Desmoid tumours are one of the rarest tumours worldwide, with an estimated yearly incidence of 2–4 new cases per million people. They are soft tissue monoclonal neoplasms that originate from mesenchymal stem cells. It seems that the hormonal and immunological changes occurring during pregnancy may play a role in the severity and course of the disease.
Clinical caseThe case is presented on 28-year-old female in her fifth week of gestation, in whom an abdominal wall tumour was found attached to left adnexa and uterus while performing a prenatal ultrasound. The patient was followed up under clinical and ultrasonographic surveillance. When she presented with abnormal uterine activity at 38.2 weeks of gestation, she was admitted and obstetrics decided to perform a caesarean section. Tumour biopsy was taken during the procedure. Histopathology reported a desmoid fibromatosis. A contrast enhanced abdominal computed tomography scan was performed, showing a tumour of 26cm×20.5cm×18cm, with well-defined borders in contact with the uterus, left adnexa, bladder and abdominal wall, with no evidence of infiltration to adjacent structures. A laparotomy, with tumour resection, hysterectomy and left salpingo-oophorectomy, components separation techniques, polypropylene mesh insertion, and drainage was performed. The final histopathology report was desmoid fibromatosis. There is no evidence of recurrence after 6 months follow-up.
ConclusionsDesmoid tumours are locally aggressive and surgical resection with clear margins is the basis for the treatment of this disease, using radiotherapy, chemotherapy and hormone therapy as an adjunct in the treatment.
Los tumores desmoides son neoplasias raras monoclonales de tejido blando, que surgen a partir de células madre mesenquimales. Son uno de los tumores más raros en todo el mundo, con una incidencia anual estimada de 2-4 nuevos casos por millón de personas. Los cambios hormonales e inmunológicos que ocurren durante el embarazo pueden desempeñar un papel en la severidad y curso de la enfermedad.
Caso clínicoMujer de 28 años de edad, en su quinta semana de gestación, a quien, al realizar ultrasonido de control prenatal, se le encontró tumoración de pared abdominal adherida a anexos izquierdos y útero. Se dejó a la paciente en vigilancia clínica y ecográfica. Acudió con actividad uterina anormal, se ingresó a Obstetricia con 38.2 semanas de gestación, se realizó cesárea y se tomó biopsia de la tumoración. Anatomía patológica reporta fibromatosis desmoide. Se realizó tomografía axial computada contrastada, que reportó tumoración con bordes bien definidos, en contacto con el útero, anexo izquierdo, vejiga y pared abdominal; sin datos de infiltración a estructuras adyacentes de 26×20.5×18cm. Se operó de forma electiva, se realizó laparotomía exploradora, con resección tumoral, histerectomía y salpingo-ooforectomía izquierda, técnica de separación de componentes, colocación de malla de polipropileno y drenajes. El reporte definitivo de enfermedad fue fibromatosis desmoide. Seis meses después de su intervención quirúrgica no ha presentado recurrencia.
ConclusiónLos tumores desmoides son localmente agresivos y la resección quirúrgica con márgenes libres representa la base en el tratamiento de esta dolencia; la radioterapia, quimioterapia y la hormonoterapia se utilizan como complemento en el tratamiento de estas pacientes.
Desmoid tumours (or desmoid fibromatosis) are rare soft tissue monoclonal neoplasms arising from the mesenchymal stem cells. No association with metastatic disease has been reported. However, they often show a strong tendency to infiltrate local adjacent tissue, which causes significant morbidity and mortality.1 Desmoid tumours are amongst the rarest in the entire world, with an estimated annual incidence of 2–4 new cases per million people.2,3
Desmoid tumours associated with pregnancy are rarer still, with few available publications in the literature. They have no known aetiological factor, however they can be associated with some familial syndromes such as familial adenomatous polyposis.2 They have also been associated with hyperoestrogenic states and trauma, but the evidence for this is largely based on retrospective cases and anecdotal. Hormonal and immunological changes that occur during pregnancy can play a role in the severity and course of the disease.1
Clinical caseA 28-year-old women in the fifth week of gestation who, during a routine prenatal ultrasound, was found to have mass of approximately 11cm×15cm×18cm, involving the left adnexa and uterus. The patient was placed under clinical and ultrasound surveillance. She consulted with abnormal uterine activity and was admitted to the obstetrics department at 38.2 weeks gestation. She underwent a midline caesarean section and a mass was found adhering to the abdominal wall, uterus and left adnexa. The general surgery department were consulted during the operation, a biopsy of the mass was taken and it was decided not to intervene until definitive diagnosis. The anatomopathological result was desmoid fibromatosis.
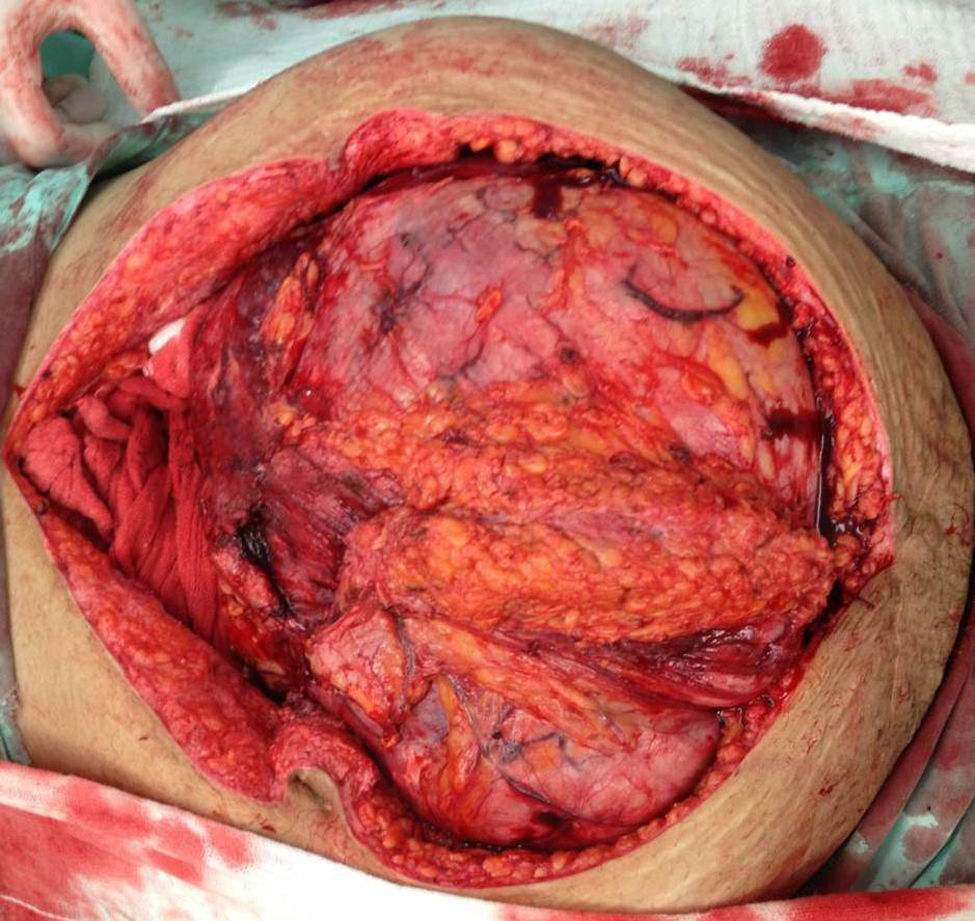
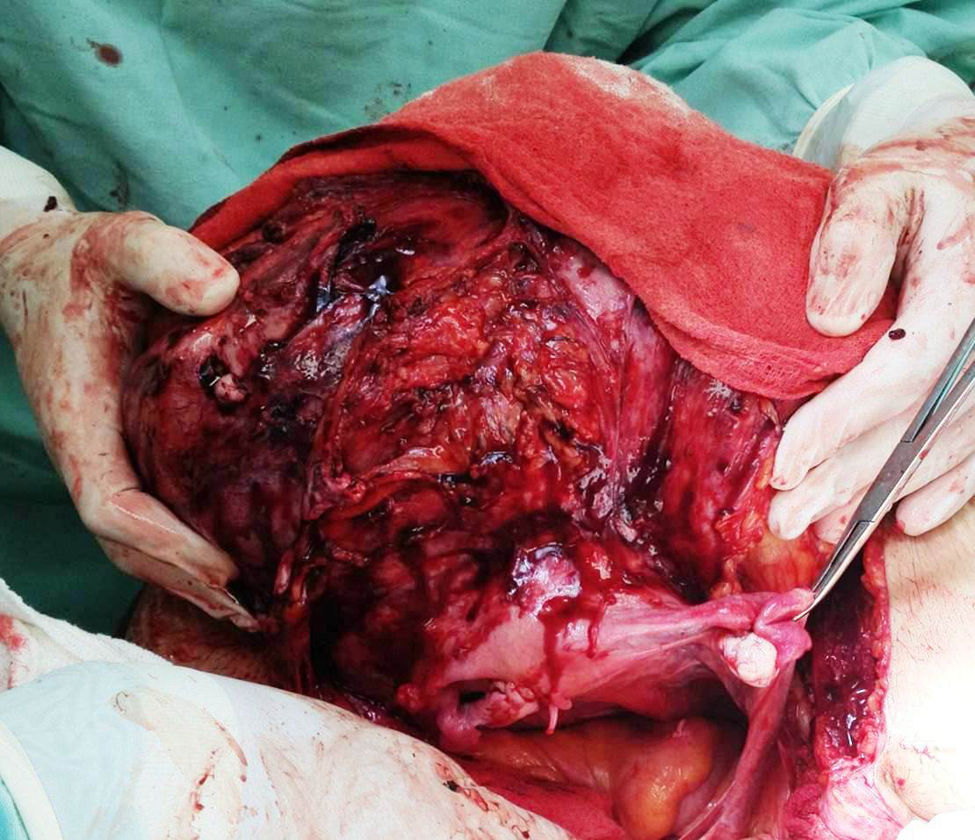
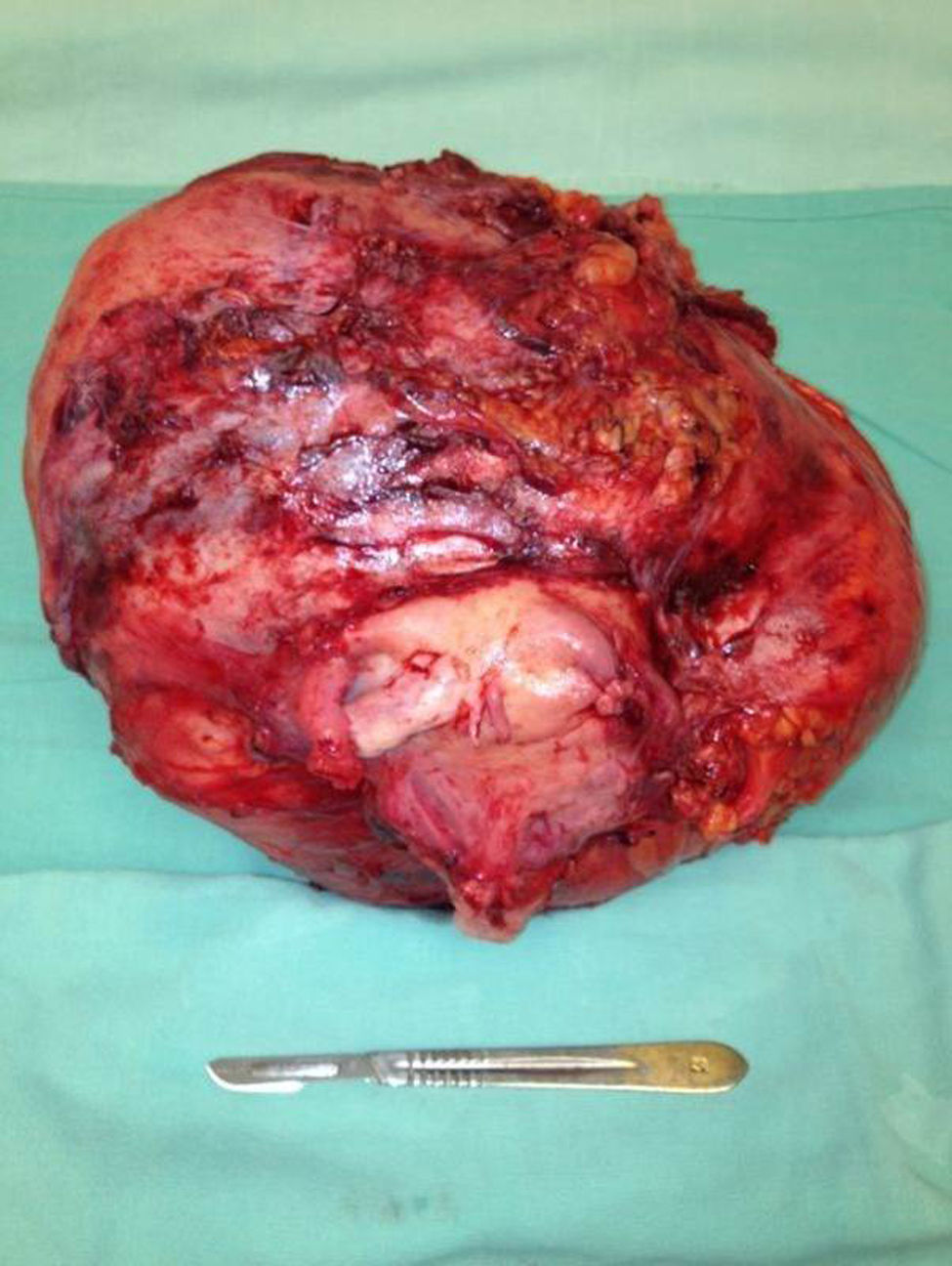
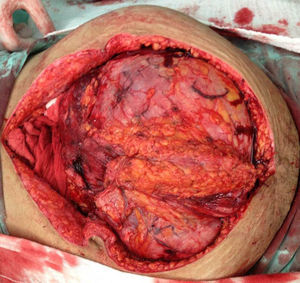
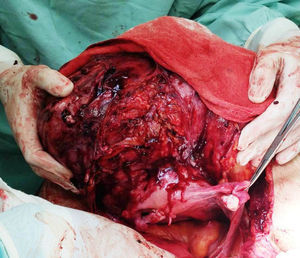
The patient was referred to the general surgery clinic. Physical examination found a distended, soft abdomen, peristalsis was present and there was no pain on palpation. The laboratory tests reported haemoglobin 11.5g/dl. Contrast computed axial tomography (CAT) was performed, which reported a mass with well-defined borders, in contact with the uterus, left adnexa, bladder and abdominal wall, with no signs of infiltration to adjacent structures. The mass was homogeneous with soft tissue density, with slight enhancement of contrast medium, measuring 26cm×20.5cm×18cm (Figs. 1 and 2). Elective surgery was performed by exploratory laparotomy, which found a large intraperitoneal mass (Fig. 3), adhering to the abdominal wall, uterus, left adnexa (Figs. 4 and 5), bladder and pubic symphysis. Resection of the tumour, hysterectomy and left salpingo-oopherectomy were performed, leaving an abdominal wall defect of 10cm×10cm. The component separation technique was performed, and placement of a polypropylene mesh and drains. The definitive anatomopathological study concluded a desmoid mass weighing 5.680g and measuring 30cm×24cm×6cm, of irregular shape, with smooth outer surface, nodular, pinkish-coffee in colour, with prominent vascular network and partially covered in fibroadipose tissue. The patient made good progress and was discharged on the fifth postoperative day. Six months after the intervention there was no recurrence of the tumour.
Aggressive growth of a desmoid tumour during pregnancy is a rare phenomenon.1 Several studies have demonstrated that desmoid tumours comprise only 0.03% of all neoplasms and 3% of all soft tissue tumours. The majority of cases occur between the ages of 15 and 60 years, with a peak incidence between 25 and 35 years.4 No significant differences have been recorded between the genders in people with familial adenomatous polyposis. However tests have shown that oestrogen can play a role in the pathogenesis and clinical course of sporadic tumours. In fact, an incidence of oestrogen receptor positivity up to 33% has been reported, with equal sex distribution.1
According to Gomez Pedraza et al.5 the first description was by McFarlane in 1832 and the term desmoid was applied in 1856 by Müller, based on the Greek etymology “desmos” referring to tendinous tissue.5,6 Although histologically desmoid tumours are benign and lack the capacity to metastasise, they can invade locally, often aggressively, grow large in size and reappear repeatedly.3
These are tumours that can also occur in the abdominal cavity organs, principally the uterus, and they can locate in the extremities (30–34%), muscles of the trunk (37–38%) and other less common sites such as the head and neck (8–10%), and abdominal cavity (19–24%).5
Ultrasound remains the most used method for initial assessment of an intra-abdominal mass suggestive of a desmoid tumour.1 On CAT they can appear homogeneous or heterogeneous and hypo-, iso- or hyperintense compared to muscle attenuation. On MRI, the characteristic findings are poorly defined margins, low intensity on T1-weighted images and heterogeneity on T2-weighted images and varying contrast medium enhancement. MRI is better than CAT in defining the structure and the extension of the disorder, and in determining whether there has been a recurrence after surgery. Although both CAT and MRI help to establish the extent of local invasion.7
Seventy-five percent of all patients have a progressive growth pattern which requires prompt surgical treatment. Because desmoid tumours are so rare and due to the lack of available data on how to treat them surgically, there are no specific guidelines or standardised therapeutic approach for their management.2 Complete surgical excision with wide tumour-free margins is the current treatment for primary and recurrent desmoid tumours.4 Case reports with successful surgical treatment during and after pregnancy have been described in the medical literature.1
Preoperative biopsy is recommended for differential diagnosis with intestinal carcinoma, carcinoid tumour, mesenteric fibromatosis, lymphoma and retroperitoneal fibrosis.2 Clinical characteristics and imaging are not sufficient to fully differentiate a desmoid tumour from other soft tissue tumours.1
Incomplete removal of the tumour or positive surgical margins can result in local recurrence (from 20% to 77%, depending on the location, extension and whether there was complete initial resection). Desmoid tumours of the abdominal wall have a significantly lower recurrence rate (20–30%), which, in general, becomes evident within 6 months after removal.7
Radiotherapy, chemotherapy and hormone therapy are used in patients with inoperable tumours, local recurrences or lesions that have been incompletely extirpated.7
Radiotherapy has been studied for primary treatment as well as adjuvant treatment for desmoid tumours. The best local control of desmoid tumours is achieved with radiotherapy alone or surgery plus radiotherapy. Radiation doses of >56Gy do not significantly improve local control, but are associated with a greater risk of complications, especially in patients aged 30 or younger. Complications include fibrosis, soft tissue necrosis, anaesthesia/paraesthesia, pathological fracture, secondary malignant neoplasms, oedema and, rarely, vascular complications that require amputation. The currently recommended radiotherapy dose is 50–56Gy in 2Gy fractions. Radiotherapy is still controversial, despite the high rates of local control of the disease, due to the risk of complications, particularly in younger patients.3
A review of the literature helped us conclude that the rates of local control with surgery plus radiotherapy or radiotherapy alone are significantly better than surgery alone, regardless of the margins achieved in surgery. The relative superiority of radiotherapy alone or in combination with surgical treatment increases in cases with positive margins.8
With regard to pharmacological treatment, most of the published literature only comprises case reports or series of cases with limited numbers of patients and inconclusive results to demonstrate a benefit. The most used agents are: (a) anti-hormonal drugs (tamoxifen, toremifene, progesterone, prednisolone), because desmoid tumours have oestrogen receptors, especially those that are associated with familial adenomatous polyposis. (b) Non-steroidal anti-inflammatory drugs (indomethacin, meloxicam), due to the probable dependence of the tumour on prostaglandins for growth and (c) interferons and cytotoxic drugs (metotrexate/vinblastine, pegylated liposomal doxorubicin).5
Our patient responded well to elective surgical treatment after her caesarean. We were able to undertake the surgery after a definitive report of desmoid fibromatosis. The operation required separation of components and placement of a polypropylene mesh, therefore intervention prior to the caesarean section would have complicated good closure of the abdominal wall.
ConclusionDesmoid tumours are locally aggressive. Surgical resection with free margins is the baseline treatment for this disorder. Radiotherapy, chemotherapy and hormone therapy can complement the surgical treatment of these patients. The presence of these tumours during pregnancy has been seldom reported. However, when these tumours appear, mother and foetus should be strictly monitored, due to their high association with a hyperoestrogenic state associated with pregnancy and because they can grow rapidly. Surgical resection should be decided during or after pregnancy depending on the risk to mother and foetus, based on each individual case.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Palacios-Zertuche JT, Cardona-Huerta S, Juárez-García ML, Valdés-Flores E, Muñoz-Maldonado GE. Reporte de caso: tumor desmoides gigante de pared abdominal con rápido crecimiento durante el embarazo. Cir Cir. 2017;85:339–343.