Adamantinoma is a rare lesion of low-grade malignancy, and represents 1% of malignant bone tumours of bones, and is mainly located in two regions of the body, jaw (ameloblastoma), and lower extremities. The treatment of choice is surgery due to it being a radio- and chemotherapy-resistant neoplasia.
Clinical caseA 39-year-old male with a history of neonatal hydrocephalus with moderate psychomotor retardation. He began with pain in the posterior region of the left thigh for one year before admission, which was managed as posterior radicular syndrome. He had sudden intense pain on walking that led him to fall over. In the examination, left pelvic limb with deformity in the distal third with increase in volume in the thigh, with pain to palpation, and presence of crackles in the distal third of the femur were observed. A biopsy of the thigh was performed, with subsequent local wide excision+replacement of bone with cadaver bone and a central medullary nail. The final diagnosis was adamantinoma of femur.
ConclusionAdamantinomas are rare tumours. It is important to recognise this type of tumour from the beginning, since its prognosis is excellent in initial stages. It is important to have free margins as survival is very high.
El adamantinoma es una rara lesión de bajo grado de malignidad, representa <1% de los tumores malignos de huesos, se localiza principalmente en 2 regiones del cuerpo, la mandíbula (ameloblastoma) y las extremidades inferiores. El tratamiento de elección es la cirugía ya que se trata de una neoplasia resistente a la radioterapia y quimioterapia.
Caso clínicoPaciente masculino de 39 años de edad con antecedente de hidrocefalia neonatal con retraso psicomotor moderado. Un año previo a su ingreso comenzó con dolor en región posterior del muslo izquierdo, el cual se manejó como síndrome radicular; posteriormente presentó dolor súbito intenso a la deambulación, por lo que tuvo caída de su propia altura. A la exploración de miembro pélvico izquierdo con deformidad en el tercio distal con aumento de volumen en el muslo, dolor a la palpación y presencia de crepitación en tercio distal de fémur. Se le realizó biopsia en muslo, posterior escisión local amplia+colocación de hueso de cadáver con clavo centromedular con reporte definitivo de adamantinoma de fémur.
ConclusiónLos adamantinomas son tumores raros y es importante reconocer este tipo de tumores desde un inicio, ya que su pronóstico es excelente en etapas iniciales. Es importante tener bordes libres ya que la supervivencia es muy alta.
Primary bone tumours are neoplasias that represent less than 0.2% of all malignant tumours. The most common ones are osteosarcoma (35%), chondrosarcoma (30%) and Ewing's sarcoma (16%); adamantinoma only occurs in <1%.1 The first case reported is attributed to Maier in the year 1900.2 In 1913, Fisher reported the first tibia adamantinoma.3
The origin of this disease is currently unknown. However, there are various hypotheses. Fisher proposed a congenital implantation of epithelial cells3; Ryrie,4 Dockerty and Meyerding5 are in favour of a traumatic implantation; Lederer and Sinclair,6 Naji et al.7 propose a synovial origin. Currently, the theory that states that this disease has an epithelial origin is a subject of debate; during the development of the embryo the basal epithelium shifts, which supports this since the most frequent place is the anterior part of the tibia where there is proximity to the skin.8 Among the revised cases by Moon and Mori, 60% of 200 cases had a history of trauma in the tumour area.9
Clinical caseA 39-year-old male patient with relevant medical history; his mother died of breast cancer. He suffered from neonatal hydrocephalia with moderate psychomotor retardation. The onset of the disease was a year before admission, with pain in the posterior part of his left thigh. It was treated by multiple doctors as radicular syndrome with mild pain improvement. He attended the casualty department due to sudden intense pain during ambulation with no lesion mechanism, causing him to fall from standing height with limb deformity and reduced mobility. During physical examination, a deformity in his left pelvic limb could be observed, located at the distal third of his thigh. There was volume augmentation, pain on palpation on femoral diaphysis and crepitation on the distal third of the femur. Sensitivity was conserved and pulses present were not compromised. Chest X-ray showed no alterations. Anteroposterior and lateral femur X-rays: with cross-sectional breaks in continuity at the distal third of the femur, in pathological area, due to the presence of a radiolucent, medullar, expansive, monostotic lesion of 70mm×45mm. There was periosteal reaction and the transition area was short (Fig. 1).
Anteroposterior and lateral femur X-rays that evidence cross-sectional breaks in continuity at the distal third of the femur, in the pathological area, due to the presence of a radiolucent, medullar, expansive, monostotic lesion of 70mm×45mm. There is periosteal reaction and the transition area is short.
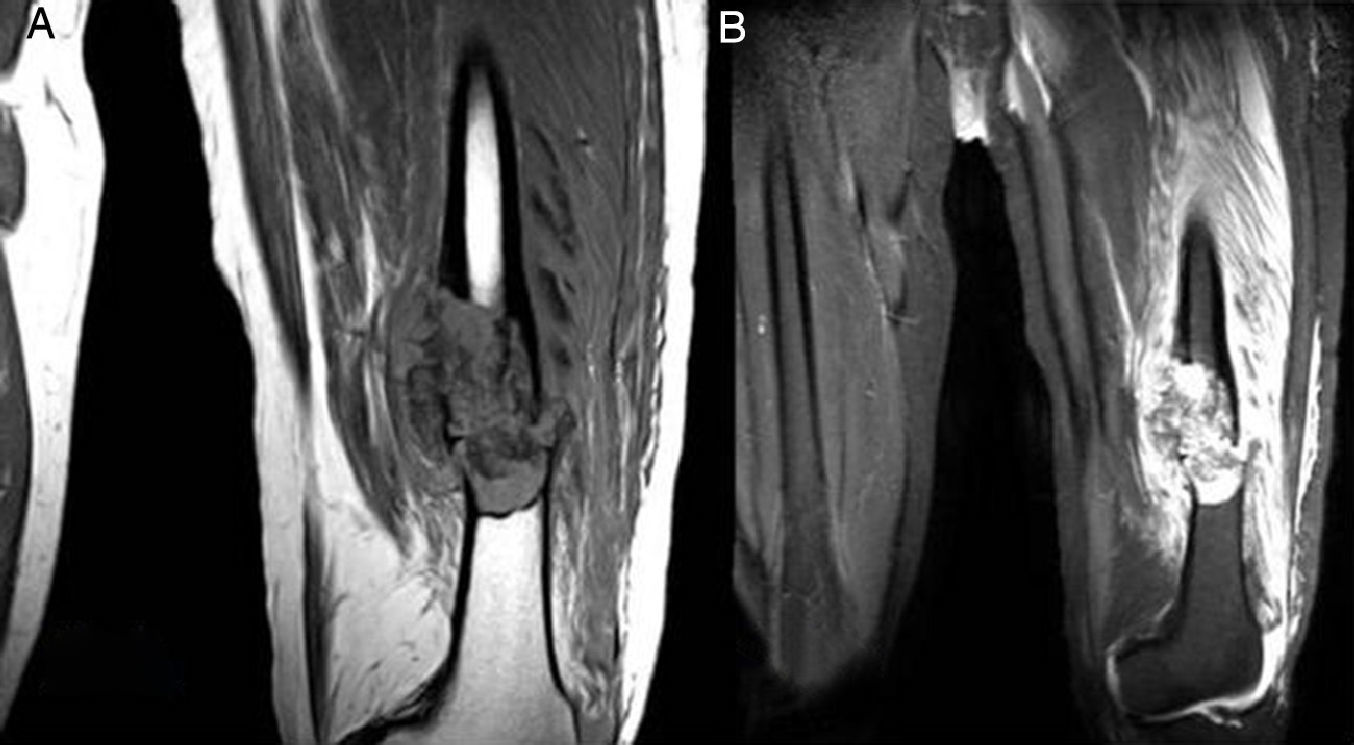
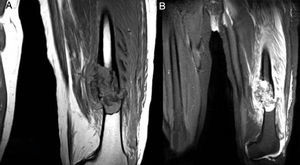
Medullar lesion in the intersection of the medial third and the distal third of the left femur that was associated with multifragmentary fracture over the pathological area in a neoplastic lesion, without being able to rule out a bone cyst or another pathological process diagnosis (Fig. 2A and B).
Magnetic resonance of the femur. Medullar lesion in the intersection of the medial third and the distal third of the left femur that was associated with multifragmentary fracture over pathological area in a neoplastic lesion without being able to rule out a bone cyst or another disease diagnosis.
A trucut-type biopsy of the lesion was performed, from which the histopathological diagnosis corresponded to an adamantinoma, the reason why a R0 wide local excision was made in the left femoral diaphysis with open reduction and fixation of the pathological fracture in the left femur with an unreamed femoral nail (UFN) and the placement of cadaveric bone grafting. Fig. 3 shows the final reconstruction of the limb with an anteroposterior plate in the left thigh where data related to osteotomies can be observed; there is osteosynthesis in the left femur with centromedular nail and three antirotation screws.
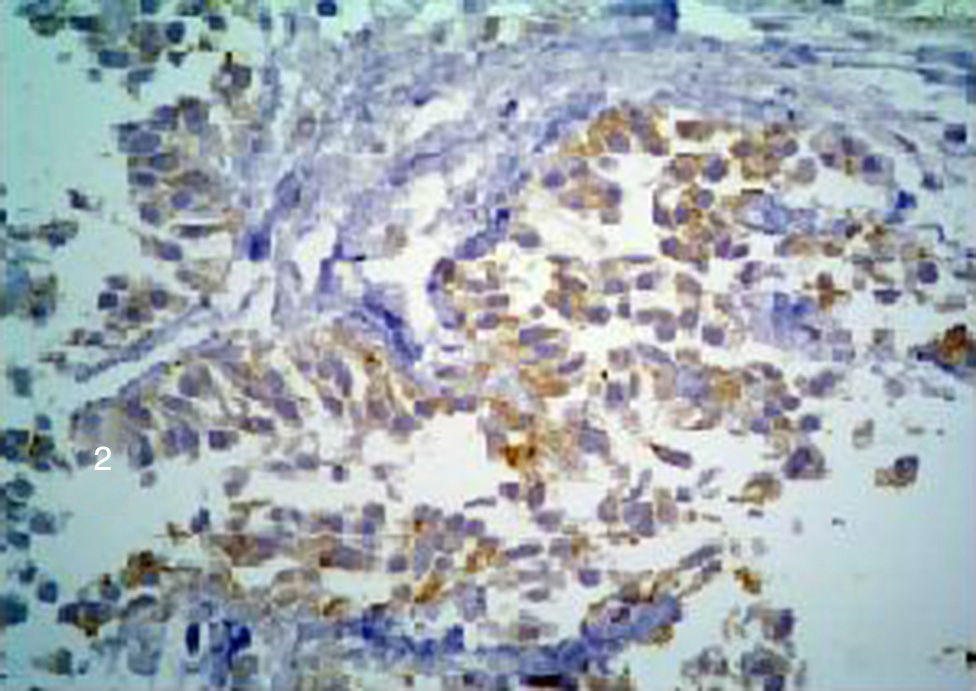
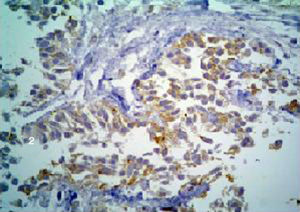
Pathological anatomyThe medial and distal third of the femur was amputated. There was a 6cm tumour in the medial section at the long axis, with ill-defined infiltrating borders (Fig. 4). Histologically, the neoplasia was biphasic, with solid areas, of which cells had an epithelioid aspect and basaloid pattern; nuclei were ovoid and comprised of finely granular chromatin; the cytoplasm was wide, eosinophilic and clear in some areas. Immunostaining demonstrated expression of the mixture of keratins and cytokeratins 5/6 (Fig. 5). There were other areas of osteofibrous aspect and nests of basaloid cells caught between them. Therefore, in the TNM pathological classification for bone cancer, this tumour is classified as T1 N0 M0 G1, clinical stage IA.
Primary bone malignant tumours are infrequent and only comprise 0.2% of all primary malignant tumours and 5% of malignant paediatric tumours. The predominance of primary bone malignant tumours is estimated at 8 in every 1,000,000 persons, with 2500 new cases diagnosed per year in the United States.10 Adamantinoma represents <1% of all bone malignant tumours.1 Clinical presentation of these tumours occurs during the second and fifth decades of life, average age between 25 and 35 years. They rarely occur during infancy; only 3% of the cases involve children under the age of 10.11 There is a male/female ratio of 5:4.9
There is a predilection for long bones: in 80% of the cases they are located at the tibial diaphysis, and with less frequency at the fibula, humerus or in the bones of hands or feet, and it involves the tibia and the fibula simultaneously in only 10% of the cases.10,11 In their initial stage they are located at the affected bone's cortex and they can be asymptomatic or have a very slight symptomatology, while during the advanced stage they affect the perilesional soft tissue and the bone marrow, and symptoms such as pain and limb deformity increase.
Since it is a slow-growing tumour, metastases are not that frequent and they are present in 20% of the patients at the time of diagnosis; the most frequent locations are the lungs, other bones and the lymphatic system.10
Imaging departmentX-rays show an osteolytic image, well delimitated, comprised of one or several cysts, which can extend longitudinally in the cortex or destroy it, spreading to the bone marrow. There can be a periosteal or soft tissue reaction. There can also be a multifocal reaction in the same bone or in other bones. Differential diagnosis with fibrous dysplasia and osteofibrous dysplasia is important, the first being common in younger patients.10
Magnetic resonance shows low density in T1, while there is a high level of capture in T2.12
From a histological point of view, adamantinoma is a biphasic tumour with epithelial characteristics and osteofibrous components.12 It is classified into two types: Classic adamantinoma usually appears in patients over the age of 20. Histologically, it has an epithelial and osteofibrous component and is a more aggressive tumour.12Differentiated adamantinoma (juvenile intracortical, osteofibrous dysplasia-like). This appears in younger patients. Histologically, it appears as masses of epithelial cells. Its evolution is more benign.12
Neoplastic cells vary from small to large, located in an osteofibrous matrix content. There are several histological variants13: tubular, basaloid, flaky, fusiform and osteofibrous dysplasia-like. Calcification areas, giant cells and foamy histiocytes are frequent. Epithelial cells express cytokeratins, particularly cytokeratin 7, 5/6, 14, 17 and 19.
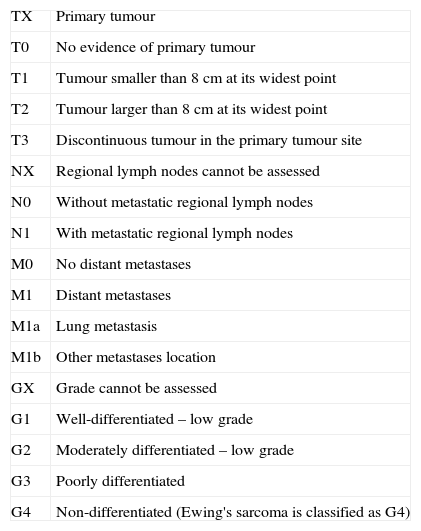
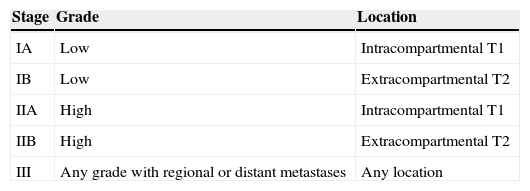
Since bone tumours are handled differently according to their histology, it is essential to do a biopsy, which must always be performed by the surgeon who will be in charge of the final treatment of the disease. Differential diagnosis is mainly performed in osteofibrous dysplasias, which occurs in patients under the age of 10. It is a disease with benign characteristics and the presentation place involves both the tibia and the fibula. It can regress spontaneously in puberty in up to 33% of the cases.12 Other differential diagnoses are: fibrous dysplasias, chondromyxoid fibromas, chondrosarcomas, osteomyelitis, eosinophilic granulomas, giant-cell tumours, epithelial metastases and angiosarcomas.12 Bone tumours are classified according to the TNM system (Tables 1 and 2) and according to the Enneking system (Table 3).
2009 TNM classification.
| TX | Primary tumour |
| T0 | No evidence of primary tumour |
| T1 | Tumour smaller than 8cm at its widest point |
| T2 | Tumour larger than 8cm at its widest point |
| T3 | Discontinuous tumour in the primary tumour site |
| NX | Regional lymph nodes cannot be assessed |
| N0 | Without metastatic regional lymph nodes |
| N1 | With metastatic regional lymph nodes |
| M0 | No distant metastases |
| M1 | Distant metastases |
| M1a | Lung metastasis |
| M1b | Other metastases location |
| GX | Grade cannot be assessed |
| G1 | Well-differentiated – low grade |
| G2 | Moderately differentiated – low grade |
| G3 | Poorly differentiated |
| G4 | Non-differentiated (Ewing's sarcoma is classified as G4) |
G: histological grade; M: metastasis; N: ganglia; T: tumour.
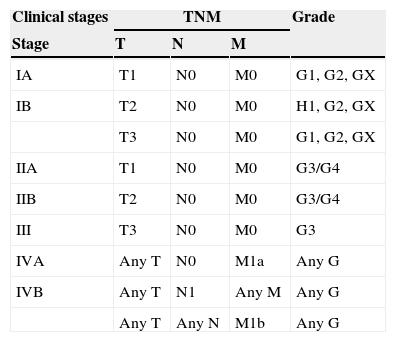
Clinical stages.
| Clinical stages | TNM | Grade | ||
|---|---|---|---|---|
| Stage | T | N | M | |
| IA | T1 | N0 | M0 | G1, G2, GX |
| IB | T2 | N0 | M0 | H1, G2, GX |
| T3 | N0 | M0 | G1, G2, GX | |
| IIA | T1 | N0 | M0 | G3/G4 |
| IIB | T2 | N0 | M0 | G3/G4 |
| III | T3 | N0 | M0 | G3 |
| IVA | Any T | N0 | M1a | Any G |
| IVB | Any T | N1 | Any M | Any G |
| Any T | Any N | M1b | Any G | |
G: histological grade; M: metastasis; N: ganglia; T: tumour.
These are slow-growing tumours and if they have adequate margins their potential to present local recurrences or metastases is limited.
The marginal resection of these tumours has a local recurrence of up to 32%.
En-bloc resection: with this type of intervention there should be no local recurrences. Amputation: this should only be performed in cases where the neurovascular bundle is compromised, if there is vast invasion of soft tissues, cutaneous compromise or recurrences.12
Radiotherapy: Since adamantinomas are low-grade lesions with an extremely low mitotic index, they are radioresistant lesions.
The use of chemotherapy for this disease has not proven to be effective.
PrognosisAs in every oncological pathological process, the prognosis will depend on the clinical stage in which the patient is before treatment. In a revision by Qureshi et al.14 in which a tumour-free border resection was performed in 70 patients, an overall survival rate of 87.2% was reported after 10 years.
ConclusionAdamantinomas are infrequent tumours and it is important to recognise these types of tumours from the beginning, since their prognosis is excellent during early stages. It is important to always do a biopsy that confirms the diagnosis and have full surgical equipment that includes a surgical oncologist and an orthopaedic surgeon to be able to obtain adequate free borders, since survival is very high. A proper reconstruction that ensures adequate mobility and functioning of the affected limb is required.
Conflict of interestThe authors declare that there are no conflicts of interest.
Please cite this article as: Carrera-Muiños A, Díaz-González C, Monges-Jones JE, Carballo-Zarate A, Colin-Carrasco J. Tratamiento de adamantinoma de fémur con preservación de extremidad. Reporte de un caso y revisión de la literatura. Cir Cir. 2015;83:249–54.