Hypoparathyroidism is one of the most frequent complications of neck surgery. The treatment is currently medical; however this involves several complications secondary to high doses of calcium and vitamin D, thus making parathyroid allotransplantation a good management option.
Material and methodsPatients with hypoparathyroidism were selected in the April-December period of 2011 in the general surgical clinic. They were between 16 and 65 years, and ingested high doses of calcium. The donors were patients with primary and secondary hyperparathyroidism, and the transplants were performed in relation to blood group and human leucocyte antigen.
ResultsFive parathyroid allografts were performed. All the patients had iatrogenic hypoparathyroidism, all women with a mean age of 49.8 years. The graft was implanted under local anaesthesia in the non-dominant forearm. Four of the patients are so far considered functional due to the increase in paratohormone, and demonstrating its function by scintigraphy with sestamibi. One of the patients showed no increase in paratohormone or imaging studies that demonstrate its functionality. After a two year follow-up the graft remains functional but with oral calcium intake at a lower dose than before transplantation. None of the patients had immunosuppression side effects.
ConclusionsIn this study, allogeneic unrelated living parathyroid transplant with an immunosuppressive regimen of six months has proven to be a safe alternative treatment to improve quality of life by decreasing the excessive calcium intake and improving physical activity with adequate graft survival at 24 months follow-up.
El hipoparatiroidismo es una complicación frecuente de la cirugía de cuello. Actualmente el tratamiento es médico, y conlleva complicaciones secundarias a altas dosis de calcio y vitamina D, por lo que el alotrasplante es una opción de manejo.
Material y métodosSeleccionamos pacientes con hipoparatiroidismo en el periodo abril-diciembre de 2011 de la consulta de Cirugía General, de entre 16 y 65 años, que ingirieran dosis altas de calcio. Los donantes fueron pacientes con hiperparatiroidismo primario y secundario; los trasplantes se realizaron en relación con grupo sanguíneo y antígeno leucocitario humano.
ResultadosSe realizaron 5 alotrasplantes de paratiroides, en pacientes con antecedente de hipoparatiroidismo iatrogénico, mujeres con una edad promedio de 49.8 años; al tener el injerto bajo anestesia local se implanta en el antebrazo no dominante. De los trasplantes realizados 4 se consideran funcionales por elevación de paratohormona y se ha demostrado su función mediante gammagrama sestamibi. Una de las pacientes no mostró aumento de paratohormona ni los estudios de imagen demostraron la funcionalidad del injerto. A 2 años de seguimiento se mantienen con el injerto funcional, pero aún con ingesta de calcio oral aunque a más bajas dosis que antes del trasplante. Ninguna de las pacientes tuvo efectos secundarios a la inmunosupresión.
ConclusionesEl alotrasplante de paratiroides de vivo no relacionado con esquema de inmunosupresión ha demostrado ser un tratamiento alternativo seguro, para mejorar la calidad de vida al disminuir la ingesta excesiva de calcio y mejorar la actividad física de los pacientes, con sobrevida del injerto a 24 meses de seguimiento.
Hypoparathyroidism is one of the most common complications in neck surgery (thyroid glands, parathyroid glands, etc.); its incidence is associated with the type of disease or surgical technique used, as well as with the surgeon's experience. It is estimated that 10% of the patients who undergo surgery due to thyroid carcinoma will develop hypoparathyroidism.1
Nowadays, the only treatment for hypoparathyroidism is calcium and vitamin D supplements, which for a lack of negative feedback is frequently associated with overdoses or insufficient doses, leading to either hypo- or hypercalcaemia complications. With the purpose of avoiding complications associated with medical treatment, several surgical techniques have been attempted, such as the autotransplantation of fragments of parathyroid tissue. However, many times it is not possible to have parathyroid tissue for this procedure.
In 1971, Wells et al. performed a living-related donor allotransplantation, removing two parathyroid glands and implanting them in his/her son, who had previously received a renal transplantation. After a 30-month follow-up, endocrine activity was found in this implant.2 Since then, there have been several reports about parathyroid allotransplantations with diverse results.3–5 However, this procedure requires immunosuppression, which involves some well-known side effects.
One of the main issues related to allotransplantations is implant rejection, and implant survival and functionality will only be possible when the tissue is devoid of antigenic cells that strongly express human leucocyte antigen (HLA) class II. Parathyroid cells weakly express HLA class I antigens, which are not responsible for the rejection reaction, so this type of tissue generates a low incidence rate of rejection.6
We present the clinical results of five patients who received parathyroid allotransplantation due to postsurgical hypoparathyroidism after a one-year follow-up.
Material and methodsSelection of donorsPatients between the age of 10 and 65 who had primary or secondary hyperparathyroidism; not related to the recipients. Serological testing for hepatitis B virus, hepatitis C virus, human immunodeficiency virus, cytomegalovirus IgG and IgM antibodies, Epstein–Barr and purified protein derivative, as well as HLA, blood group and Rh factor was performed in all potential donors to find the ideal recipient of the tissue. Anyone who tested positive for any study or who had a history of neoplasia was dismissed as a potential donor.
All patients signed an informed consent to accept the transplantation. This study was approved by the Ethics Committee of the Hospital de Especialidades del Centro Medico Nacional de Occidente, registration number R-2012-1301-74.
Conservation of tissueOnce the donor's parathyroid tissue was removed, it was prepared for immediate transplantation following the parathyroidectomy. The tissue was cut in fragments of approximately 2 to 3mm, and one fragment was sent for intraoperative analysis to rule out malignancy. Subsequently, each of the fragments was placed inside a sterile storage tube with Celsior® preservation solution or Custodiol® to be transplanted immediately after removal.
Selection of recipientsPatients with hypoparathyroidism were identified at the general surgery outpatient service, aged between 16 and 65, who had secondary hypoparathyroidism caused by surgical procedure (thyroidectomy), with laboratory and imaging studies (parathyroid gland gammagram) that proved they had hypoparathyroidism. In addition, their calcium carbonate intake had to be higher than 2.5g/day, their calcitriol intake higher than 1 mcg/day, and they had to have gastric intolerance to calcium and/or vitamin D.
Surgical technique for transplantationAn incision of approximately 3cm was made in the nondominant forearm under local anaesthesia with Xylocaine® 1%. The dissection reached the fascia; 3 to 4 fragments of parathyroid tissue were placed in groups of 4, which were marked with metallic staples, and then the wound was tackled. The forearm was chosen as the implant site since it is an area with a well-developed vascular network, which would provide a sufficient amount of oxygen and nutrients to the implant tissue. It is also an area in which it is easy to perform ultrasonographies and control scintigrams, as tissue identification is simple.
Immunosuppression schemeAn immunosuppression scheme was used, which consisted of an induction dose of methylprednisolone 250mg. Then a cyclosporine A scheme was used, calculated at 5mg/kg/day during the first week, maintaining serum levels between 200 and 250, and decreasing the dose to suspend it after 6 months; and 20mg of prednisone was used during the first week, 15mg during the second week, 10mg during the third week, 5mg during the fourth week and a maintenance dose of 2.5mg was used until 6 months were completed. None of the patients had side effects from the cyclosporine.
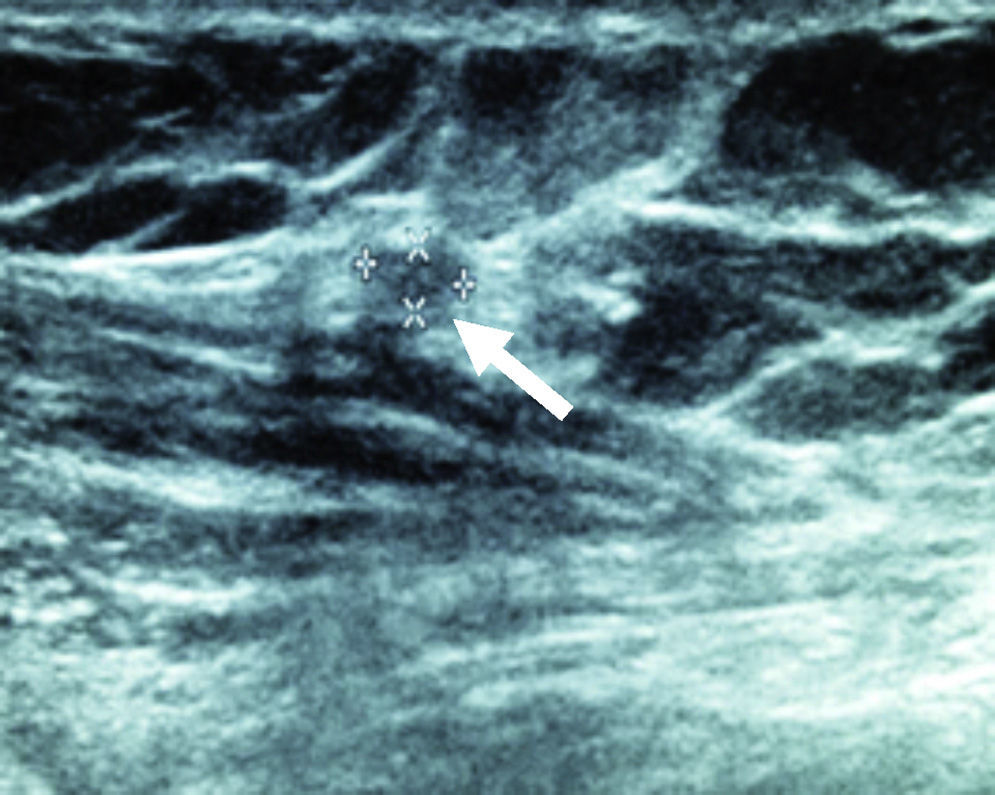
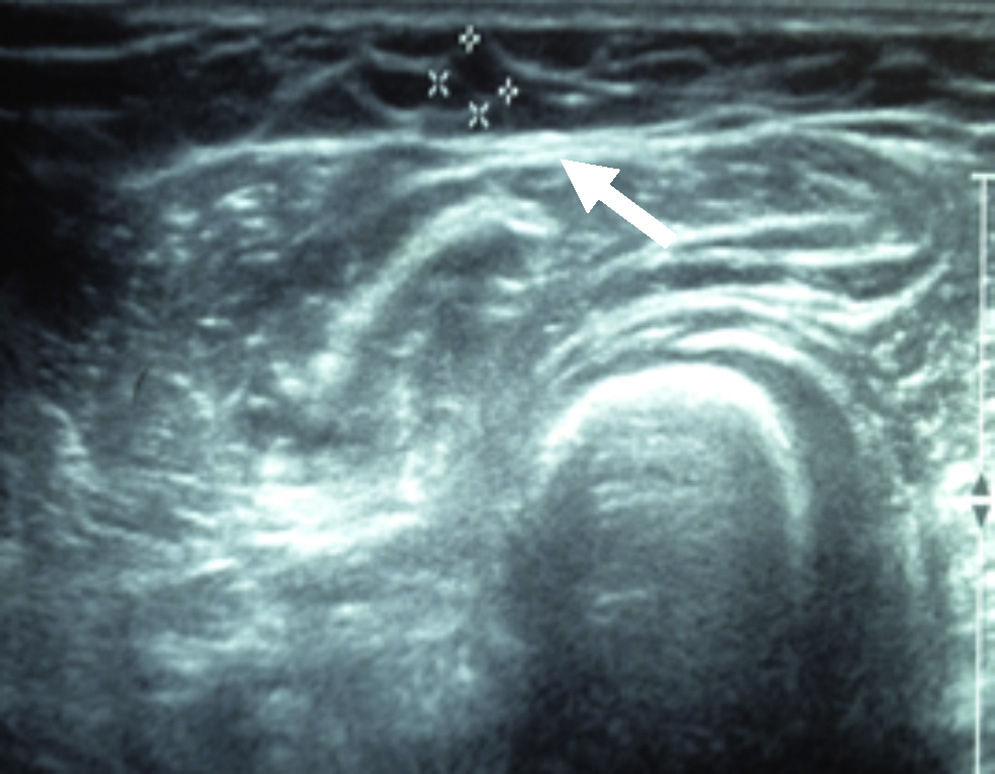
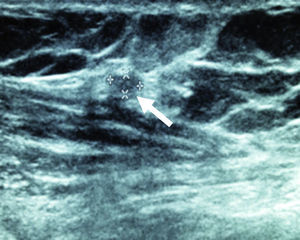
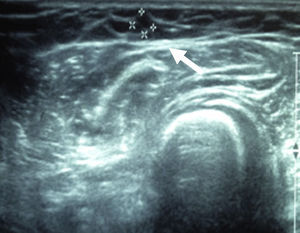
Monitoring the implant's functioningBefore the transplantation, calcium and serum parathyroid hormone (PTH) samples were taken from all the patients. PTH measurement was performed through chemiluminescence, using Siemens’ ADVIA Centaur® XP equipment. After the transplantation, samples were taken from the implanted arm to check the concentrations of calcium and PTH on post-transplant months 1, 3, 6, 9, 12 and 24. The implant was considered functional when: (1) there was an increase in PTH compared to its pre-surgical value; (2) the implant was detected by means of a gammagram with parathyroid sestamibi using Philips Precedence; (3) the implant and its vascularity was detected through an ultrasonography, and (4) the patient reduced his/her oral calcium intake. The implant was considered dysfunctional when: (1) serum PTH levels were undetectable; (2) there were clinical symptoms such as tingling or numbness, and (3) there were hypocalcaemia data that forced an increase in the oral calcium dose.
ResultsFive patients with hypoparathyroidism were included, all females. The aetiology of four patients was iatrogenic hypoparathyroidism after thyroid gland surgery. Initially, one of the patients had primary hyperparathyroidism and then hypoparathyroidism, in spite of having received an implant from her own gland. The median age of the patients was 49.8 years. All the patients received an implant from different donors, all of whom had primary hyperparathyroidism. They were selected according to their blood group (ABO) phenotype; two were A+, two O+ and one B+.
The average level of serum PTH prior transplantation was of 2.2pg/ml (SD 1.62); calcium was 8.14mg/dl (SD 0.44), phosphorus was 5.08mg/dl (SD 0.44) and urine calcium was 146.60mg/dl (SD 85.27).
During the follow-up, the numbers for serum PTH did not increase significantly during the first trimester; the median was of 2.82pg/ml (SD 1.45). However, at the third-trimester follow-up there was a significant increment with a median of 7.65pg/ml (SD 1.58). At the 24-month follow-up, the numbers were still on the rise, with a median of 19.07pg/ml (SD 6.46).
Mean presurgical levels of serum calcium were of 8.14mg/dl (SD 0.44). Its increment was more prominent during the third trimester, with a mean of 9.26mg/dl (SD 0.41). At the 2-year follow-up, the amount of calcium was stable, with a mean of 8.51mg/dl (SD 0.1); although there was no significant increase in calcium, it should be pointed out that at the 2-year follow-up the patients’ intake of calcium carbonate was lower and they had almost the same levels of serum calcium as prior to transplantation.
Throughout the follow-up period, phosphorus levels were high and although during the first month, when numbers were within a normal-high range, with a mean of 4.6mg/dl (SD 0.66), at the 12-month follow-up the mean was 5.2mg/dl (SD 0.54), and at the last 24-month follow-up the levels of phosphorus were controlled, with a mean of 5.6mg/dl (SD 0.77).
Presurgical urine calcium values were of 146.60mg/dl (SD 85.27), and after 24 months, the mean was 134.54mg/dl (SD 18.24).
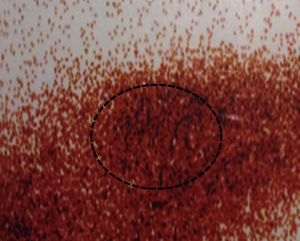
After 24 months, the sestamibi gammagram and the Doppler ultrasound reported that the radiopharmaceutical detected an implant with blood flow in four patients. In one of the patients the implant was not detected or identified in the ultrasound (Figs. 1–3).
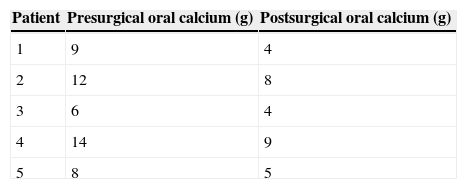
All the patients received an intake of calcium carbonate of 8.4g/day. At present, their mean intake is 6g/day and the implant is functional after a two-year follow-up. Another benefit is that they can carry out their basic daily activities without having signs of hypocalcaemia, which was not possible before transplantation (Table 1).
DiscussionAcute hypocalcaemia following a parathyroidectomy due to hyperparathyroidism is rare and has an incidence of 1 to 2%. Patients with higher risk are the ones who undergo total or near-total thyroidectomies of their parathyroid glands, whether because they have primary hyperparathyroidism or because they suffer from parathyroid gland disease associated with kidney disease (secondary or tertiary hyperparathyroidism). After parathyroid autotransplantation was recognised as a means of preventing permanent hypoparathyroidism in 1976, allotransplantation was attempted in patients for whom this was the only treatment option, to avoid the intake of high doses of vitamin D and calcium, which increase the risk of long-term complications, such as paraesthesia, multiorgan calcinosis and renal failure.6,7
Parathyroid allotransplantation is a potential therapy for permanent hypoparathyroidism7 with variable and limited results, despite having been experimentally recreated in animals and humans.7–9
There are several ways to perform parathyroid allotransplantations, among which is the parathyroid-cell culture, of which it has been reported the results are not long-lasting, with subsequent implant rejection through immune mechanisms.10–12 Alginates were used to protect the implant, and before transplantation they were treated with a 5% CO2 atmosphere; through this treatment, cells are protected from an immune response and results are functionally more long-lasting.
In our study, we decided to use a living unrelated donor; we looked for compatibility by means of blood group and HLA, as well as by an immunosuppression scheme at low doses to be able to protect the implant from acute rejection, since currently this has been shown to have more long-lasting results, such as the ones reported by Belda González et al.13 We decided to use a scheme similar to the one for renal transplantation, since it allows recovery of the implant's PTH secretion, based on a report by Flechner et al.14 who used the same immunosuppression scheme for renal transplantation in their study. It is well known that the use of these drugs is associated with high morbidity and toxicity rates, so we carried out a strict control of serum levels without seeing any complications during the follow-up period; therefore, in patients with permanent hypoparathyroidism for whom the only treatment option is allotransplantation, the use of these drugs can be justified.
Based on our results, there was a significant increase in serum PTH in four patients after a 24-month follow-up, and the results were similar to the ones reported by Belda et al.,13 where after a two-year follow-up the implant was still functional and serum PTH levels had increased; this is why we can state that parathyroid allotransplantation is a good treatment option for patients with hypoparathyroidism.
ConclusionsIn our study, it was demonstrated that parathyroid allotransplantation from a living unrelated donor with an immunosuppression scheme is a safe alternative treatment to improve the patients’ quality of life, with which the excessive intake of calcium can be reduced, as well as the complications involved in consuming high doses of calcium. In addition, it improves their quality of life by allowing them to do their basic daily activities without signs of hypocalcaemia. At present, we keep performing parathyroid transplantations with promising results at our centre, although treatment with calcium cannot be completely suspended; clinically, there is evidence of an improvement in daily life activities and a reduction of the side effects associated with the consumption of high levels of calcium.
Conflict of interestThe authors declare that there are no conflicts of interest.
Please cite this article as: Hermosillo-Sandoval JM, Leonher-Ruezga KL, Jiménez-Gómez JA, Fuentes-Orozco C, González-Ojeda A, Ramírez-González LR. Alotrasplante de paratiroides: seguimiento a 2 años. Cir Cir. 2015;83:188–92.