía, en la que se deben dejar bordes quirúrgicos libres para evitar recidivas.
Intussusception is defined as a segment of the gastrointestinal tract and mesentery within the lumen of an adjacent segment. The folded intestine slips into the adjacent intestine segment, propelled by peristalsis, with consequent intestinal obstruction and ischaemia.1 Intussusception is a rare condition in an adult and can occur anywhere in the gastrointestinal tract from the stomach to the rectum. It represents approximately 1%–5% of all cases of intestinal obstruction. The mean age of presentation of intestinal intussusceptions in adults is 50, with a male/female ration of 1:1.3.2 It has been established that this condition is found in less than one out of every 1300 abdominal operations and one out of every 100 patients operated on for intestinal occlusion. Mortality by intussusceptions in adults is 8.7% for benign lesions and 52.4% for the malignant variety.2 Unlike children, in whom the majority of cases are idiopathic, intussusception in adults has an identifiable aetiology in 80%–90% of cases. Out of these, 50%–75% are due to benign diseases. Among the most common are the adhesions and Meckel's diverticulum. Other tumours include: lymphoid hyperplasia, lipomas, leiomyomas, hemangiomas and a minor proportion is idiopathic.3
Increased flaccidity of the intestinal wall facilitates intussusception.
Inflammatory myofibroblastic tumour is rare, is usually found in the lung, and rarely detected in the bowel. Some cases have been reported in the head of the pancreas and the duodenum. Although the aetiology of myofibroblastic tumours is not entirely known, the World Health Organisation classifies them as tumours of intermediate biological potential, since both local recurrence and metastases are possible, as is progression with malignant potential.3,4
The definitive diagnosis of this type of tumour is histopathological. Over 71% of inflammatory myofibroblastic tumours test positive for ALK1, which is a gene that is involved in the phenomena of vascular remodelling and angiogenesis. Its determination is genetic, in approximately 50% of cases it has a clonal rearrangement, related to the ALK locus, in chromosome 2p23, which is related to the neoplasic nature of the inflammatory myofibroblastic tumour.5 ALK1 negative has been linked to elderly patients, and it also shows many nuclear pleomorphisms and atypical mitoses.6,7 Since ALK1 positive is related to young patients, with a high recurrence, it is important to carry out the determination of ALK1, to establish disease prognosis.8,9
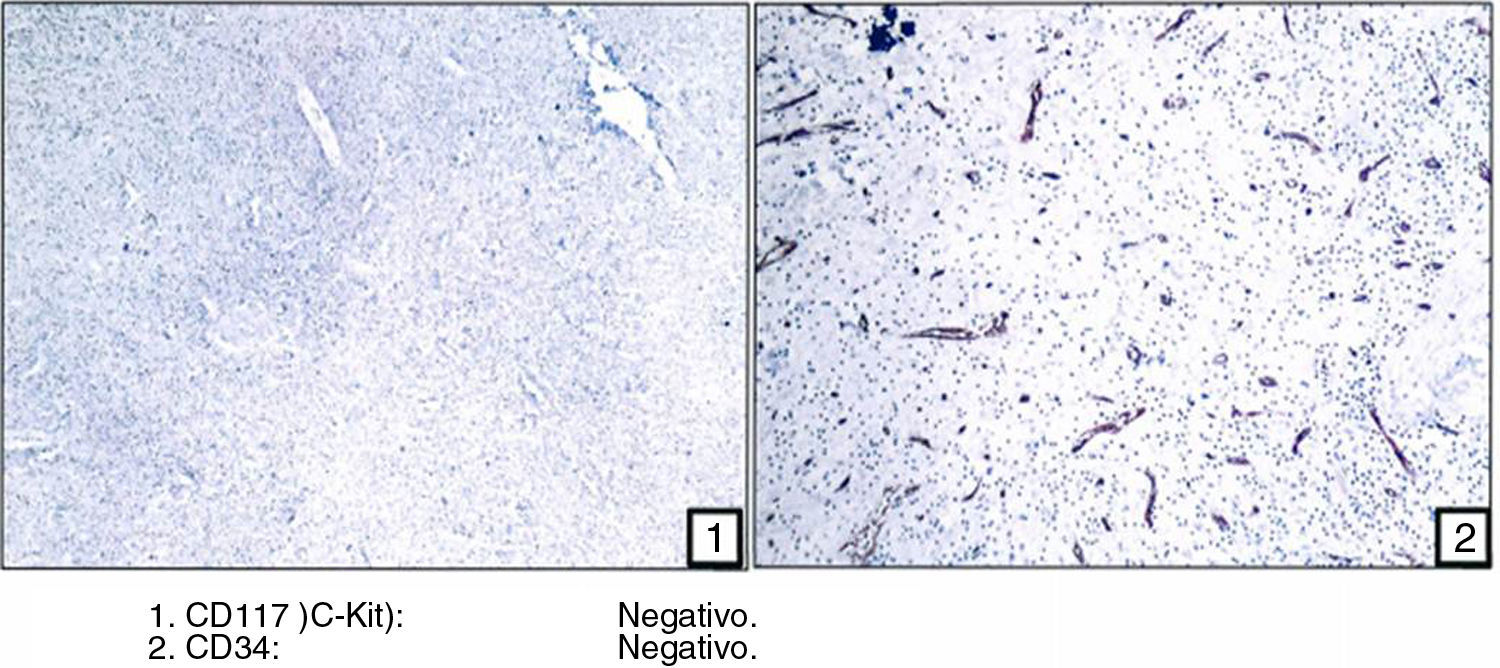
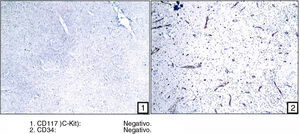
With regard to immunohistochemistry, these tumours test positive to vimetin without expression of CD 117 and CD32. The cells test positive to smooth cell actin with or without expression of desmin and S100 positive. All the previous ones are proteins expressed in the tumour tissue. They equally serve as a prognostic disease factor.10,11
Surgical resection is the treatment of choice for inflammatory myofibroblastic tumours.12 Total surgical resection is associated with a recurrence under 10%. Chemotherapy is reserved for patients where surgical resection is morbid, impossible or incomplete. There is no evidence to show that chemotherapy would be effective as monotherapy, but it may play a role after surgery.12,13 Radiotherapy is solely reserved for palliative care, with the objective being to reduce the effect of the mass, or in conjunction with chemotherapy, for managing patients who will not be referred for surgery.14,15
Steroids may be used to reduce the inflammatory process generated in the tumour periphery, particularly in tumours of the nervous system.15
Non-steroid anti-inflammatory drugs are useful in managing inflammatory myofibroblastic tumours when resection is not possible or it is limited due to the invasion of vital structures.16,17
In this article we describe a clinical case of a patient aged 69, with bowel obstruction secondary to intestinal intussusception, due to an inflammatory myofibroblastic tumour.
Clinical caseA female patient aged 69, who stated the following history of importance: mitral valve disease of 18 year onset, in treatment with warfarin; rapid response auricular fibrillation of 2 year onset, in treatment with amiodarone; cerebral vascular event, with Rankin scale IV sequelae; tumour resection in left side of colon, 10 years ago, reported as liposarcoma. A family history of a late mother who died of breast cancer, 9 years ago. No other family history of importance.
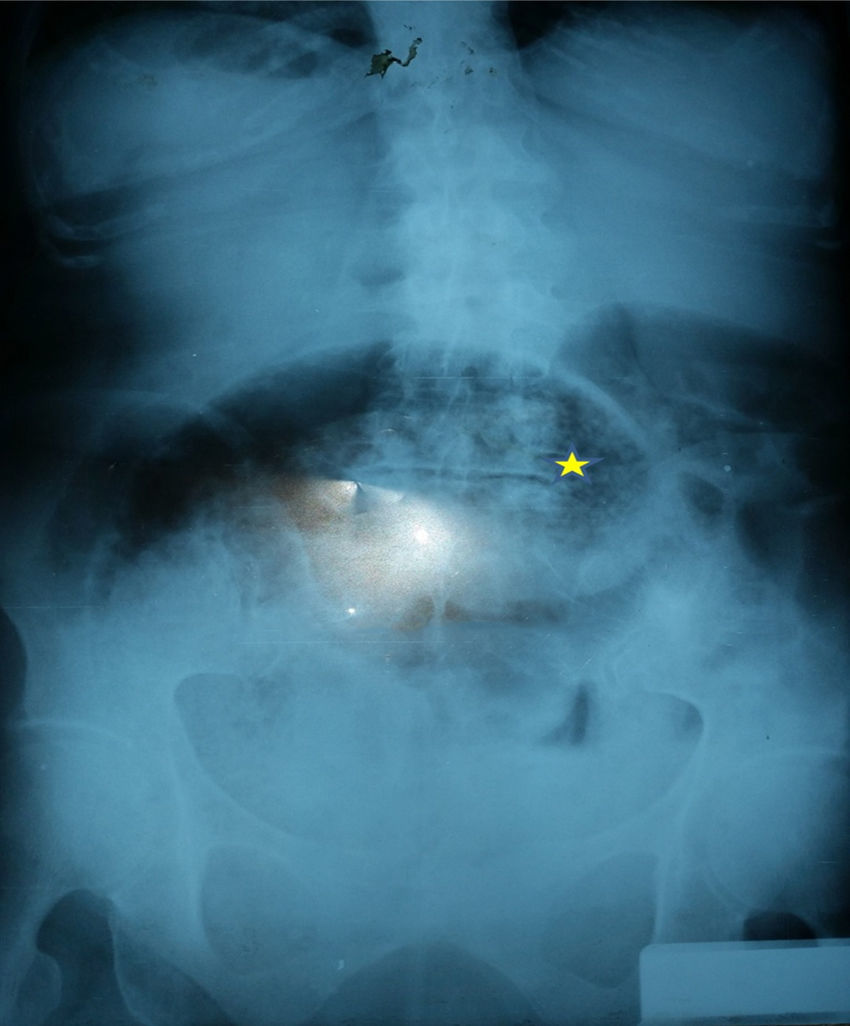
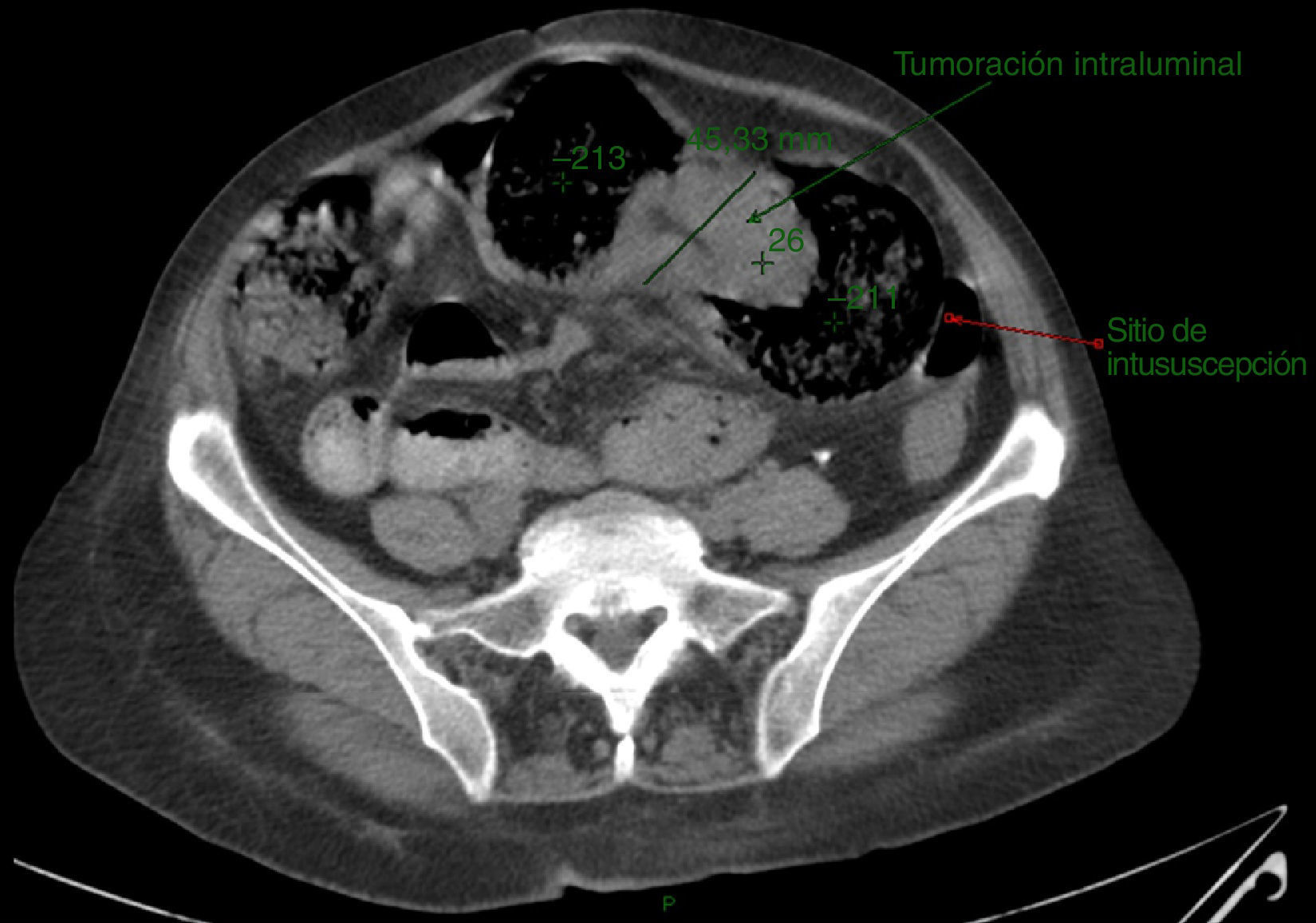
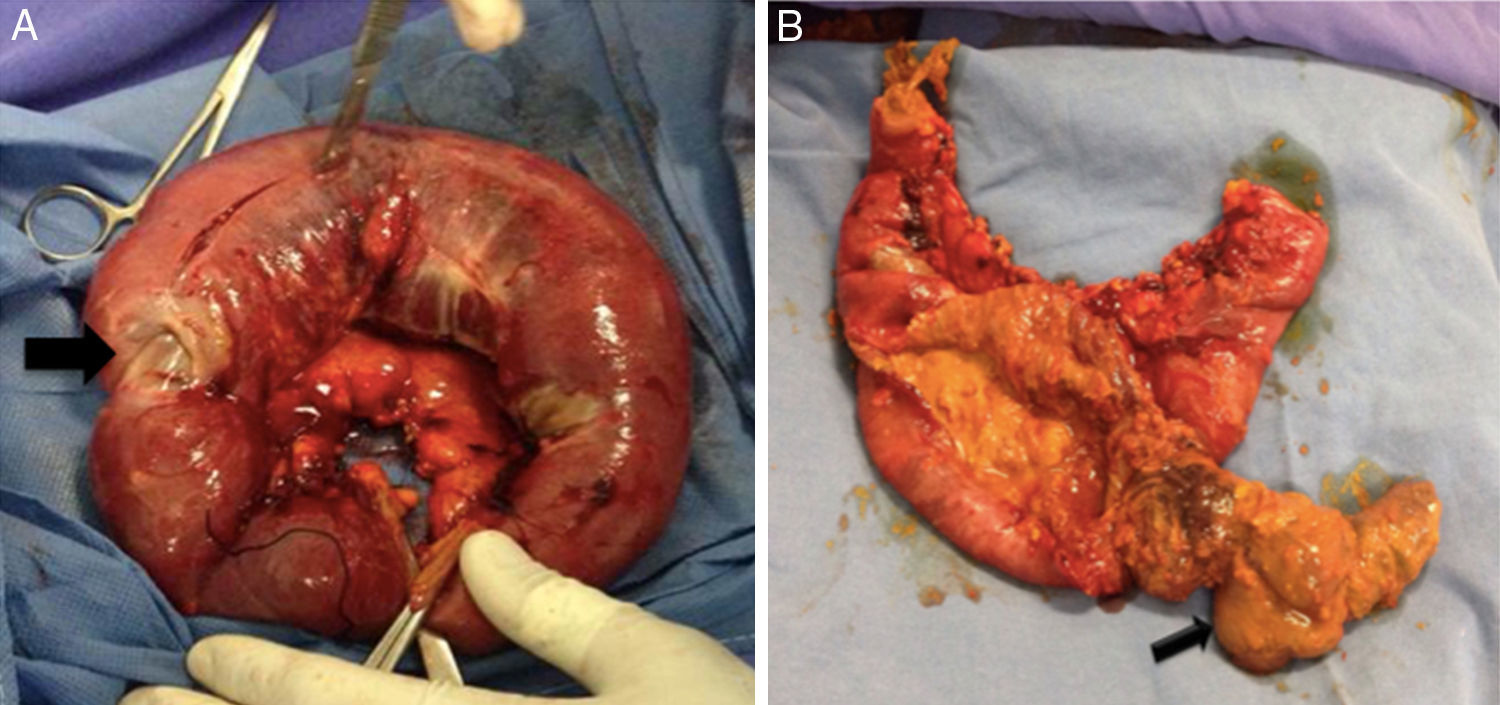
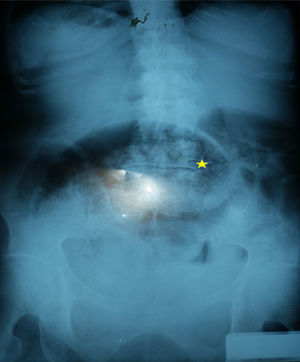
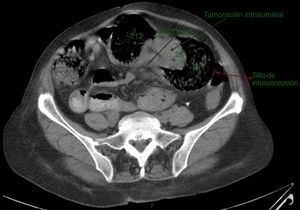
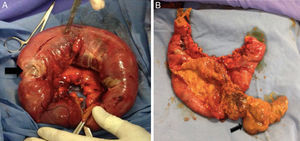
The patient was admitted to the emergency department with a partial bowel obstruction of 3 days onset. Physical examination revealed: abdominal swelling, pain on palpation, with data suggestive of acute abdomen. We decided to conduct lab tests which reported: mild leukocytosis of 13,000, with 86% neutrophilia and the presence of 4 band, red blood cells of 11.9g/dl, platelets 180,000, with a prothrombin time of 19 and a partial thromboplastin time of 33s, with INR of 1.9. A plain X-ray of the abdomen with the patient in standing position showed: one swollen small intestine loop, with no air on the rectal ampule (Fig. 1). Simple computed axial tomography showed free fluid in the cavity and thickening of the intestinal wall in the segment corresponding to the ileum, frank bloating with no signs of volvulation. An intralumen tumour was identified with reduction of loop calibre, posterior to the said tumour (Fig. 2). In the light of these findings, the following differential diagnoses were established: intestinal volvulation, and isolated abdominal adherence syndrome but the presence of intestinal tumour could not be ruled out. Given the evolution of the bowel obstruction and the previously reported findings, we decided to operate and found dilation of the proximal ileum, with frank intussusception, which presented frank changes in colouring suggestive of ischaemia (Fig. 3). Palpation of this area revealed the presence of an intralumen tumour (Fig. 4). Since there was little bowel viability we decided to resect approximately 20cm of the intestines, by manual enteroanastomosis. During her hospital stay, with considerable improvement of abdominal symptoms, parenteral nutritional support was administered. After 5 days an oral diet was re-administered with no anastomotic leakage. The patient evolved satisfactorily and was discharged from hospital, with community-based care.
The histopathological outcome was compatible with an inflammatory myofiboblastic tumour, which invaded the muscle with lymphovascular invasion. It left free borders both in the proximal and distal ends. Immunohistochemical studies confirmed this diagnosis (Fig. 5) and any possible GIST tumour was ruled out (CD 117 or C-kit negative and CD 34 negative).
DiscussionInflammatory myofibroblastic tumours are rare, of mesenchymal background and may be found anywhere in the body. This type of tumour is more common in the lung and rarer in the small intestine, as was this case, where it presented in the terminal ileum.1,2 Rarer still is its presentation as intussusception.
The behaviour of this type of tumour is benign, its aetiology is unknown, but it correlates with: Epstein–Barr virus, cytomegalovirus, autoimmune changes, collagen-vascular diseases, sclerosing mediastinitis, sclerosing cholangitis, Riedel thyroiditis, Campilobacter jejunii, and Pasteurella hemolítica, among others.3–5
Cases have been reported where an association with herpes virus 8 has been found, and an over-expression of interleukin 6 and cyclin D1, both of which have been related to the genesis of inflammatory myofibroblastic tumours.6–8
The standard clinical presentation in localised tumours in the small intestine is abdominal pain, nausea, vomiting, constipation and bowel obstruction. The case we was similar but with intussusceptions, which is a rare complication.8,9
Radiographically these tumours do not present characteristics which may distinguish them from other tumours or malignancies and for diagnosis the following is therefore required: a histopathological study together with immunohistochemical studies, vimetin stains (cellular cytoplasm stain), actin/cytokeratin and desmin (protein analysis).
In this case we found signs of bowel obstruction and therefore decided to operate. Inflammatory myofibroblastic tumours consist of: myofibroblasts, fibroblasts, lymphocytes, plasma cells, eosinophils and neutrophils, elements which must be identified for correct histopathological diagnosis.9,10
Differential diagnosis in small intestine tumours is mainly made with gastrointestinal stroma tumours, leiomyomas, lymphomas, Hodgkin's disease and fibrous histocytoma, among others.11–13
The treatment of choice is surgery, which aims at total resection of the tumour, like in the case of our patient where tumour free margins were left. In the cases where resection was not possible, because of multiple tumours or local recurrence, chemotherapy was considered.14–16
There are reports of recurrences of up to 25% and in some, with malignant transformation or metastasis, which is why follow-up is important.16 Mortality varies from 5% to 7% in cases of recurrence.17
ConclusionInflammatory myofibroblastic tumours are rare and of mesenchymal background. They are difficult to diagnose prior to surgery, and require histopathology data and immunohistochemistry screening. Total surgical resection is considered the treatment of choice. They are benign tumours but patients require follow-up due to the risk of recurrence or metastases.
FinancingNo sponsorship of any type was received for this article.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Gallegos-Sierra C, Belmonte-Chico Goerne MA, Ramírez-Jaimez J, de la Cruz-Temores S, Leonher-Ruezga KL. Intususcepción intestinal secundaria a tumor miofibroblástico en un adulto mayor. Reporte de caso. Cir Cir. 2017;85:444–448.