Coronary endarterectomy is a surgical procedure to remove atheroma plaques from the coronary arteries, with a worldwide incidence of between 3.7% and 42%. 10 years’ experience on this technique in our hospital is presented.
Materials and methodsA cross-sectional descriptive study was conducted by reviewing 486 clinical records of patients subjected to myocardial revascularisation with cardiopulmonary bypass, moderate hypothermia and ante grade cardioplegia, between January 2003 and June 2013. The risk factors included were: age, gender, left-ventricular-ejection-fraction, EuroSCORE, left main coronary disease, diabetes and systemic arterial hypertension, perioperative mortality, myocardial infarction, perioperative bleeding, surgery times, mediastinitis, sternal dehiscence, and days of hospital stay.
ResultsA total of 97 patients were included; 77 males (79.4%) and 20 females (20.6%), with a mean age of 62±8.9 years. 75.2% had arterial hypertension, 61.8% diabetes, and 46.3% both. There was left main coronary disease in 35%, and 18.5% in its equivalent (lesion >70% in anterior descending and circumflex), 58.5% with depressed left ventricular ejection, and 11.3% was related to failed intervention. The endarterectomy of a single artery was present in 75.2%, mainly to the descending artery, average aorta-coronary bridges 3, arterial left mammary graft, 96.9%, perioperative myocardial infarction 3.09%, reoperation for bleeding 5.15%, dehiscence 3.09%, and mediastinitis 2.06%. The mean stay in the Critical Unit was 4±6 days and in hospital room 5±5 days.
ConclusionsTo perform coronary endarterectomy increases the morbidity rate, as described in the international literature. Increased mortality was observed in patients with EuroSCORE of intermediate and high risk, which suggests reconsidering the use of this technique in these patients.
La endarterectomía coronaria es una intervención quirúrgica para remover las placas de ateroma que bloquean el recubrimiento interno de las arterias coronarias; su incidencia esta entre 3.7 y 42% a nivel mundial.
Material y métodosEstudio transversal, descriptivo. Se revisaron 486expedientes clínicos de pacientes sometidos a revascularización miocárdica con derivación cardiopulmonar, hipotermia moderada y cardioplejía sanguínea anterógrada, entre enero de 2003 a junio 2013, incluyendo factores de riesgo como: edad, género, fracción de eyección del ventrículo izquierdo, EuroSCORE, enfermedad del tronco coronario izquierdo, enfermedad trivascular, diabetes e hipertensión arterial sistémica, mortalidad perioperatoria, infarto del miocardio, sangrado perioperatorio, tiempos de cirugía, mediastinitis, dehiscencia esternal y estancia intrahospitalaria.
Resultados77hombres (79.4%) y 20mujeres (20.6%) con edad promedio 62±8.9. Se encontró hipertensión arterial en el 75.2%, diabetes en el 61.8% y 46.3% en ambos. La incidencia de enfermedad del tronco coronario izquierdo fue del 35% y su equivalente (lesión >70% en descendente anterior y circunfleja) del 18.5%, con fracción de eyección del ventrículo izquierdo deprimida (58.5%) y relacionado con intervencionismo fallido (11.3%). La endarterectomía a un solo vaso se presentó en el 75.2%, predominando la descendente anterior, promedio de puente aortocoronario 3, arteria mamaria izquierda en el 96.9%, infarto perioperatorio en el 3.09%, reintervención por sangrado en el 5.15%, dehiscencia en el 3.09%, mediastinitis en el 2.06%. Estancia en cuidados intensivos de 4±6 días, y en piso, de 5±5 días.
ConclusionesRealizar endarterectomía coronaria incrementa la morbilidad, como se describe en la bibliografía médica internacional. Observamos incremento en la mortalidad en pacientes con EuroSCORE intermedio y alto. Se sugiere reconsiderar su uso en este grupo de pacientes.
Cardiovascular diseases are still the major cause of death globally, as well as in Mexico, affecting mainly the older population, especially from the second half of the 20th1 century. Although ischaemic cardiopathy mortality in Mexico was one of the lowest in the decade of 1970, it had practically doubled 30 years later, surpassing the rate observed in countries like Argentina or Chile, whose rates were 3–4 times higher than those observed in Mexico in 1970.2
In Eastern European countries, an increase in the mortality caused by ischaemic cardiopathy was observed in the last 35 years of the 20th century,3 in contrast to the United States, where a significant reduction in the ischaemic cardiopathy mortality was observed during the same period (up to 64%).4
It is evident that developing countries are experiencing an emergent epidemic in mortality caused by ischaemic cardiopathy.5 At the Instituto Mexicano del Seguro Social, the largest social security institution in the country, covering almost half the Mexican population, ischaemic cardiopathy is the second most important cause of healthy life years (HLY) lost, due both to the premature mortality it causes and to the years of life with disabilities it generates.6
According to Mueller et al.7 the coronary endarterectomy developed in the initial phases of the myocardial revascularisation history was first described by Charles Bailey on October 29, 1956, in the Hahnemann Hospital, Philadelphia. He was the first to report the use of a technique for distal and blind closed endarterectomy without performing cardiopulmonary bypass in myocardial revascularisation surgery. In 1956, Absalón also conducted endarterectomies in addition to end-to-lateral or end-to-end arterial grafts (using the carotid, subclavia or internal mammary arteries with or without Ivalon prosthesis).7 The publications and advances in vascular techniques described by Alexis Carrel,8 winner of the Nobel Prize for Medicine, allowed for the anastomosis between grafts.8 In 1958, Senning described the endarterectomy through direct incision on the plaque, reconstructing with an arterial mammary graft. In 1965, Vineberg and Diethrich utilised omentum, pedicled arteries and veins, muscle, pleura and fascias grafts. That same year, Donald Effler, of the Cleveland Clinic, reported a modification to the Senning procedure,9 repairing the open endarterectomy utilising pericardial patch instead of mammary or saphenous vein grafts. This technique was implemented after, on one occasion, the venous graft fell to the ground.
Kolesov and Potashov10 indicated that Carther and Roth described open endarterectomy in dogs; and, Longmire et al.11 reported an anterograde procedure of open endarterectomy in humans without using cardiopulmonary bypass, this being the Vineberg procedure, the most popular technique of revascularisation.10,11 Today it is rarely practiced, and there is no registry about incidence or evolution in our country. The figures are supported by reports in the international medical bibliography, which presents an incidence ranging from 3.7 to 42% of myocardial revascularisation surgeries with cardiopulmonary bypass.12
Angiography showing the permeability in this type of patient 36 months later varies according to the type of graft utilised for the reconstruction: with internal mammary artery the permeability is 89.1%, versus 81% with reversed saphenous vein.13,14 There is an association between occluded stents of early presentation – around 5 months – with a longer span of endarterectomy and an increase in the preoperative infarction of 10%. This is the reason that, in these cases, a strict anticoagulation of at least six months is recommended.15 In the association between endarterectomy and the off-pump surgery, the most frequently treated artery is the right coronary artery; postoperative bleeding reported is 1.4%, and perioperative infarction is 4.3% versus 0.8% in patients who did not undergo endarterectomy. Also, early mortality at day 30 is 2.85% versus 1.3% in non-endarterectomised patients, and 10-year life expectancy is 78%.16 Mortality ranges from 2 to 8.6%, while 5-year life expectancy goes from 70 to 75%.
The topographic place in the coronary tree used for endarterectomy is also related to certain morbidity and mortality, the descending anterior being one of the most important; although, the prevalence rate of the left main coronary disease is 8.2%.17 In patients with ejection fraction lower than 35%, surgery has better outcomes.18 However, when a long endarterectomy is performed (>4cm), and reconstruction with the internal mammary artery is made, the mortality,19 surgical time, postoperative bleeding,20 and perioperative myocardial infarction increase; the 5-year life expectancy is 92%21 and the period free of cardiac events is up to 88.1%.22
Indications for it have not been well defined yet, as they depend on the patient, the angiocardiography, the perioperative findings, the intermediate size of the vessel, of 1mm in angiogram, or if it irrigates a viable area of the myocardium or causes angina. The most commonly used techniques are divided into closed endarterectomy (single or multiple) and open (reconstruction with the patching of the vein or with internal mammary artery); the method of choice will depend on the experience the surgeon has and on the presentation of the injured vessel.23
To assure early permeability, some authors use anticoagulation regimes, and once the major bleeding is over, they start in the intensive care unit with doses of acetylsalicylic acid 100mg/day, heparin, as well as with warfarin to maintain INR near 2.13.24
It is important to consider that the scarring itself and the fibrosis deposit and proliferation of myofibroblasts of the grafts25 may affect the permeability to some degree; nevertheless, the invasive nature of the studies limit follow-up, and for this reason the new techniques, whether imaging with reconstruction or virtual angioscopy, will allow closer follow-up scenario.26
It is important to know the postoperative evolution after coronary endarterectomy in myocardial revascularisation surgery, since we considered it has an impact in the resulting morbidity and mortality, being increasingly applied according to the evolution of the coronary disease.
Materials and methodsA cross-sectional, retrospective and observational study was conducted in the Department of Cardiothoracic Surgery of the Unidad Médica de Alta Especialidad (UMAE), Hospital de Cardiología No. 34, by reviewing 468 clinical records of patients with advanced coronary disease subjected to myocardial revascularisation with coronary endarterectomy in the period between 1 January, 2003 and 30 June, 2013.
Inclusion criteriaPatients of both genders, over the age of 18, subjected to myocardial revascularisation with closed coronary endarterectomy. With cardiopulmonary bypass, subjected to intermediate hypothermia (33°C) and antegrade cardioplegia.
Exclusion criteriaPatients submitted to revascularisation without endarterectomy, open endarterectomy, or submitted to off-pump surgery, normothermia, continuous delivery of cardioplegia, incomplete clinical records, or valve surgery.
All the patients who met all these inclusion criteria during the period of the study were included. The sample was a non-probabilistic sampling of consecutive cases.
A descriptive statistic was performed of the studied population through measures of central tendency and dispersion and according to the type of distribution of each variable, by means of SPSS statistics v19. Because this was a retrospective study and data was only collected from clinical records, no intentional interventions or modifications were made in the physiological, psychological and social variables of the studied subjects. Patients were given an informed consent form.
ResultsAll 468 records of patients submitted to myocardial revascularisation during the period 1 January, 2003 and 30 June, 2013 were reviewed. Of these, a total of 97 patients were subjected to closed coronary endarterectomy, which means a frequency of 20.7% in this procedure.
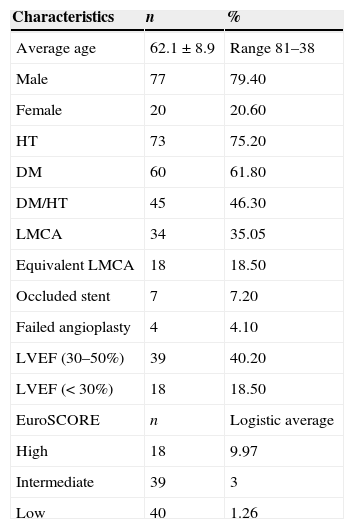
Patients were distributed in 77 males (79.4%) and 20 females (20.6%), with an average age of 62.1±8.9 years, with a lower age limit of 38 years and a maximum age of 81 years.
Among the comorbidities, 75.2% of the patients presented arterial hypertension, 61.8%, diabetes mellitus, and 46.3% a combination of both. The left main coronary artery disease was detected in 35.05%, and its equivalent left main coronary artery disease in 18.5%. Patients with depressed left ventricular ejection, 40.2%, and almost half of the patients (18.5%) presented an ejection fraction lower than 30%.
The surgical risk was calculated through EuroSCORE, being low in 41.2% of the patients (1.2% probability of mortality), intermediate in 40.2% (3% probability of mortality) and a high risk in 18.6% (9.9% probability of mortality) of the cases.
The 11.3% was related to failed percutaneous intervention (occluded stent, 7.2%; failed angioplasty, 4.1%) (Table 1).
Characteristics of the population with myocardial revascularisation through coronary endarterectomy (n=97).
| Characteristics | n | % |
|---|---|---|
| Average age | 62.1±8.9 | Range 81–38 |
| Male | 77 | 79.40 |
| Female | 20 | 20.60 |
| HT | 73 | 75.20 |
| DM | 60 | 61.80 |
| DM/HT | 45 | 46.30 |
| LMCA | 34 | 35.05 |
| Equivalent LMCA | 18 | 18.50 |
| Occluded stent | 7 | 7.20 |
| Failed angioplasty | 4 | 4.10 |
| LVEF (30–50%) | 39 | 40.20 |
| LVEF (<30%) | 18 | 18.50 |
| EuroSCORE | n | Logistic average |
| High | 18 | 9.97 |
| Intermediate | 39 | 3 |
| Low | 40 | 1.26 |
DM: Diabetes mellitus; LVEF: Left ventricular ejection fraction; HT: Arterial hypertension; LMCA: Left main coronary artery.
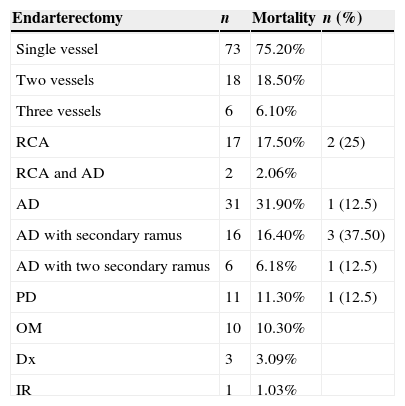
In 75.2% of the cases the endarterectomy was performed on a single vessel, followed by 18.5% in two, and 6.1% in three vessels. The predominant single artery treated was the anterior descending artery, representing 31.9%, followed by the right coronary artery, 17.5%; the combination of the anterior descending with a secondary branch, 16.4%; and the posterior descending, 11.3% (Table 2).
Distribution of endarterectomy and associated mortality (n=97).
| Endarterectomy | n | Mortality | n (%) |
|---|---|---|---|
| Single vessel | 73 | 75.20% | |
| Two vessels | 18 | 18.50% | |
| Three vessels | 6 | 6.10% | |
| RCA | 17 | 17.50% | 2 (25) |
| RCA and AD | 2 | 2.06% | |
| AD | 31 | 31.90% | 1 (12.5) |
| AD with secondary ramus | 16 | 16.40% | 3 (37.50) |
| AD with two secondary ramus | 6 | 6.18% | 1 (12.5) |
| PD | 11 | 11.30% | 1 (12.5) |
| OM | 10 | 10.30% | |
| Dx | 3 | 3.09% | |
| IR | 1 | 1.03% |
RCA: Right coronary artery; AD: Anterior descending; PD: Posterior descending; Dx: Diagonal; OM: Obtuse marginal; IR: Intermediate ramus.
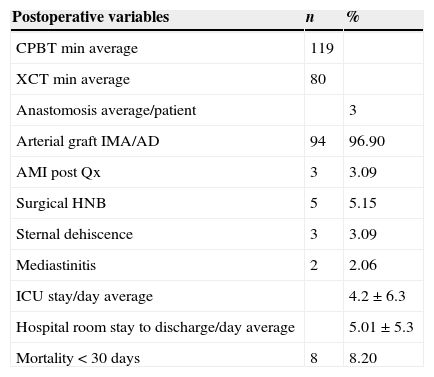
Average aorta–coronary bridges of the 292 coronary anastomosis registered was 3 bridges in each surgery. 96.9% of the patients received an internal mammary artery graft. The average time of the cardiopulmonary bypass duration was 119min, and the aortic clamping intervention, 80min (Table 3).
Postoperative findings in population with myocardial revascularisation through coronary endarterectomy (n=97).
| Postoperative variables | n | % |
|---|---|---|
| CPBT min average | 119 | |
| XCT min average | 80 | |
| Anastomosis average/patient | 3 | |
| Arterial graft IMA/AD | 94 | 96.90 |
| AMI post Qx | 3 | 3.09 |
| Surgical HNB | 5 | 5.15 |
| Sternal dehiscence | 3 | 3.09 |
| Mediastinitis | 2 | 2.06 |
| ICU stay/day average | 4.2±6.3 | |
| Hospital room stay to discharge/day average | 5.01±5.3 | |
| Mortality <30 days | 8 | 8.20 |
IMA: Internal mammary artery; AD: Anterior descending; AMI: Acute myocardial infarction; HNB: Higher-than-normal bleeding; CPBT: Cardiopulmonary bypass time; XCT: Aortic cross-clamping time; ICU: Intensive care unit.
Among the complications, we found 3.09% of the patients presented acute myocardial infarction, and 2/3 of the cases died due to associated cardiogenic shock. Reoperation for higher-than-normal bleeding was performed in 5.15%. Two-fifths of the patients died.
Enteral dehiscence was observed in 3.09% and mediastinitis in the 2.06%, with one case of death due to sepsis (Table 3).
The mean stay in the postoperative care unit was 4.2±6.3 days (maximum 55 days), and 5.01±5.3 days in a hospital room; and mortality at <30 days was 8 patients (8.2%).
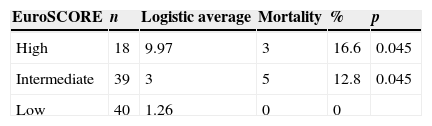
Causes of mortality were: higher-than-normal bleeding (25%), acute myocardial infarction (25%), sepsis (12.5%), cardiogenic shock (non-acute myocardial infarction) (25%) and anaphylactic shock (12.5%), statistically significant in patients with EuroSCORE of intermediate and high risk (p=0.045) (Table 4).
DiscussionMyocardial revascularisation surgery is one of the procedures most frequently performed in our hospital. Today, it is common to find more complex cases, not only because they present a higher number of comorbidities, but also because the coronary structures are in a worse condition. Many patients are subjected to atheroma plaque extraction with no choice, or an artery is inadvertently opened in a coronary bed where the disease is worse than expected, or it is not possible to find a healthy site with healthy walls to perform the arteriotomy, or a technique has been conducted in a place where the disease is widely spread. The surgeon must be resourceful and have experience in these scenarios.
Our hospital, Unidad Médica de Alta Especialidad 34, takes care of patients from seven states in Northeast Mexico, with an annual surgical average of more than 900 procedures, of which, 65% (585) are myocardial revascularisation surgery involving the conducting of a wide variety of techniques: on-pump and off-pump techniques, and, although controversial, the performance of endarterectomy. Careaga et al.27 indicate that, just as Charles Bailey had described it in 1957, the myocardial revascularisation surgery continues to be the most frequent surgical procedure in our institution.
In Mexico, this procedure has hardly been reported, which makes it difficult to choose whether or not to perform coronary endarterectomy. In this group, it was performed with a frequency of 20.7% within the previously described ranges, males being predominantly more affected, as has been reported by the medical bibliography.1
The most commonly used technique for the removal of coronary plaque was the closed one, which is the recommended technique for the right coronary and the circumflex arteries. This technique exposes the intima and there is the risk of obtaining incomplete plaques, which is associated with an early mortality of 7% in contrast with the 3% of the open technique. The result found in our review was an early mortality of 8.2%, similar to that described in the medical bibliography.28
On the other hand, there are reports stating that closed endarterectomy is linked to complications, and that it has a three-dimensional configuration in the branches of the anterior descending artery (diagonal and septal).10 We observed mortality in the group submitted to endarterectomy of the anterior descending artery. Although isolated cases of patients younger than 40 years are observed, in our study the age group mainly affected with ischaemic cardiopathy is the group over the age of 60 years.
At the national level, there are reports of the association of cardiovascular diseases with diabetes and arterial hypertension in the Mexican population27; which, according to the Federación Mexicana de Diabetes, are chronic degenerative diseases and risk factors for death in our country. Half of the deaths associated appear in patients younger than 70 years. The incidence in our study was 75.2% and 61.8% for arterial hypertension and diabetes mellitus, respectively; also, almost half of the patients presented both diseases, which has great impact on morbidity and mortality.29
The risk of sudden death increases in patients with left main coronary disease associated, which is reported in the medical bibliography in more than 50%.18 In our population, this risk represented about half (53.8%), with affection of the left main coronary artery or equivalent.
The 58.8% of the patients presented depressed ejection-fraction; however, it has been demonstrated that the surgical treatment reduces the mortality, in comparison with the medical treatment, in this group of patients.19
Operative risk was calculated with the EuroSCORE I, 41.2% of the population being defined as “low-risk” group, with a probability of mortality of 1.26%, without cases of death in this group. For the “intermediate-risk” group, the average value of probability of mortality was 3%; and for the “high-risk” group, the average value of risk was 9.97%.
According to EuroSCORE, mortality was associated with the intermediate-risk group (n=39); the deaths represented 12.8%, practically 4 times more than what was calculated (3%). The same is observed in the high-risk group (n=18), with 3 deaths (16.6%), which is almost double of the value calculated (9.97%).
The type of coronary endarterectomy most frequently practised was single-vessel endarterectomy, mainly involving the descending artery; however, performing the closed endarterectomy in this artery bed may be associated with complications and morbidity and mortality increase. The placement of optimal graft can be considered, since the 96.9% of the patients received an arterial left mammary graft to the left descending artery, which is the gold standard. Also, an average of three aorta-coronary bridges was performed per patient.
The average times of bypass and of clamping were maintained, as, in contrast with open coronary endarterectomy, they take more time to reconstruct.28
Perioperative acute myocardial infarction was presented in 3.09% of the cases, similar to the 4.6% reported in the medical bibliography, in contrast to conventional surgery without coronary endarterectomy, where it ranges from 2 to 19.1%. Reoperation for bleeding was 5.1%, whereas in the medical bibliography reports it goes up to 6%10; and in conventional surgery without coronary endarterectomy, 1–3% of the cases will require reoperation for bleeding.29 No increase in the dehiscence (3.09%) or mediastinitis (2.06%) was observed, compared with the average risk of 1.4–3.1% described in conventional myocardial revascularisation.30
Moreover, no long stay in postoperative care unit or hospital room was observed (between 4 and 5 days, respectively). The early mortality of this group was 8.2%, in contrast with 6.8 and 8.5% reported in some publications.
ConclusionsIn this study, we followed for 10 years the evolution of patients submitted to myocardial revascularisation with coronary endarterectomy. Throughout the time, surgeons have been facing more complex cases, together with the rise of the percutaneous and medical treatments, the patient arrives for surgery in advanced stages, a great percentage of them presenting comorbidities, which have a significant impact in the outcomes.
Coronary endarterectomy is associated with higher morbidity and mortality; however, in our experience the incidence of morbidity and mortality is similar to those reported in medical literature, even if in our study the artery mainly treated was the anterior descending artery, which is not recommended as it increases morbidity and mortality. It is recommended not to practise closed endarterectomy in the descending artery.
Poor outcomes have been observed in patients who had intermediate and high EuroSCORE, with morbidity and mortality higher than two to three times the percentage of risk calculated. For this reason, it is recommended that the benefits of this practice in this group of patients be reconsidered. In spite of this, coronary endarterectomy has increasingly been performed in accordance with the present evolution of the coronary disease. As a tool, it is still controversial and is not recommended as routine management of patients with the coronary bed in a poor state.
Conflict of interestThe authors declare that there are no conflicts of interest.
Please cite this article as: Bernal-Aragón R, Sáenz-Rodríguez R, Orozco-Hernández E, Guzmán-Delgado N, Aragón-Manjarrez R, Hernández-Alvídrez A. Experiencia de la endarterectomía coronaria en cirugía de revascularización miocárdica. Cir Cir. 2015;83:273–278.