Osteochondromas are benign bony tumours, with only 1–4% being located in the spine. It occurs more frequently in the cervical spine, with C2 being the vertebra most affected. The neurological presentation is slow due to the growth characteristics of the tumour. Computed axial tomography is the reference method for diagnosis. Surgical management is indicated for patients with neurological impairment or pain.
Clinical caseThe first case presents a 21-year-old male with osteochondroma located in the spinous processes of L2, L3 and L4. The second case is a 20-year-old female with multiple osteochondromatosis with tumours at the right lateral mass of C1, with extension to C2 and tumours on the spinous processes of C5 and C7. Both patients presented with painful symptoms, which were resolved after surgical resection of the tumours.
ConclusionsThe rarity of these conditions, relevance of a clinical-radiographic diagnosis, and considerations required for surgical treatment are discussed here.
Los osteocondromas son tumores óseos benignos, solo el 1 al 4% se localizan en la columna vertebral; se presentan con más frecuencia a nivel cervical, siendo C2 la vértebra más afectada. La presentación neurológica es lenta debido a las características del crecimiento del tumor. La tomografía axial computada es el estudio de elección, para diagnóstico y programación quirúrgica. El manejo quirúrgico está indicado para pacientes que presentan deterioro neurológico o dolor.
Casos clínicosEl primer caso se trata de un paciente masculino de 21 años, con diagnóstico de osteocondroma localizado en los procesos espinosos de L2, L3 y L4. En el segundo caso; una paciente femenina con osteocondromatosis múltiple, que presenta tumoraciones a nivel de la masa lateral derecha de C1 con extensión a C2 y procesos espinosos de C5 y C7. Ambos pacientes cursan con sintomatología dolorosa, la cual remite posterior a la resección quirúrgica de los osteocondromas.
ConclusionesSe realiza un reporte de casos y revisión de la literatura, para ejemplificar los diversos síntomas que causan los osteocondromas espinales. El conocimiento y la sospecha de este tipo de tumores permiten brindar el manejo apropiado; según su localización y sintomatología.
Osteochondromas are benign tumours, and represent 8.5% of all bone tumours and around 36% of benign bone tumours.1,2 They present as single or multiple lesions; the latter are termed multiple osteochondroma.3
The long bones are most affected; only 1–4% of osteochondromas are found in the spinal column.2–4 They are more common in men with a ratio of 1.5:1; in the second or third decades of life,5 and the degenerative changes in the spine can contribute to the onset of symptoms.6,7
The clinical manifestations vary, the main symptom is pain. Neurological manifestations seldom present, as the lesions generally grow outside the medullary cavity.3,8,9 Radiculopathy can present acutely, secondary to trauma,5 or can cause paresthesias, due to the tumour's slow-growth pattern.10–12
The most common location of osteochondromas is in the cervical spine, at 50%,13 chiefly C2,14–16 followed by C3 and C6.5,6 The thoracic region is the second most common location, 28% of these lesions.6,17
Clinical casesFirst caseA 21-year old male patient, presenting with a one-year history of low back pain, classified as 2/10 based on an analogue visual scale, and increased volume at lumbar level. He attended a reference institution for assessment. In his initial assessment, increased volume was found in the lumbar region at L2 level, immobile, adhered to the deep planes, with mild pain on palpation only, and no changes to the overlying skin.
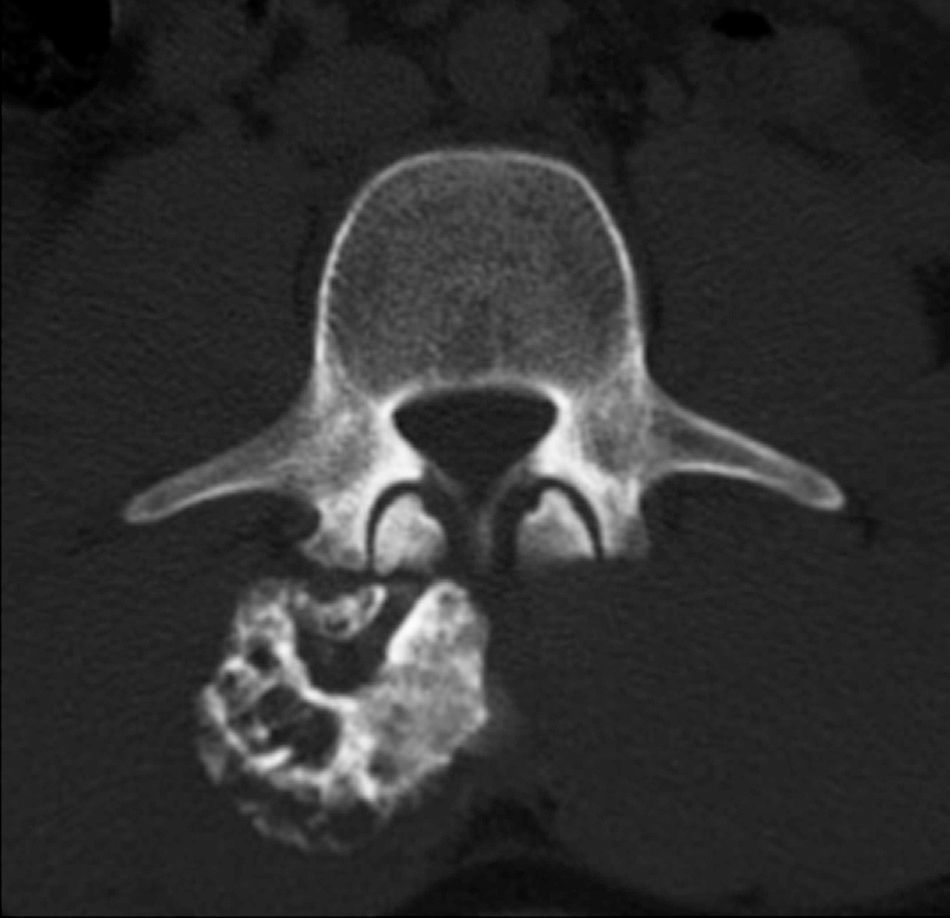
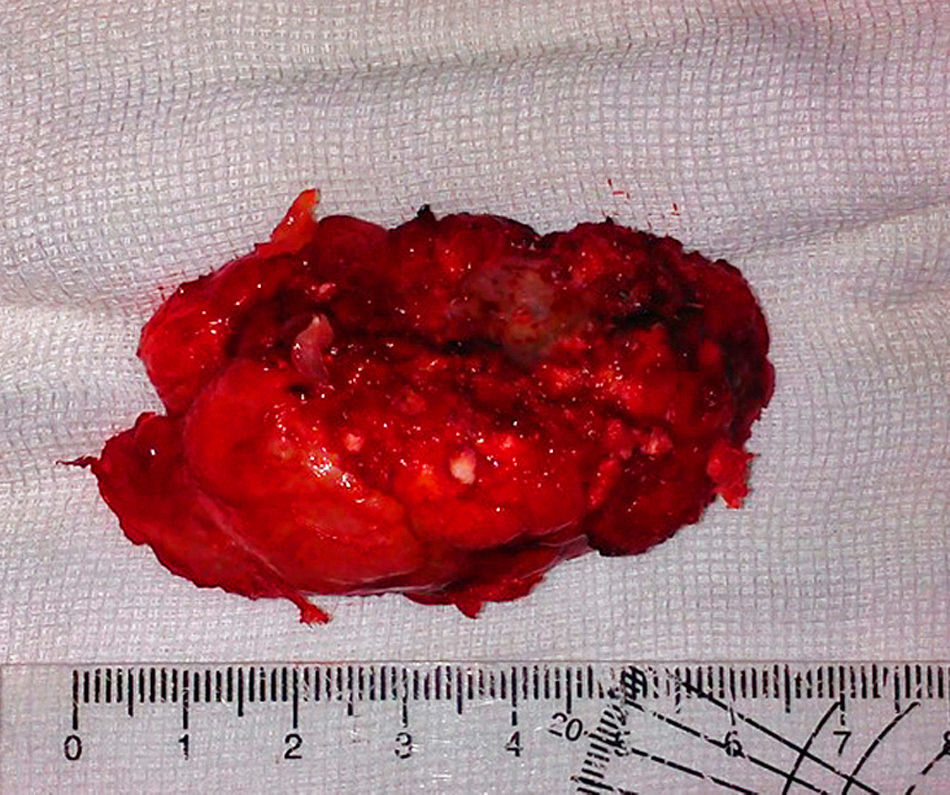
Neurologically, both pelvic extremities had sensitivity 2/2, and muscle strength 5/5, normo-reflective, no pathological reflexes evoked, and no signs of neurotension. The anteroposterior and lateral radiographic views of the lumbosacral spine showed a radio-opaque, pedunculated tumour, next to vertebral bodies L3 and L4 and the spinous process of L2 (Fig. 1). The following were considered as differential diagnoses: chondrosarcoma, osteoblastoma, and connective tissue disorders, such as dermatomyositis of heterotopic ossification. The radiographs were complemented with computed axial tomography (CAT) which showed a tumour arising from the spinous processes of L2, L3 and L4, with no invasion of the spinal canal (Fig. 2). Due to the patient's increasing pain, even when lying down, an en bloc resection was performed, obtaining a bone tumour with a cartilaginous cap 7cm×3cm×2cm, pedunculated to L2, L3, and L4 spinous processes, and lamellae (Fig. 3). With a histopathological diagnosis of osteochondroma without atypia. The patient is currently asymptomatic, with muscle strength 5/5, sensitivity 2/2, and normo-reflective.
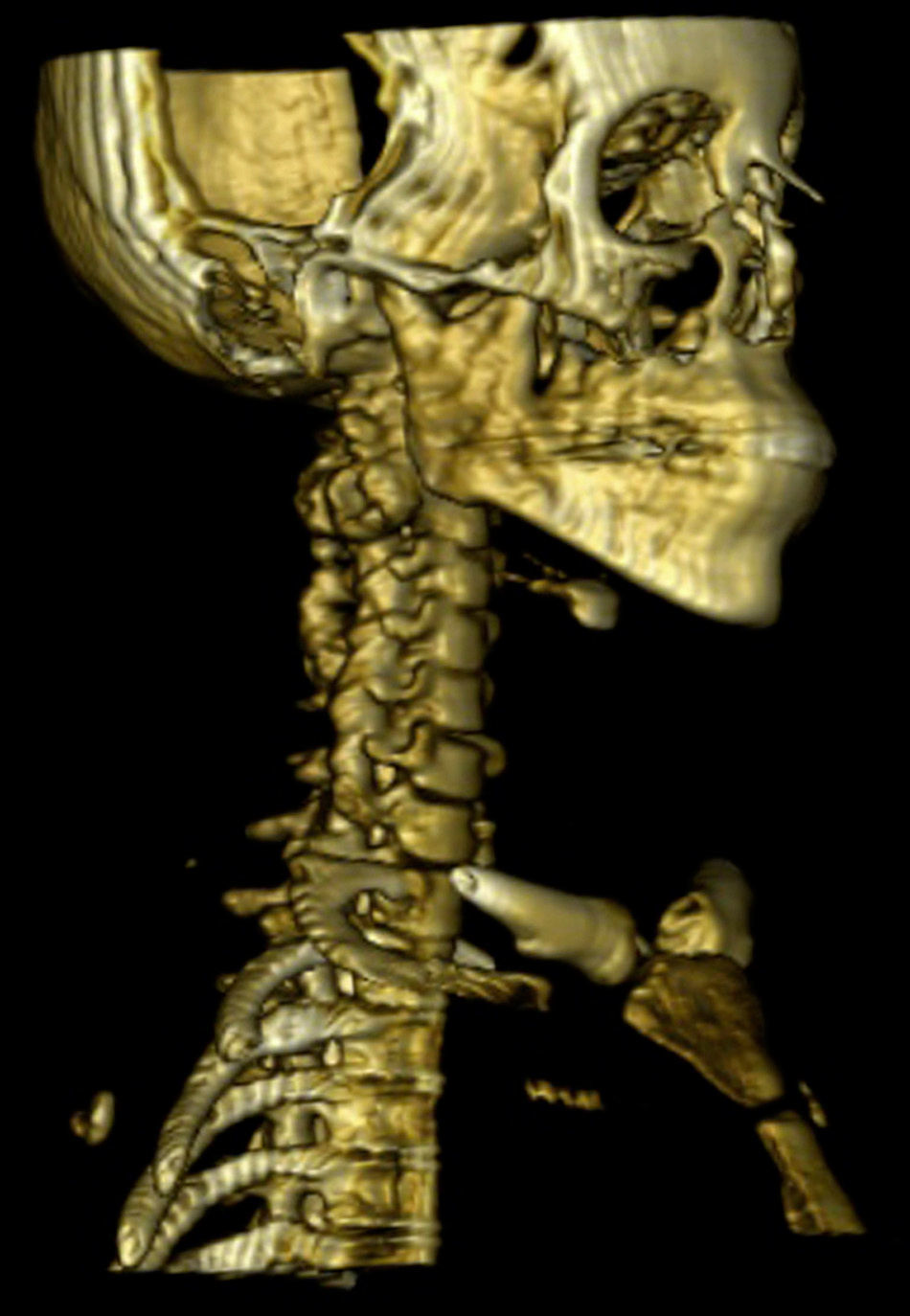
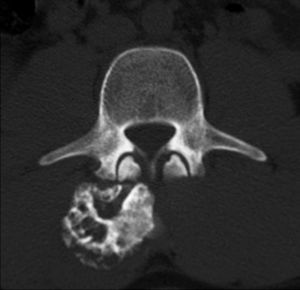
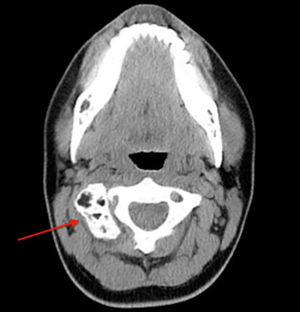
A 20-year old female patient, diagnosed with multiple osteochondromatosis since the age of 2. She attended for assessment with a 3-month history of pain in the cervical region, accompanied by paresthesias in the right thoracic limb, crushing pain of 4/10 intensity based on an analogue visual scale, exacerbated by flexion and right rotation to an intensity of 6/10, she did not report dysphagia. Increased volume in the right cervical region at C2 level of 2cm×2cm was found on physical examination, immobile, and adhered to deep planes, with pain of mild intensity on palpation, and no changes to the overlying skin. Neurologically, she had 2/2 sensitivity in the thoracic limbs, muscle strength 5/5, normo-reflective, with no signs of neurotension, no pathological reflexes evoked. X-rays showed a radio-opaque tumour 19mm×29mm, pedunculated to the right lateral region of C1 extending to C2, and a tumour in the spinous process of C5 and C7. Due to the patient's history of multiple osteochondromatosis, a diagnosis of osteochondroma was highly suspected. The study was complemented with unenhanced tomography, which recorded bone neoformation involving the right lateral side of C1, extending to C2 with moulding of the intervertebral foramen (Fig. 4), osteochondroma in the left lamella, and spinous process of C5, and C7. Finally, bone and vascular reconstruction of the cervical column showed moulding of the horizontal segment of the right vertebral artery due to the tumour growth, without obliterating its lumen, and with no invasion towards the spinal canal (Figs. 5 and 6).
The patient was scheduled for resection of the osteochondroma, due to her symptoms, and the proximity of the tumour to the vertebral artery. It was partially resected obtaining multiple fragments of tissue, which were small and irregular in shape, measuring together 2cm×2cm×1cm, of hard consistency and yellowish-white in colour. The presence of hyaline cartilage with no atypias was found under the microscope, and areas of endochondral ossification, and spongy bone with haematopoietic elements in the intertrabecular space. A diagnosis of osteochondroma was made.
The patient is currently asymptomatic, with a eutrophic scar, full range of movement of the cervical column, and neurological examination shows muscle strength 5/5, sensitivity 2/2, and preserved reflexes.
DiscussionOsteochondromas arise through a process of endochronal ossification of aberrant cartilage at the growth plate, as a consequence of congenital defects or trauma.12,18 Albretch et al.3 indicate that the predominance of these lesions at cervical level is due to microtraumas suffered by the cartilage of the growth plate because this vertebral segment is highly mobile and flexible: thus, the vertebral regions which are most affected should be the cervical and the lumbar regions, however, there is a greater incidence of lesions found in the lumbar region.19–23 Another theory suggests that secondary ossification centres in the spinous, transverse and articular processes appear between 11 and 18 years of age, and ossify in the cervical region during adolescence, and in the thoracic and lumbar regions in the second decade of life.24 The cartilage of these secondary ossification centres could be the source of aberrant cartilage tissue, which results in the formation of an osteochondroma. It is speculated that the faster the ossification process of these centres, the greater the probability of the formation of aberrant cartilage tissue; this explains the greater incidence in the cervical region. Osteochondromas generally arise in the pedicles, in the lamella or in the vertebral body.23
These bony tumours can be solitary or multiple. Multiple osteochondromatosis, also known as hereditary multiple exostoses, is an autosomal dominant inheritance disorder, transmitted by the father, with incomplete penetration in women. The incidence of the condition is 1 in 50,000. The severity of the disorder varies, and the determinants have as yet not been established. Genetic variations play a major role and 3 specific loci have been identified in the genome: EXT1 (18q), EXT2 (11p) and EXT3 (19p). The involvement of the vertebral column occurs more often in hereditary multiple exostoses, both types affect men more than women.6
It is difficult to diagnose osteochondromas in the spine by radiography, due to the superimposition of several structures on the image depending on the projection taken,25–28 and they have been found to be insufficient in up to 79% of cases, therefore computed axial tomography is advocated.5,29
The pathognomonic features of the lesion by computed axial tomography are the presence of sessile or pedunculated growths which present continuity between the cortical bone and the spongy tissue of the vertebral body from which they arise.23 Spinal exostoses can be better visualised on computed axial tomography than with magnetic resonance, due to the bone characteristics of the lesion.30
Magnetic resonance is recommended in patients with radiculopathy in order to observe the level, and the extent of neurological compression.5 On this, a prominent peripheral hypointense border can be seen corresponding to ossification, and a small central core isointense to that of the bone marrow, giving a “bullseye” appearance.5
These lesions are managed by surgical resection, if they present symptoms.31 Recurrence of the disorder after surgical treatment is rare, and is due to incomplete resection of the lesion.3,8,16
Recurrence of the lesion, associated with accelerated and sudden growth of the osteochondroma, can be indicative of malignancy in the future, which occurs in 1% of isolated lesions, and in 5–25% of patients with multiple lesions.2,30 Malignancy should be suspected when magnetic resonance imaging shows the cartilage cap to be greater than 2cm in adults and greater than 3cm in children.30
In our cases, like those regularly reported in scientific literature, location in the neural arch is the cause of symptoms, and although rare, it is known that the main diagnosis is in this area.31
ConclusionsOsteochondromas are benign tumours formed from bone with a cartilage cap. They present very rarely in the spine; however, they can be managed appropriately if a suspected diagnosis is established. Surgical treatment involves resection of the tumour, and is the ideal method of treatment; it relieves the symptoms almost immediately, and also provides good functional results, since there are low rates of complication and relapse following surgery.
Conflict of interestsThe authors have no conflict of interest to declare.
Please cite this article as: García-Ramos CL, Buganza-Tepole M, Obil-Chavarría CA, Reyes-Sánchez AA. Osteocondroma espinal: diagnóstico por imagen y tratamiento. Reporte de casos. Cir Cir. 2015;83:496–500.