Hidradenitis is a disorder where abscesses appear after the infection of the apocrine sweat glands. It is located normally in the axillae, groin, perineal region, and the scalp.
Clinical caseA 37 year old male was referred by his GP to the General Surgery Department with axillary hidradenitis which had evolved over the years. The physical examination shows signs of hidradenitis in both axillae, with a noticeable suppurative hidradenitis in the right armpit. En bloc extirpation was performed to remove the whole affected area. The pathological examination revealed a cutaneous leishmaniasis. Subsequently, fucidin was administered topically, as well as local infiltrations of one millilitre of Glucantime™.
DiscussionHidradenitis normally appears in intertriginous areas and its manifestation is accompanied by recurrent subcutaneous nodules. The incidence rate in females is three times higher than in males.
The isolated Hidradenitis caused by Leishmania is a rare condition presented only in endemic areas or in immunocompromised patients, such as HIV-infected patients.
Clinical manifestations can be different and the diagnosis can be confirmed through haematoxylin–eosin. The main pattern displays a disorganised granuloma without necrosis.
Systemic or topical treatment can be applied. Immunotherapy treatment is the most common.
ConclusionsHidradenitis caused by Leishmania in HIV-negative patients is a rare condition. Therefore it is important to perform a good histological diagnosis and to administer the right treatment.
La hidrosadenitis es la abscesificación tras la infección de las glándulas sudoríparas apocrinas. Se localiza frecuentemente en: axila, ingle, periné, región perineal y cuero cabelludo.
Caso clínicoVarón de 37 años de edad, sin antecedentes personales de interés. Acudió al servicio de Cirugía General derivado por su médico de Atención Primaria por hidrosadenitis axilar de años de evolución. En la exploración física presentaba signos de hidrosadenitis en ambas axilas, con una marcada hidrosadenitis supurativa en la axila derecha. Se procedió a la extirpación en bloque de la zona afectada con resultado anatomopatológico de leishmaniasis cutánea. Posteriormente, se le administró ácido fusídico de forma tópica con infiltraciones de un mililitro Glucantime®.
DiscusiónLa hidrosadenitis supurativa afecta a zonas intertriginosas y se presenta con nódulos inflamatorios subcutáneos recurrentes. La incidencia en el sexo femenino es 3 veces superior al masculino.
La hidrosadenitis aislada por Leishmania es poco frecuente, aparece en zonas endémicas y en pacientes inmunodeprimidos, como con VIH.
La clínica puede ser muy diversa. Histopatológicamente, se puede confirmar el diagnóstico con hematoxilina-eosina. El patrón predominante presenta un granuloma desorganizado y sin necrosis.
El tratamiento puede ser sistémico o local. Actualmente, destacan las inmunoterapias.
ConclusionesLa hidrosadenitis causada por Leishmania en paciente VIH negativo es una patología muy rara. De ahí la importancia de un buen diagnóstico histológico y tratamiento adecuado.
Hidradenitis is a disorder where abscesses appear after infection of the apocrine sweat glands. It is normally located in the axillae, groin, perineal region and the scalp.1
The most standard predisposing factors are obesity, individuals with seborrheic skins and excessive sweating.2
We present the case of a male who with a suppurative hidradenitis produced by Leishmania.
Clinical caseA 37 year old male, with no personal history of interest was referred to the General Surgery Department with axillary hidradenitis which had evolved over the years. There were no other physical symptoms, nor any fever.
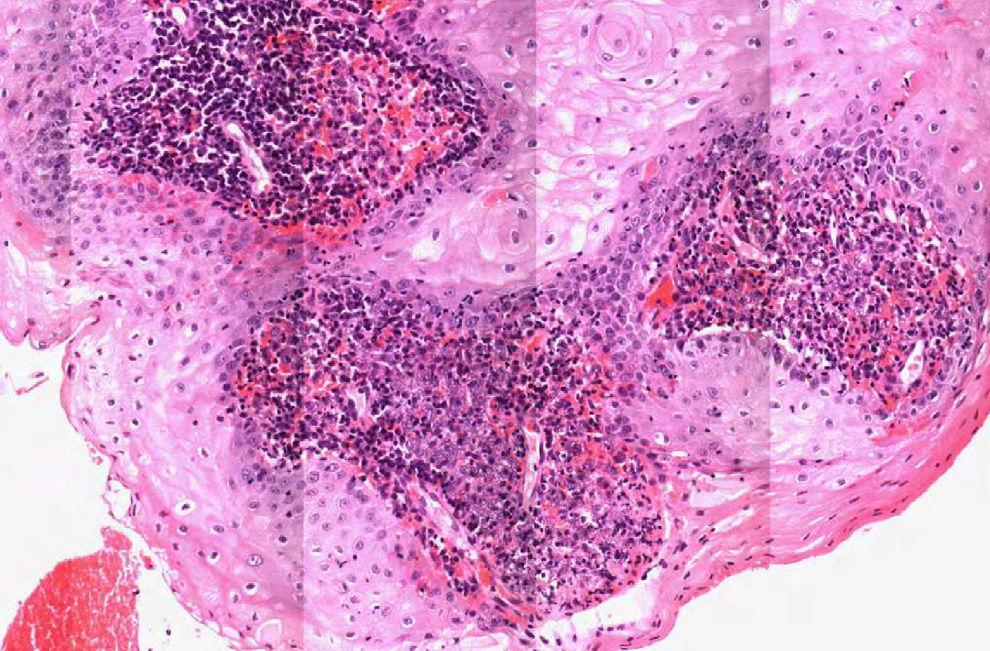
Physical examination showed signs of hidradenitis in both axillae, with a noticeable suppurative hidrosadenitis in the right armpit (Fig. 1). No malignancies were felt nor were there any other signs of clinical interest.
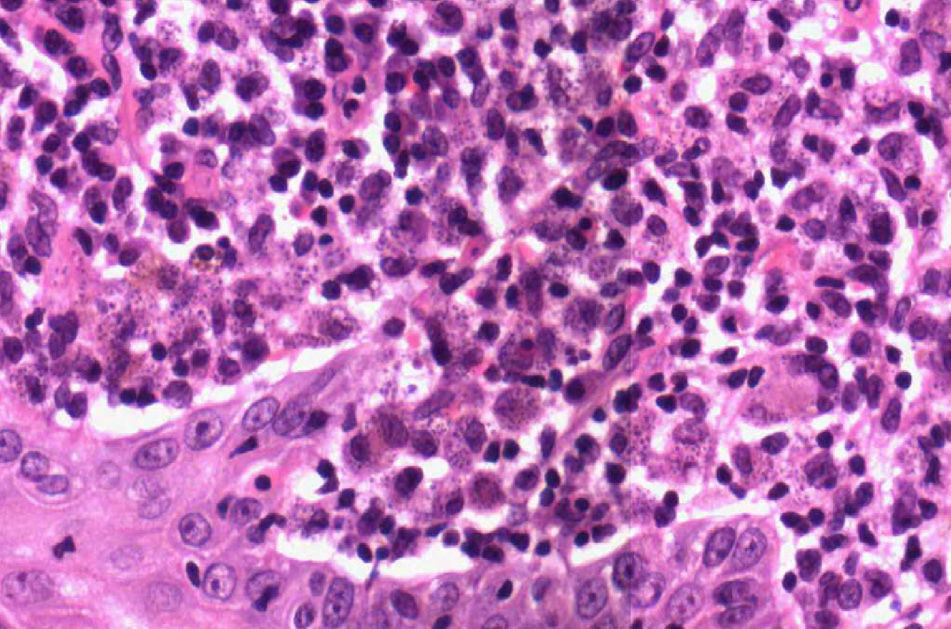
En bloc extirpation was performed to remove the whole area. The pathological examination revealed granulomatous reaction together with chronic inflammation with microorganisms in the interior of the macrophages compatible with cutaneous leishmaniasis (Figs. 2 and 3). Chain reaction polymerase reaction was requested which tested positive for Old World Leishmania. Serology was requested for the HIV virus, which tested negative and a laboratory report showed no notable changes.
The patient was treated with fucidin topically and with local infiltrations of one millilitre of Glucantime® on the scar.
Four months after the first intervention, the patient again presented with new episodes of suppuration and inflammation, and we decided to perform a new surgical extirpation. The histological study of the same sample revealed fibrosis and chronic inflammation with abundant plasmatic cells. Three months after surgery the patient was asymptomatic, with lower local inflammation, having been discharged by the General Surgery and Dermatology Department.
DiscussionSuppurative hidrosadenitis, also called inverse acne, Verneuil disease or apocrinitis, is a chronic disease which affects the intertriginous areas and its manifestation is characterised by the presence of recurrent subcutaneous inflammatory nodules.1
It is more frequent in the second and third decades of life. It is rare after menopause and children do not usually get it, unless they present with early adrenarche.3 Incidence rate in females in 3 times higher than in males.4
Isolated hidradenitis caused by Leishmania is considered an infrequent form of cutaneous leishmaniasis.5 It appears in endemic areas and currently affects immunocompromised patients more frequently, such as patients infected with HV.6
Patients with adenopathies and hidrosadenitis are studied for probable infection by infection by Staphylococcus, Streptococcus.7
Leishmaniasis is an infectious disease which is caused by an intracellular protozoa transmitted by a mosquito bite, which inoculates the parasite through the subject's skin.8 There are 3 forms of clinical presentation: cutaneous, mucocutaneous and visceral. In immunocompromised patients, essentially HIV-infected, the most common form is generalised visceral.6
The vectors responsible for transmission are phlebotomus females. In the Old World species the main vectors belong to the Phlebotomus (in Spain P. perniciosus) species.5
There are approximately 1–1.5 million cases per year, mainly in endemic areas,9 although they may also affect travellers.10,11 In Spain incidence is unknown, since this is not currently a disease which is forcibly declared.12
Clinical symptoms may be very diverse, from asymptommatic to presenting serious physical symptoms. When symptoms are cutaneous, single lesions may appear which develop slowly, or multiple lesions which mature more rapidly.
Histopathologically, if we stain the infected tissues with haematoxylin–eosin, diagnosis of the disease may be confirmed in the majority of cases. Although there is variability, the predominant pattern is characterised by the presence of a disorganised granuloma without necrosis. Leishmania normally appears as a bright blue colour with Giemsa and the Leishman-Donovan bodies which are round or oval shaped, are generally visible within the macrophages but may also be visible in extracellular areas. One prospective study conducted in Saudia Arabia in 2005 described 4 different groups: type A, with highly parasitic and vaculolated macrophages with some lymphocytes; types B and C, which present a mixed inflammatory response, with or without necrosis (Old World cutaneous leishmaniasis). Lastly type D, which presents a tuberculoid granuloma with absent or low parasitic load, and is associated with chronic forms such as lupoid leishmaniasis or the final stage of spontaneous curation.13
The existence of foreign body granulomas, infections from microbacterias such as cutaneous tuberculosis, fungal infections such as paracoccidioidomycosis and histoplasmosis in travellers to endemic areas, leprosy, sarcoidosis, syphilis, cutaneous tumours, sporotrichosis and trauma ulcers form differential diagnosis of cutaneous presentation.14,15
Treatment may be systemic or local.
Systemic treatment is based on the use of pentavalent antimonial drugs (Glucantime®)16 and sodium stibogluconate (Pentostam®),13 pentamidine, metronidazole, amphotericin B or azoles.
Local treatment is administered in intralesional injections of pentavalent antimonial drugs (1–3ml injection is recommended below the edges of the lesion). Cryotherapy has also been considered useful since the Leishmania is sensitive at low temperatures. In particular it is used for small lesions. Other treatments include: the use of aminoside, which is an antibiotic of the amino glycoside family, imiquimod, thermotherapy, CO2 laser, dynamic phototherapy or electrotherapy.13
Lastly, immunotherapies have played an important role here; they are based on the consideration that Leishmania produces an infection which generally induces memory and protection against new immunological infections for life. This infection requires the generation of Th1 response represented by the production of gamma interferon in absence of Th2 response, which is associated with IL-4 and IL-10.13
ConclusionHidradenitis caused by Leishmania in HIV negative patients is a very rare pathology, which may lead to erroneous diagnosis. Good diagnosis through histological study is important and thus the ability for proper treatment. For this reason we believe it is necessary to further expand our clinical case.
Conflict of interestsThe authors have no conflict of interest to declare.
Our thanks to doctor Aurora Gil Rendo, because she provided us with case study data and to doctor Esther Pilar García Santos, for her help in the entire data collecting process, plus creation and support. We are also greatly indebted to Laura Flores Perez, without whom this would not have been possible.
Please cite this article as: Alberca-Páramo A, García-Santos EP, Sánchez-García S, Ruescas-García FJ, Bertelli-Puche JL, Martín-Fernández J. Hidrosadenitis axilar por Leishmania: presentación de un caso y revisión de la bibliografía. Cir Cir. 2016;84:253–256.