Tele-cardiology is the use of information technologies that help prolong survival, improve quality of life and reduce costs in health care. Heart failure is a chronic disease that leads to high care costs.
ObjectiveTo determine the effectiveness of telemetric monitoring for controlling clinical variables, reduced emergency room visits, and cost of care in a group of patients with heart failure compared to traditional medical consultation.
Material and methodsA randomised, controlled and open clinical trial was conducted on 40 patients with heart failure in a tertiary care centre in north-western Mexico. The patients were divided randomly into 2 groups of 20 patients each (telemetric monitoring, traditional medical consultation). In each participant was evaluated for: blood pressure, heart rate and body weight. The telemetric monitoring group was monitored remotely and traditional medical consultation group came to the hospital on scheduled dates. All patients could come to the emergency room if necessary.
ResultsThe telemetric monitoring group decreased their weight and improved control of the disease (p=0.01). Systolic blood pressure and cost of care decreased (51%) significantly compared traditional medical consultation group (p>0.05). Admission to the emergency room was avoided in 100% of patients in the telemetric monitoring group.
ConclusionIn patients with heart failure, the telemetric monitoring was effective in reducing emergency room visits and saved significant resources in care during follow-up.
La telecardiología es el uso de tecnologías de la información que permiten prolongar la supervivencia, mejorar la calidad de vida y reducir costos en la atención de la salud de algunas enfermedades como la insuficiencia cardíaca.
ObjetivoDeterminar la eficacia del seguimiento telemétrico para el control de variables clínicas, disminución de visitas a urgencias y costo de atención en un grupo de enfermos con insuficiencia cardíaca en comparación con la consulta médica tradicional.
Material y métodosEnsayo clínico aleatorizado, controlado y abierto en 40 enfermos con insuficiencia cardíaca en un centro de tercer nivel de atención del noroeste de México. Aleatoriamente se formaron 2 grupos de 20 enfermos cada uno (seguimiento telemétrico, consulta médica tradicional). Las variables evaluadas fueron: presión arterial, frecuencia cardíaca y peso corporal. El grupo de seguimiento telemétrico se vigiló a distancia y el grupo de consulta médica tradicional acudió en fechas programadas al hospital. Todos podían acudir al servicio de urgencias en caso necesario.
ResultadosEl grupo de seguimiento telemétrico redujo su peso y mejoró el control de su enfermedad (p = 0.01). La presión arterial sistólica disminuyó significativamente (p > 0.05). El coste de atención se redujo en el grupo de seguimiento telemétrico (51%), en comparación con el grupo de consulta médica tradicional. Se evitó el ingreso a urgencias en el 100% de los enfermos del grupo de seguimiento telemétrico.
ConclusionesEn enfermos con insuficiencia cardíaca, el seguimiento telemétrico fue efectivo en disminuir las visitas a urgencias y ahorró significativamente recursos en la atención durante el seguimiento.
The incidence of chronic cardiovascular diseases is a major problem worldwide.1,2 The heart failure incidence is estimated in 5 per 1000 inhabitants annually; and it doubles every decade of life from 45 years on.3 It represents a common cause of hospital admission in people over 65 years.4 Heart failure is included among the chronic diseases that contribute most to the world burden in terms of care.5 This care has been estimated to cost than U$S10 billion annually, which is, to a great extent, due to a high annual number of decompensations.6 For this reason during recent years, several initiatives to improve the services provided to these patients have been developed.7 Among the actions proposed is home-based multidisciplinary care with health care personnel, which has promising results, although it is difficult to apply on a large scale and is expensive.2 Patients with decompensated cardiac failure always require urgent medical attention from a specialist, a situation that cannot always be resolved in a scheduled home visit.
At present there are new therapeutic options that use information technology which, from outside the hospital premises, may facilitate medical attention.3,4 One of these methodologies is telemedicine, which is the application of the most advanced telecommunication technologies for therapeutic, follow-up and monitoring purposes.8 In particular, telecardiology is a highly developed medical discipline that involves almost all the aspects of cardiology, including the study of the acute coronary syndromes, disrhythmia, congestive cardiac failure, and sudden cardiac arrest, among others. The aims of telecardiology include improving the quality of life and survival of the patient, and to significantly reduce health costs.9 Telecardiology or cardiac telemetry is characterised as a non-invasive, individualised methodology that offers the double advantage of both providing a greater degree of control and promoting the patients participation in the management of their illness. This is also a way to reduce hospital visits that happen due to poor control situations. Through this methodology, patients are treated in their normal surroundings,10,11 as it allows for the remote monitoring of main indicators of cardiovascular decompensation, body weight, heart rate and blood pressure. All of these are important indicators of cardiovascular decompensation.12
Patients are able to make their consultation remotely from the comfort of their home through the use of sensors equipped with a Bluetooth system for voice and data transmission. Data are sent automatically to a digital platform located inside the hospital. Before follow-up starts, the setting of the alarms for each variable is performed, such as the systemic blood pressure, heart rate and body weight values. In the event that the parameters exceed the established value of reference, the doctor will indicate changes in the diet and/or medical treatment to revert the tendency to decompensation, avoiding unnecessary visits to the A&E department.10,12
The Instituto Mexicano del Seguro Social offers a model of care through a technological platform that integrates related services and technological support into a multidisciplinary care network.13 For this reason, the aim of this study was to determine the efficacy of telemetry monitoring in the control of body weight, heart rate and blood pressure, and in the reduction of the decompensation risk, emergency room visits, and the healthcare costs in a group of patients with chronic cardiac failure, compared with standard ambulatory follow-up.
Material and methodsStudy designA randomised, controlled and open clinical trial was conducted on 40 patients with a diagnosis of chronic heart failure selected from the Cardiology Service external offices in a tertiary care centre in north-western Mexico. The study was conducted from August 2011 to February 2012.
Prior to the beginning of the study, approval was obtained from the Local Ethics and Research Committee of the Hospital de Especialidades No. 2, of the Centro Médico Nacional del Noroeste in Obregón City, Sonora, Mexico.
Selection criteriaPatients from both genders diagnosed with heart failure and New York Heart Association functional class IV were selected. Each participant needed a relative committed to participate in the study14; both had to live within the coverage and mobile phone signal zone, and to sign an informed consent form accepting responsibility for taking care of the unit they would be supplied with, and to strictly comply with the instructions from the doctor. Among the exclusion criteria were: having an ontological or infectious disease; having chronic renal failure, following peritoneal dialysis or haemodialysis programmes, and being bedridden for cerebral vascular disease sequelae. The reasons to reject a case from the study were: the need to use a resynchroniser, to have undergone a revascularisation procedure or a percutaneous intervention, to have moved or changed residency, and to abandon the study for any cause, including death.
ProceduresThe patients were randomly divided into 2 groups: telemetry-monitored group and the traditional medical consultation group. The patients in the telemetry-monitored group received digital aneroid sphygmomanometer (A&D, model: UA-851 Premium Blood Pressure), a floor scale, and an Alcatel® mobile phone. All the devices provided had access to a wireless personal area network through Bluetooth which allows for voice and data transmission via 2.4GHz ISM radio frequency band connection.
All the measurements of the patients were sent to a receiving platform located in the hospital, where nurses would do the follow-up from 8:00 a.m. to 4:00 p.m. If any changes in the monitored parameters of the patient were detected, the nurse would immediately notify the doctor so that new instructions could be issued to the patient.
For the traditional medical consultation group, the patients attended the external appointments on the set dates, according to the schedule established and marked in each patient's agenda of visits. The participants from both groups were given a medical appointment booklet so that if they needed medical attention they could seek it in the A&E department. In this book, the emergency doctor would record the event, the clinical attributes of the patient on arrival, the clinical condition presented, and the treatment provided until discharge.
Economic assessmentIn addition to the clinical results for each patient, the data collected relating to the resources used for medical attention included: (a) hospitalisations, (b) attention from the casualty department, family doctor and consultant (cardiologist), (c) the medical tests and procedures, and (d) the names and doses of medications prescribed and the extra medications administered in case of uncontrolled disease, as stated in the record of expenses of each patient. The costs of the A&E department visit and hospitalisations were estimated, based on the comments entered in the medical records. Losses of productivity (incapacity) were not included in the analysis because the patients were not active workers.
Statistical analysisAll the information was stored in a database with the help of the SPSS® version 19.0 software for Windows® (IBM Corporation, USA). For the numerical and ratio variables, a descriptive analysis was conducted using measurements of central and dispersion tendency. The dichotomous and categorical variables were initially described by means of absolute frequencies and percentages. The Mann–Whitney U test was used to measure the differences within and between groups of the variables of weight, heart rate, and systolic and diastolic blood pressure. The actions instructed by the doctor were analysed with the Kruskall–Wallis test to eliminate the high-variability effects. Dichotomous and categorical variables were tested by means of the x2 of McNemar test to determine treatment changes among groups. The value p≤0.05 was considered to be statistically significant.
ResultsThe traditional medical consultation group comprised 14 males (70%, 95% CI: 50–90) with an average of 69±8 years, and 6 females (30%, 95% CI: 10–50) with an average of 68±7 years. The telemetry-monitored group consisted of 12 males (60%, 95% CI: 39–81) with an average age of 68±7 years and 8 females (40%, 95% CI: 19–61) with an average of 67±9 years. Most of them were married and all were living with some relative, their carer.
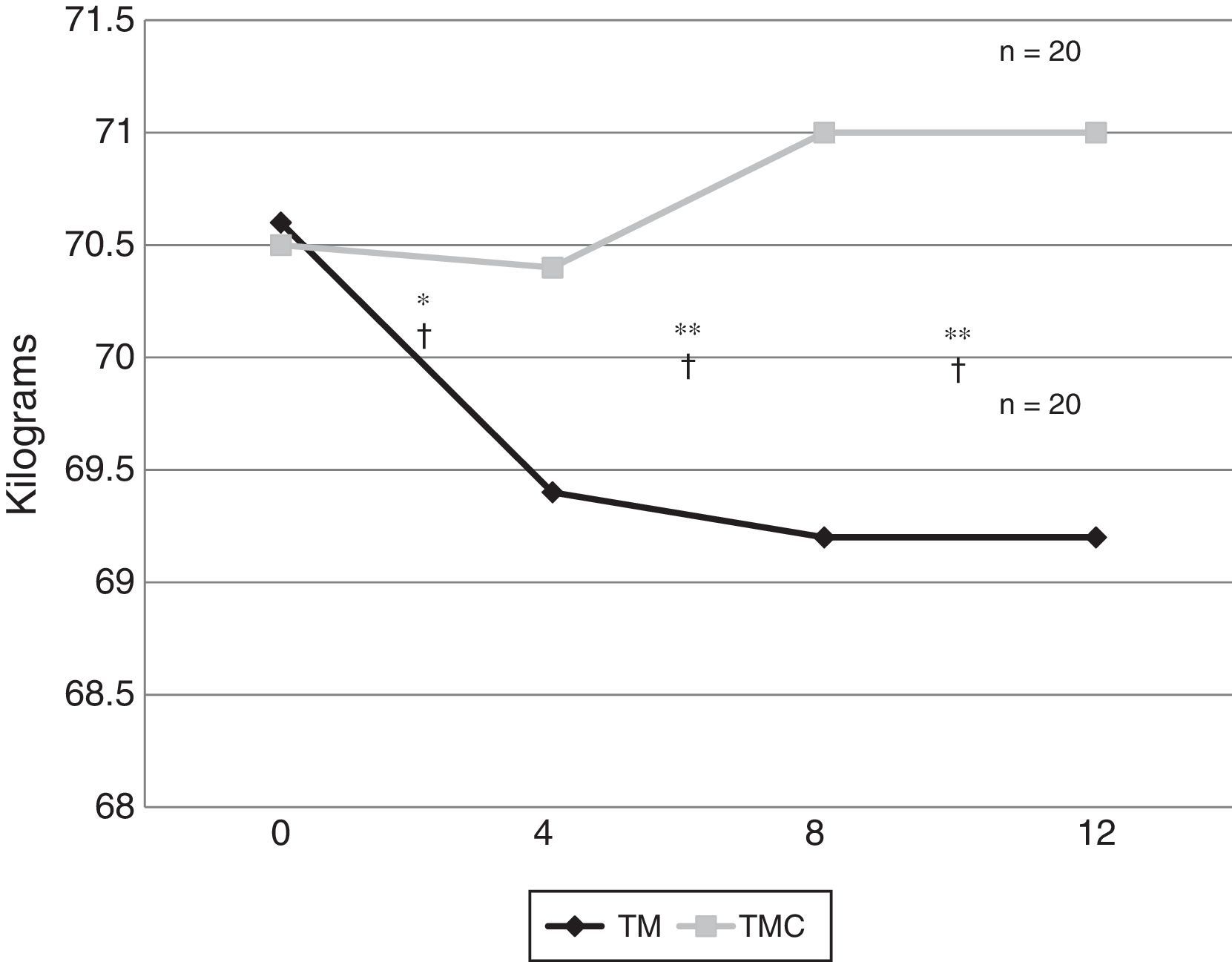
The initial body weight was similar in both groups; however, at the end of the study, the telemetry-monitored group showed an average reduction of 1.3kg from the fourth week of follow-up (p=0.01). Fig. 1 shows the comparison of the body weight averages between both treated groups at weeks 0, 4, 8 and 12 of follow-up.
The comparison of the average body weights between both groups at weeks 0, 4, 8 and 12 of follow-up. TMC: traditional medical consultation group; n: number of participants; TM: telemetry-monitored group.
*Value of p calculated with Mann–Whitney U test (p=0.01).
**Value of p calculated with Mann–Whitney U test related to the baseline (p=0.001).
†Value of p calculated with Mann–Whitney U test between groups (p=0.01).
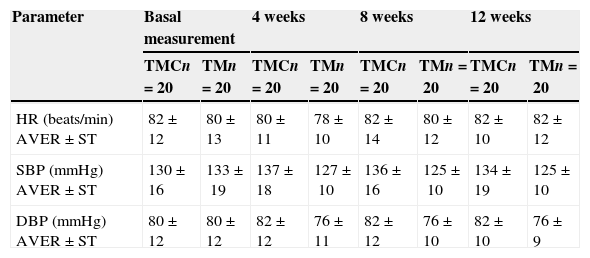
Regarding the physiological variables, neither the heart rate nor the diastolic blood pressure presented significant changes in any of the groups. Nevertheless, the reduction in the average systolic blood pressure of the telemetry-monitored group was significant compared with that of the traditional medical consultation group, which went from 133±19mmHg to 125±10mmHg (p>0.05). Table 1 shows the comparison of average heart rate and blood pressure between both study groups at weeks 0, 4, 8 and 12 of follow-up.
Average and standard deviation of the heart rate and the blood pressure by group according to weeks of follow-up.
| Parameter | Basal measurement | 4 weeks | 8 weeks | 12 weeks | ||||
|---|---|---|---|---|---|---|---|---|
| TMCn=20 | TMn=20 | TMCn=20 | TMn=20 | TMCn=20 | TMn=20 | TMCn=20 | TMn=20 | |
| HR (beats/min) AVER±ST | 82±12 | 80±13 | 80±11 | 78±10 | 82±14 | 80±12 | 82±10 | 82±12 |
| SBP (mmHg) AVER±ST | 130±16 | 133±19 | 137±18 | 127±10 | 136±16 | 125±10 | 134±19 | 125±10 |
| DBP (mmHg) AVER±ST | 80±12 | 80±12 | 82±12 | 76±11 | 82±12 | 76±10 | 82±10 | 76±9 |
TMD: traditional medical consultation; SD: standard deviation; HR: heart rate; mmHg: millimetres of mercury; DBP: diastolic blood pressure; SBP; systolic blood pressure; AVER: average; TM: telemetry monitoring.
Statistical analysis with ANOVA without significant differences.
Regarding the cost of medical care, the traditional medical consultation group was observed to have an average cost of $14,185.90 Mexican pesos per patient, in contrast with the much lower average cost of the telemetry-monitored group, $8642.10, with a real difference in savings by patient of $5543.00 Mexican pesos.
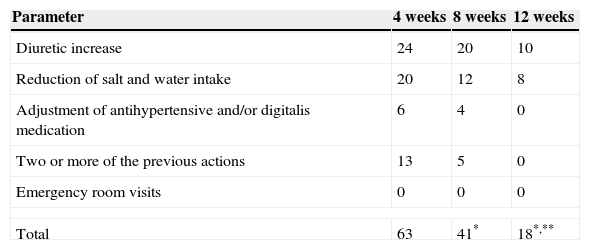
During the study, the doctor indicated 63 modifications to the treatment in the telemetry-monitored group during the first four weeks of follow-up; 41 corrections at week 8; and 18 in the third period (p=0.001), avoiding the A&E admission for decompensation in 100% of the patients. In the traditional medical consultation group, the treating doctor did not introduce any modification to the prescription of medications in the monthly visit, as patients were asymptomatic the time of consultation. However, 20% of the patients had decompensation and attention was necessary in the emergency room, with no severe complications in their diseases. None of the patients died during the conduct of the study. Table 2 shows the number of times the doctor indicated, via telephone, corrections to the treatment of the patients of the telemetry-monitored group.
Number of times that doctor indicated some action via telephone to the patients of the telemetry-monitored group.
| Parameter | 4 weeks | 8 weeks | 12 weeks |
|---|---|---|---|
| Diuretic increase | 24 | 20 | 10 |
| Reduction of salt and water intake | 20 | 12 | 8 |
| Adjustment of antihypertensive and/or digitalis medication | 6 | 4 | 0 |
| Two or more of the previous actions | 13 | 5 | 0 |
| Emergency room visits | 0 | 0 | 0 |
| Total | 63 | 41* | 18*,** |
Kruskall–Wallis: *p=0.001.
McNemar for the study of related populations before-after: **p=0.01.
The demand for medical care in the A&E department has increased exponentially.15 Chronic diseases are the main cause of this problem,16,17 contributing to service saturation and affecting both space and administrative aspects. In the case of patients with chronic heart failure, the regular control through traditional medical consultation in the Instituto Mexicano del Seguro Social is carried out via monthly scheduled appointments, which are registered in a medical record; but this greatly depends on the attending doctor's schedule and availability.
In our study, the monitoring of both groups was based on highly predictable variables of a known haemodynamic imbalance, although the telemetry-monitored group presented daily variations and changes in the body weight at the end of the study. Regarding systolic blood pressure and heart rate, there were no significant changes during the conduct of the study; but this may be more related to a bias due to the way in which variables were measured (once every four weeks) and it is not necessarily a sign of lack of therapeutic effect in the patients. This is consistent with meta-analysis studies showing the existence of better clinical results with the telemetry-monitored support and the use of phone call, rather than with the traditional medical attention only.18,19 However, in patients of advanced age, the remote monitoring does not reduce the number of hospitalisations or visits to A&E.20 In our cases, age seems not to have influenced the result of the telemetry monitoring, and we think that this is due to the fact that from the beginning of the study, one of the conditions was that there should be a relative collaborating with the monitoring and with the patient, complying with the doctor's instructions. On the other hand, despite of the tendency to the reduction of the systolic blood pressure in the telemetry-monitored group, there were no significant changes in the global values of the blood pressure or in the heart rate in both groups, as has been observed in other studies.19
In this study we could observe that the remote monitoring allowed the treating physician to identify the early warning signals associated to fluid retention, and to reestablish dietary adherence or modify the medication dose to avoid the appearance of complications.
It is important to mention that there were no emergency admissions among the telemetry-monitored group, which is consistent with other studies on home intervention, whether in the form of a home visit or any type of remote intervention, where it has been demonstrated there was a tendency towards the reduction of unplanned hospital readmissions, a reduction in the number of hospitalisations, a better quality of life, and a reduction in the health care costs or in mortality from any cause.12,19–21
Regarding the group on traditional follow-up care, four patients experienced uncontrolled heart failure, which promoted medical attention in the emergency department due to a clinical condition of acute pulmonary oedema, a widely known situation, the result of the vulnerability of these patients to easily unbalance their haemodynamics.2,3,5 These episodes did not coincide with the scheduled day of the appointment and for this reason they frequently presented themselves at A&E with complications from their underlying condition.
In the cost analyses performed, the care expenditure generated in the telemetry-monitored group was much lower than it was in the traditional medical consultation group. The above was translated into a significant actual saving per patient, which was 51% of the traditional medical consultation cost. This suggests that the longer these technologies to monitor patients with chronic heart failure are used, the greater the savings in financial, health care, and human resources will be. Similar results were showed by Ricci et al.22 in their TARIFF study in Italy, an economic assessment that compared the use of telemetry monitoring and ambulatory medical attention. The study concluded that the remote monitoring systems can improve the ambulatory follow-ups, sparing human and economic resources, and increasing patient safety.
Among the deficiencies of this study, we may mention the small size of the sample, although the number of participants was correlated with the number obtained from the differences in proportions tested in controlled clinic trials; and it was also subject to the number of devices available at the time of performing the study. However, the results are promising and justify the conduct of new studies in which this type of technological strategy for the care of patients with chronic diseases is evaluated. It was interesting to observe how the indications made in the telemetry-monitored group began to diminish as the follow-up weeks went by. This could be probably explained by the fact that patients learnt how to recognise the normal parameters and those warning signals alerting to a genuine risk. However, this observation could not be corroborated, since it was not the aim of the study. Finally, a comparative evaluation of the modification in the quality of life of the participants subjected to these two care strategies was not carried out. This last aspect could be an interesting line to explore in future research due to the clinical repercussion that it entails in the development of a chronic disease.
Although it was not the aim of this study, it would also be interesting to conduct a comparative analysis of the costs associated with standard ambulatory follow-up vs1 costs of remote medical attention in patients with chronic heart failure.7
To conclude, with the preliminary results of this study it is possible to affirm that the remote follow-up of patients with heart failure allowed for a prompt attention from home, avoiding the emergency room visit for uncontrolled disease or complications; and it allowed for the saving of resources in the patient care in our hospital.
Ethical declarationThis study was approved by the Local Research and Ethics Committee No. 2602 of the Hospital de Especialidades No. 2, Unidad Médica de Alta Especialidad of the Instituto Mexicano del Seguro Social, in the Centro Médico Nacional del Noroeste in Obregón city, Sonora.
ContributorsPérez-Rodríguez, G contributed to the original idea, the study design, the results analysis and data interpretation, and to the writing and edition of the final article.
Brito-Zurita, OR contributed to the study design, results analysis and data interpretation, bibliography review, writing and editing of the final article.
Sistos-Navarrese, E contributed to the adjustment of the platform for the reception and sending of the data, training of the nurse for the interpretation of the signal in the platform, collection and assembly of the data, review and approval of the final writing.
Benítez-Aréchiga, ZM contributed to the recruitment of the patients, results analysis and data interpretation, writing and editing of the final article.
Sarmiento-Salazar, GL contributed to the recruitment of the patients, data interpretation and analysis, writing and editing of the final article.
Vargas-Lizárraga, JF contributed to the recruitment of the patients, results analysis and data interpretation, writing and editing of the final article.
All the authors read and approved the final manuscript.
Conflict of interestThe authors declare that there are no conflicts of interests of any nature in this research work.
To the Instituto Mexicano del Seguro Social for the technical, human, and financial support in the accomplishment of this study.
To the telephone company Alcatel-Lucent de México S A de C V for their technical support in the accomplishment of this work.
And very special thanks to Dr. José Manuel Ornelas Aguirre, for his observations, suggestions, and recommendations in the final writing of this study.
Please cite this article as: Pérez-Rodríguez G, Brito-Zurita OR, Sistos-Navarro E, Benítez-Aréchiga ZM, Sarmiento-Salazar GL, Vargas-Lizárraga JF. El seguimiento telemétrico disminuye la visita a la sala de urgencias y coste de atención en enfermos con insuficiencia cardíaca crónica. Cirugía y Cirujanos. 2015;83:279–285.