Mucoceles are benign cystic lesions of the paranasal sinuses. Endoscopic marsupialisation is considered the first choice of treatment, due to its low morbidity and recurrence rates.
ObjectiveTo establish the number of patients with recurrence, who were diagnosed clinically or by computed tomography, and who were submitted to surgery in the Ear, Nose and Throat Unit in a tertiary university hospital.
Material and methodsA clinical, cross-sectional, descriptive, observational and retrospective study was conducted on patients with a mucocele diagnosis operated on in the period from January 2006 to December 2013. A descriptive statistical analysis was performed to obtain the frequencies, ratios and proportions. Measures of central tendency and dispersion were obtained. The recurrence rates of each surgical technique were compared using the Chi-squared test.
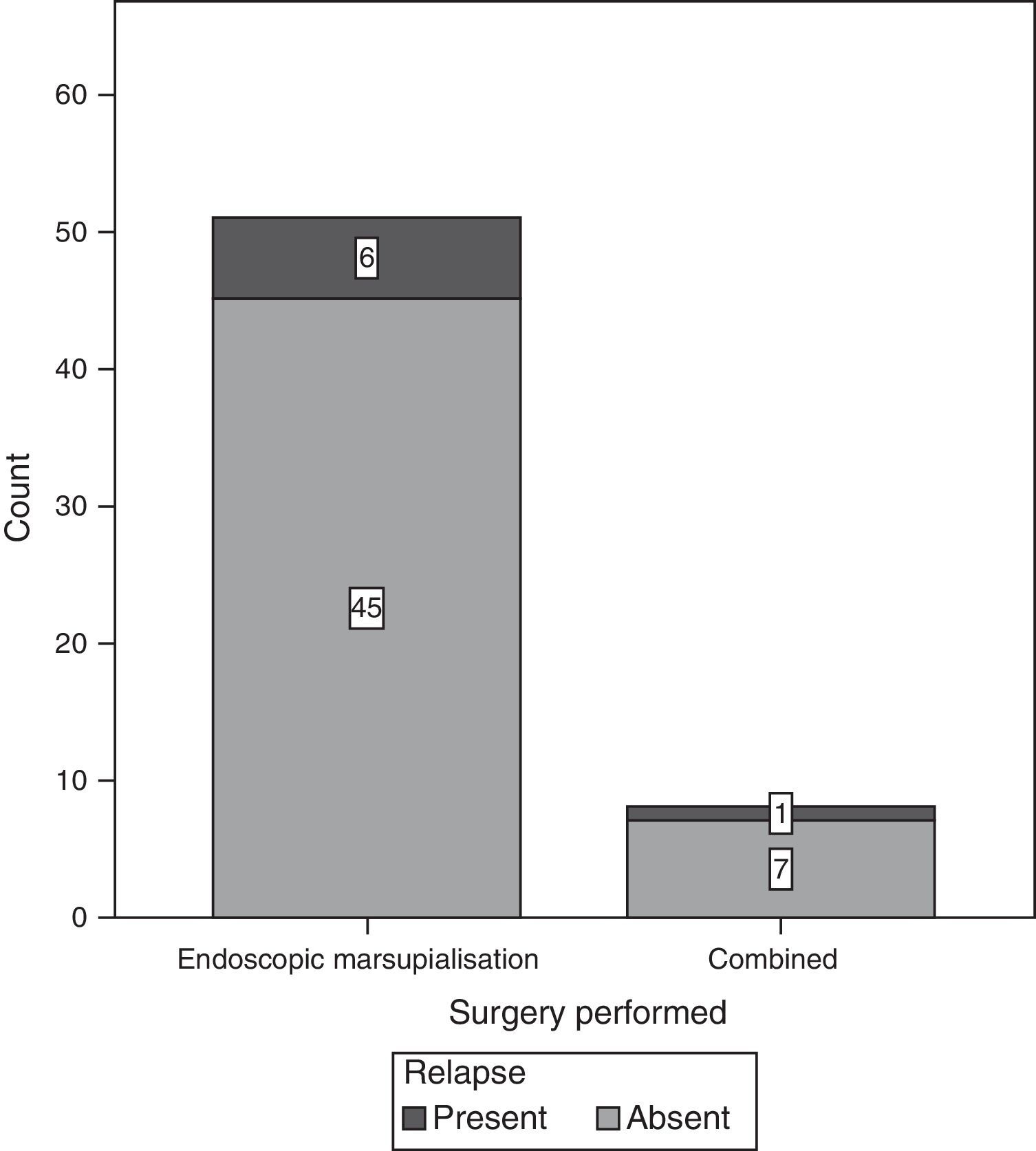
ResultsOf the 59 patients included in the study, 39 were female and 20 were men. The most common location was in the maxillary sinus (22 patients) followed by frontoethmoidal (20 patients). There was a recurrence of 9% in those submitted to a surgical procedure. The endoscopic approach was used in 51 patients, 8 cases were combined (open plus endoscopic), and there was no open approach. There was a recurrence in 7 of 51 of patients with endoscopic surgery, and one out of 8 patients had a recurrence with a combined technique.
ConclusionsNo statistically significant relationship was found between the type of surgery and recurrence, or between the presence or absence of a predisposing factor and recurrence.
El mucocele es una lesión quística benigna de los senos paranasales. El tratamiento de elección con bajas tasas de morbilidad y recurrencia es la marsupialización vía endoscópica.
ObjetivoDeterminar la cantidad de pacientes con recurrencia de mucocele, que recibieron tratamiento quirúrgico en el Servicio de Otorrinolaringología de un hospital universitario de tercer nivel.
Material y métodosEstudio clínico, transversal, descriptivo, observacional y retrospectivo. Universo de trabajo: 59 pacientes operados con el diagnóstico de mucocele, de enero del 2006 a diciembre del 2013. Análisis estadístico: descriptivo con frecuencias, razones y proporciones; se obtuvieron medidas de tendencia central y de dispersión, se compararon las recidivas de cada técnica quirúrgica.
ResultadosSe analizó a 59 pacientes, 39 mujeres y 20 hombres. La localización más común fue en el seno maxilar (22 pacientes), seguido por frontoetmoidal (20 pacientes). Del total de los pacientes que fueron tratados mediante el procedimiento quirúrgico, 9% presentaron recidiva de la lesión. En cuanto al tipo de abordaje quirúrgico, encontramos 51 pacientes con manejo endoscópico y 8 casos combinados (endoscópico y externo), en ningún caso se realizó el manejo abierto exclusivamente. De los operados por vía endoscópica, 7 de 51 tuvieron recidiva y uno de los 8 con técnica combinada la presentó.
ConclusionesNo se apreció asociación estadísticamente significativa entre el tipo de cirugía y la presencia de recidiva; tampoco se demostró relación significativa entre la presencia o ausencia de factor predisponente y la aparición de recidiva.
Mucocele is a benign cystic lesion of the paranasal sinuses, which are covered by pseudostratified columnar epithelium of the upper respiratory tract. They contain mucus that is sterile in the majority of cases. In spite of their benign nature, mucoceles slowly expand and destroy the bone structure adjacent to the paranasal sinuses.1
Jaswal et al.2 state that mucoceles were first described by Lagenbeck in the 19th century, although their history goes back further. In the 3rd century BC Cannalis described a cranium with changes in the frontal sinus, indicating that the specimen probably had a mucocele. Until Rollet used the term mucocele in 1886, these lesions were known as hydatid cysts, from the Greek hydatis “drop of water”.2
They may be classified as primary or secondary. The first originate due to anatomical obstructions caused by mucus membrane hyperplasia or mechanical fractures. Their formation may be attributed to blockage of mucus drainage due to an inflammatory process, obstruction of the secretor duct, cystic dilation of the mucus glands and cystic degeneration of polyps. Secondary mucoceles originate due to sequestration of residual mucus and the long-term retention of fluids in tissues.3
Lund4 suggests that obstruction of the drainage from a paranasal sinus in combination with an additional infection leads lymphocytes and monocytes to free cytokines, stimulating fibroblasts to secrete prostaglandins and colagenases, which may stimulate bone re-absorption and lead to expansion of the mucocele.4
In their clinical presentation mucoceles occur equally in both sexes and may arise at any age, although the majority are diagnosed when they are from 40 to 60 years old.5
Mucoceles predominantly affect the frontal sinus (60–65%), followed in order of frequency by the ethmoidal (20–30%), maxillary (10%) and sphenoidal sinuses (2–3%).6 They cause slow and progressive expansion and dilation of the paranasal sinuses, leading to symptoms such as: cephalea, nasal blockage, facial pain, a fall in visual acuity, diplopía, displacement of the eyeball and facial oedema.7
In severe cases patients may present: keratopathy due to secondary exposure to exophthalmos, an increase in the volume of the region of the forehead due to erosion of the anterior table and fistula of the cerebrospinal fluid or meningitis secondary to erosion of the posterior table, with subsequent intracranial expansion.5
The pressure exerted by the mucocele causes thinning of the bone wall and finally expansion at the point of least resistance adjacent to important structures, such as: the orbit and cranial cavity. If it is allowed to grow, it leads to significant morbidity and potential mortality.8
A high rate of intracranial extension has been reported (55%): half of these patients have a larger intracranial than sinusal component. An infection may arise due to the mucus stagnating in the cyst, giving rise to a mucopyocele. This may cause rapid expansion of the lesion, with an increase in the incidence of local complications.5
Diagnosis is based on clinical history, physical examination and radiological findings. Computed tomography is the imaging technique of choice for mucocele.2 It is used to determine the regional anatomy and size of the lesion; more specifically its intracranial extension and bone erosion. 3 criteria are used to diagnose a mucocele using tomography: a homogeneous isodense image, a clearly-defined margin and irregular osteolysis around the lesion. Erosion of the sinus wall with marginal sclerosis is also a suggestive finding.9
Magnetic resonance imaging is useful too when evaluating intracranial extension or to differentiate a mucocele from a neoplasia. In the majority of cases a mucocele will be: hypointense in T1 and hyperintense in T2, with no enhancement following the application of gadolinium. In general, when the concentration of proteins increases in association with a mucocele that has evolved over a long time, the T1 signal increase and the T2 signal decreases, which would cause confusion of these lesions with fungi or accumulated secretions.5
To standardise the description, analysis, communication between surgeons, treatment approaches and results, the following classification is used for frontal and frontoethmoidal mucoceles10: type 1, limited to the frontal sinus (with or without orbit involvement); type 2, frontoethmoidal mucocele (with or without extension into the orbit); type 3, erosion of the posterior wall which may be minimal or without intracranial extension, or with greater intracranial extension; type 4, erosion of the anterior wall and type 5, erosion of the anterior and posterior walls with minimum or no intracranial extension, or with greater intracranial extension.
The definitive treatment for mucocele is surgery. Until 1980 mucoceles were mainly resected using external approaches that included: the Lynch–Howarth incision, frontal sinus osteoplastic sinusotomy and the Caldwell-Luc procedure.11 These techniques are associated with significant morbidity and cosmetic deformity, as well as with a relatively high rate of relapse.5
The Lynch–Howarth incision is made in the superomedial quadrant of the orbit. The lesion is completely resected together with the frontal sinus mucus membrane, and the nose is broadly drained. The procedure includes the resection of the anterior and lateral ethmoidal wall; this may lead to prolapse of the soft tissue in the frontal recess and the obstruction of sinus drainage.11
The Caldwell-Luc procedure was the treatment of choice for involvement of the maxillary sinus, and it includes an open approach in the anterior wall of the maxillary sinus through an incision in the gingival-oral sulcus. The content of the sinus is removed and the diseased mucus membrane after the creation of a window in the bone.4
Before 1990 mucoceles were treated by external frontoethmoidectomy with or without the placement of a stent in the nasofrontal duct. The majority of surgeons now exclusively prefer to use an endoscopic nasal approach. The benefits of this technique include: the preservation of the bone structure of the affected sinus, a shorter operation, avoiding external incisions and a lower hospitalisation cost.7
Paranasal sinus surgery has evolved over time. Because of its size and accessibility the maxillary sinus used to be the centre of attention for the study of problems and surgical procedures. This has changed over time and now, thanks to scientific and technological advances, attention centres on the anterior ethmoidal sinus. Endoscopic surgery has progressed greatly, and it is now used in all of the paranasal sinuses for many ailments that until 20 years ago were treated using open approaches.
In 1989, Kennedy et al.12 suggested an alternative endoscopic approach that showed zero relapses after an average follow-up of 18 months. The marsupialisation of mucoceles using an endoscopic approach is now the treatment of choice, with low rates of morbidity and relapse. External approaches are still used for the frontal sinus, either alone or in combination with endoscopic surgery in laterally located lesions.
To compare the different approaches it is necessary to know the indications, advantages, complications and basic concepts corresponding to each one.
In several series with more than one hundred endoscopically-treated cases the relapse rate varies from 0.9% to 2.2%. In other series with a small number of cases and a short follow-up time the relapse rates stand at from 11% to 13% of cases.6
Open procedures are considered to be the treatment of choice for the management of frontal sinus mucoceles. These procedures include: cranialisation or osteoplastic flap with obliteration of the sinus. Although these procedures are highly effective, they also involve a high level of morbidity and difficulty in evaluating postoperative radiological images.10
The relapse rate for these approaches to the frontal sinus has been reported to stand at 19%.3 The decision to use an endoscopic approach in frontal mucoceles is influenced by several factors: the extension and location of the mucocele, the anatomy of the frontal sinus, the experience of the surgeon and the presence of a cutaneous cyst.
A lateral location in the frontal sinus usually merits a combined procedure mixing a traditional external approach with endoscopic techniques. These procedures include: external trephination of the frontal sinus plus endoscopy, or endoscopy with a Lynch–Howarth incision or endoscopy with external osteoplastic sinusotomy; nevertheless, there are no definitive criteria for selecting the best surgical approach, and choice is based on the experience of each surgeon. The prevention and detection of recurring mucoceles is one of the main challenges in treating this ailment. To this end regular check-ups and a prolonged follow-up are recommended to detect asymptomatic lesions before the onset of complications. Computed tomography should be performed every 2 years for at least 4 or 5 years.13
ObjectiveTo determine the number of patients with recurring mucocele diagnosed either clinically or tomographically and who were treated surgically, to compare the different types of surgical approach in terms of lesion relapse and the complications deriving from these procedures.
Material and methodsType of study: transversal and clinical, descriptive, observational and retrospective. It includes patients of the Ear, Nose and Throat Department of the Unidad Médica de Alta Especialidad of the Hospital de Especialidades, attached to the Centro Médico Nacional Siglo XXI, diagnosed with mucocele of the paranasal sinuses and treated surgically from 1 January 2006 to 31 December 2013. The inclusion criteria were: above the age of 18 years old, with a diagnosis of mucocele, having been operated in the same reference hospital and with a complete clinical record. The exclusion criteria were: not having a clinical record on file or an incomplete record that prevented data gathering, or having lost the right to social security coverage during follow-up.
The variables studied were: dependent variables: lesion recurrence (qualitative) and independent variables: predisposing factors (dichotomous and qualitative), the surgical technique used (qualitative) endoscopic marsupialisation, open or combined technique (Cadwell-Luc plus an endoscopic approach, frontal osteoplastic procedure plus an endoscopic approach), age (quantitative) and sex (dichotomous and qualitative) and the procedure.
All of the patients diagnosed with mucocele and treated surgically in the period from 1 January 2006 to 31 December 2013 were identified in the surgical records. Based on these data patient files were requested from the unit archive to obtain the study data.
All of the data obtained from the files were recorded in the data collection sheet, including age, sex, patient symptoms before and after the operation, personal history, the location and extension of the condition, laboratory studies used, the surgery that was performed, transoperative findings and postoperative evolution.
A descriptive analysis was performed, including frequencies, ratios and proportions. Measurements of central tendency were obtained (mean, median and mode) as well as dispersion (standard deviation). Relapses corresponding to each surgical technique were compared using the chi-squared test. Multivariate analysis was performed using logistic regression, including in the model the type of surgery performed, the presence of a predisposing factor and lesion extension. The SPSS 20 (MR) programme was used, together with Excel (MR) for statistical analysis.
Regarding ethical considerations, this study respects the institutional, national and international norms governing research in human beings. Patient identity is confidential, given that this is a descriptive study that uses their clinical records as a source of information. No patient names are included and no invasive procedures were applied.
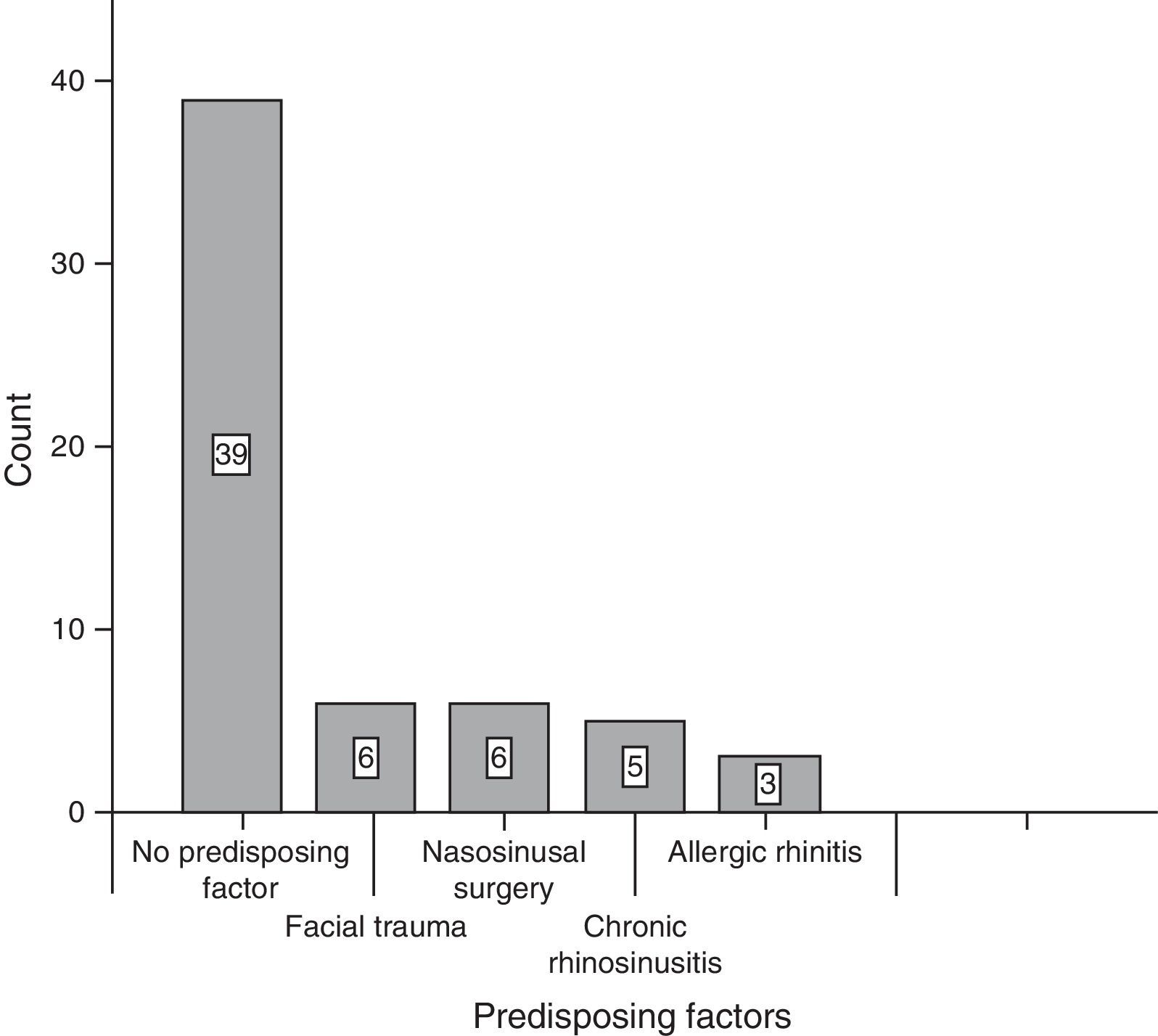
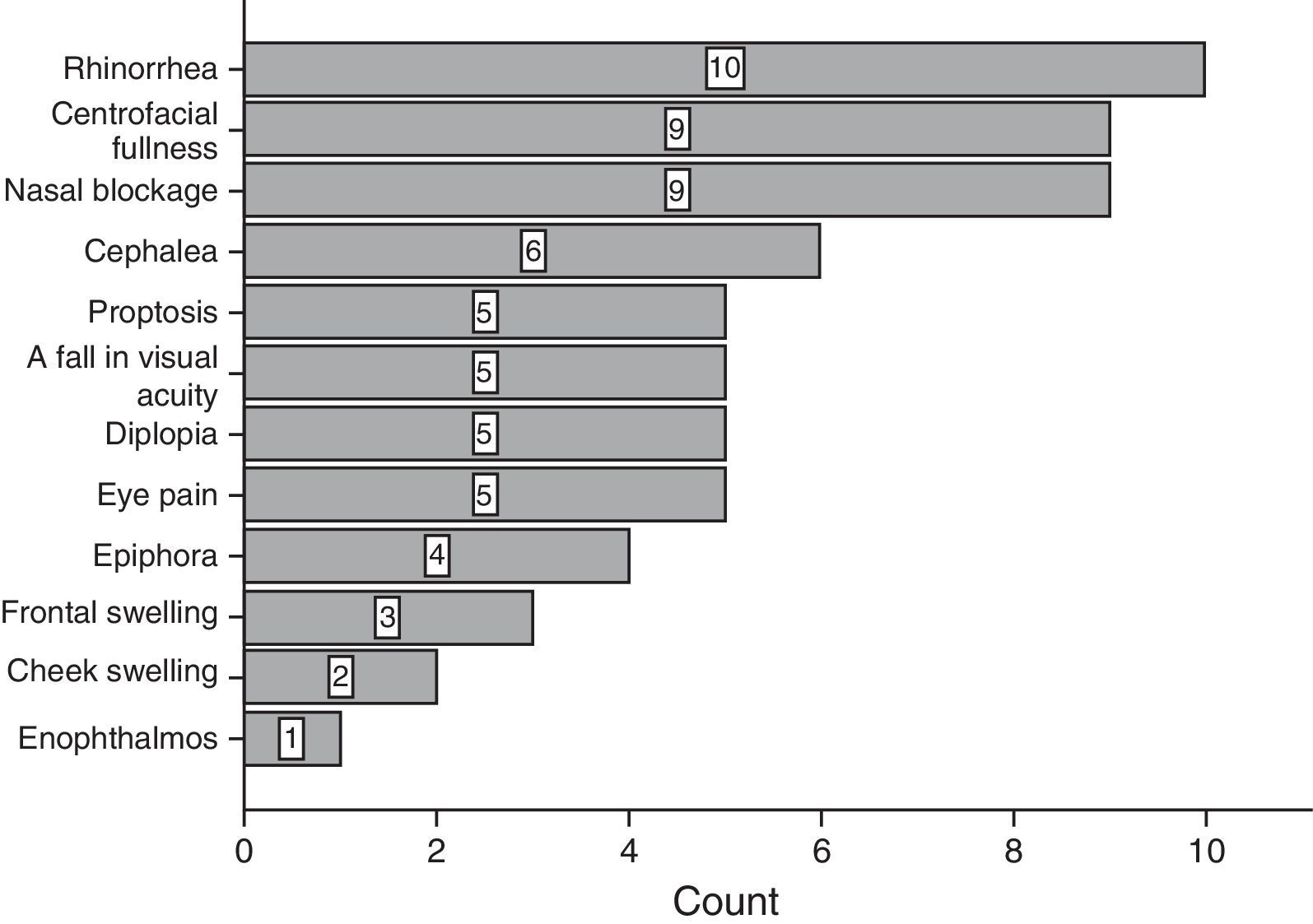
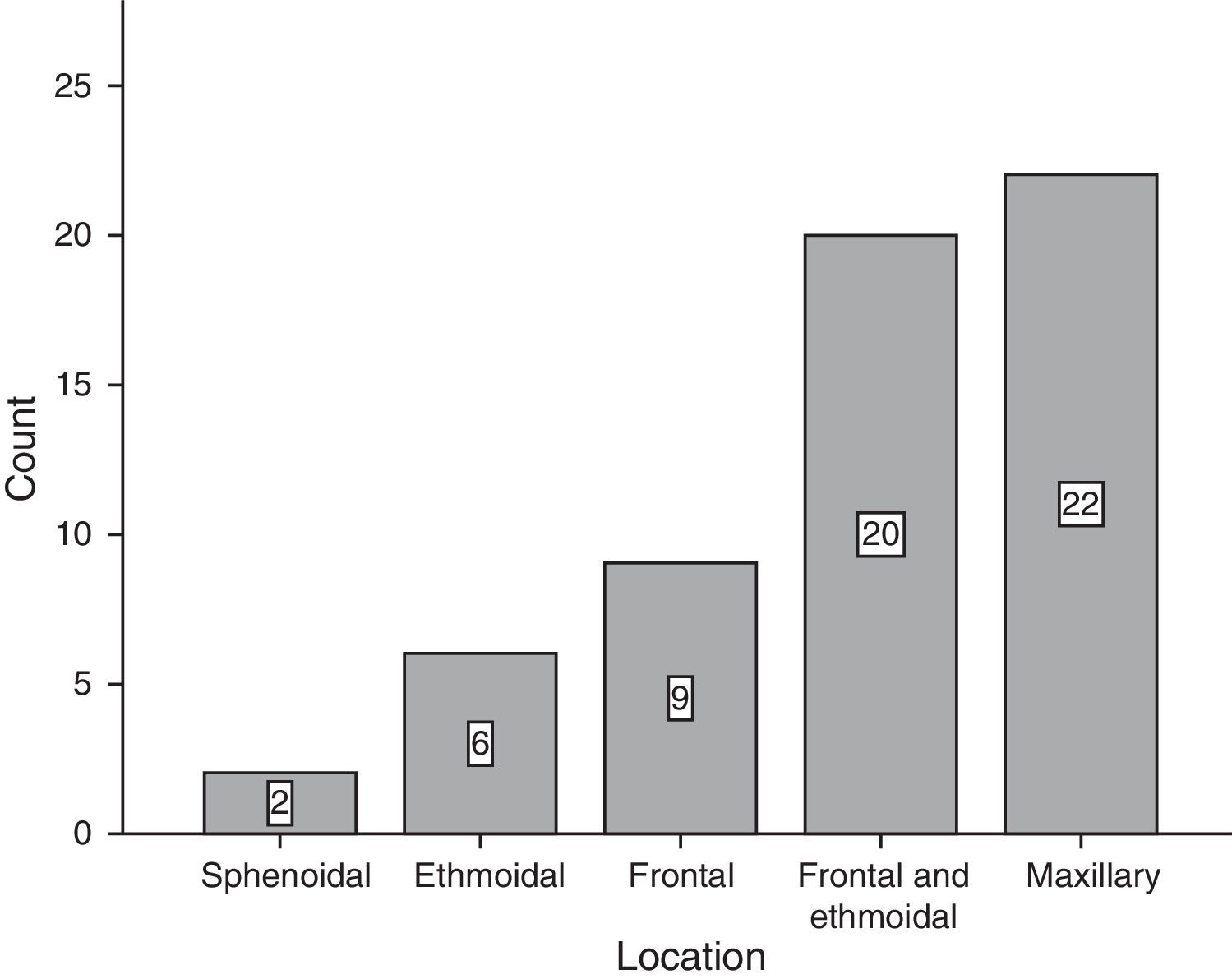
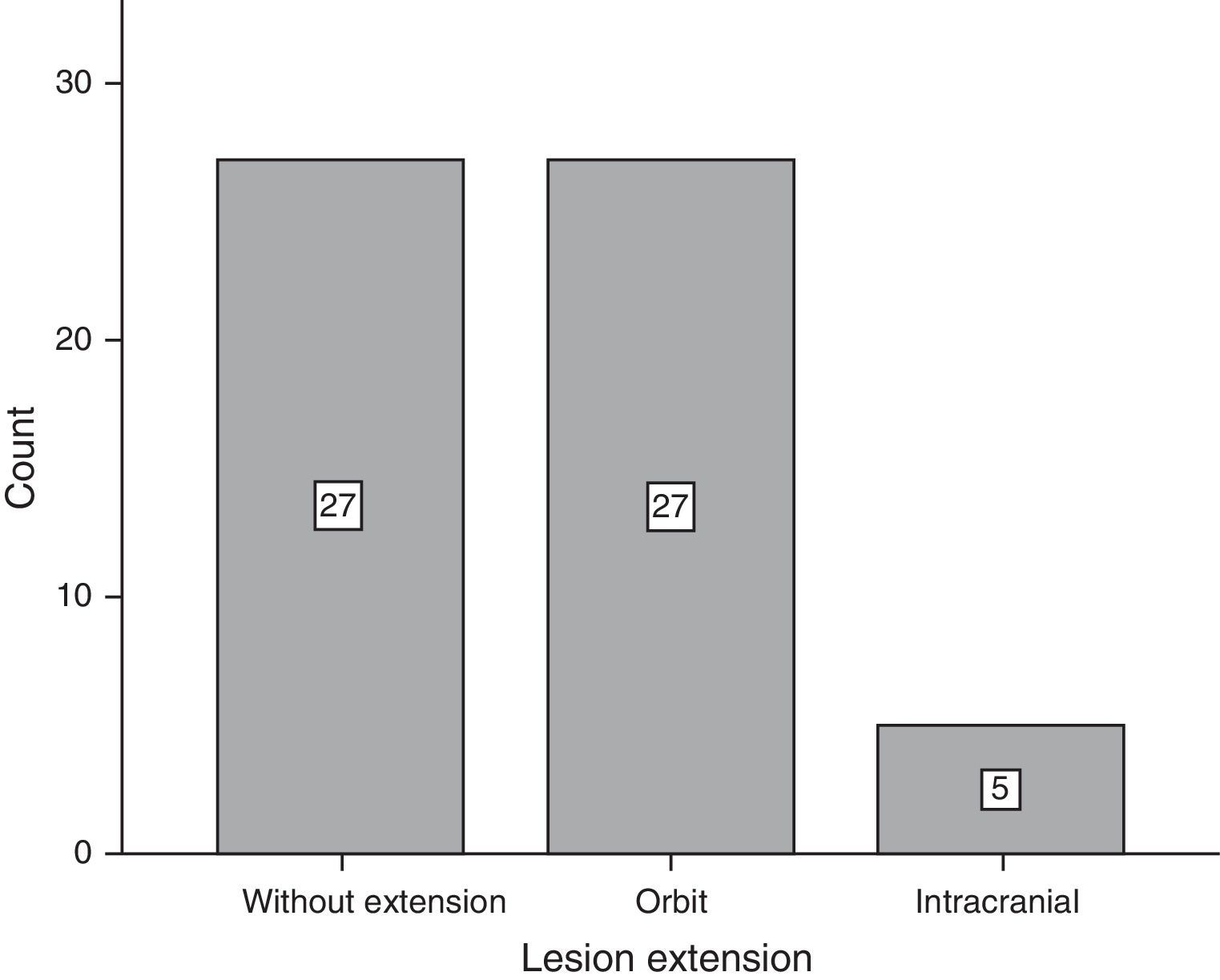
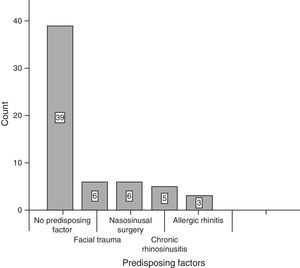
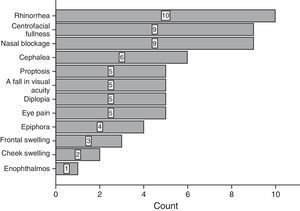
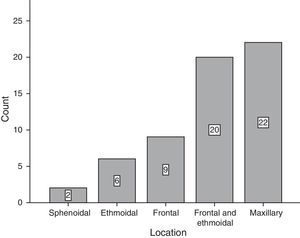
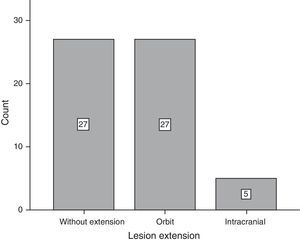
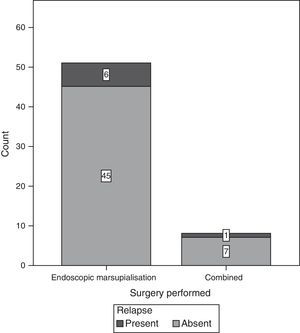
ResultsOf the total of 59 patients, 39 were female and the rest were male. The most common age group was 30–39 years old and 40–49 years old, with 6 patients each. For the majority of patients, 39 of 59, no predisposing factor for the development of a mucocele was found. The most common factors were facial trauma, allergic rhinitis and chronic rhinosinusitis, at 10.17% for each factor (Fig. 1). The most frequent form of clinical presentation was rhinorrhea, with 10 cases (15.63%), followed by nasal blockage and centrofacial fullness, with 9 cases (14.06%) for each one, while cephalea was in fourth place with 6 cases (9.38%) (Fig. 2). Respecting the time during which symptoms developed, the most frequent period was the range of less than 3 months, followed by 12–24 months, 6–12 months and 3–6 months, respectively. The most common location of the mucocele was in the maxillary sinus (22 patients), followed by frontoethmoidal involvement (20 patients) (Fig. 3). The least frequent extension was intracranial, with only 5 cases (8.47%), while 27 patients (45.76%) had extension into the orbit and 27 (45.76%) had exclusively sinusal involvement (Fig. 4). Of the 59 patients who were treated using a surgical procedure, 8 (9%) presented relapse of the lesion. Regarding the type of surgical procedure used, no open surgery was performed and only endoscopic technique was used (51 patients) or combined technique (8 patients); 7 of the 51 patients operated endoscopically relapsed, as did 1 of the 8 patients treated using a combined technique. These data correspond to 13.7% and 12.5%, respectively (Fig. 5).
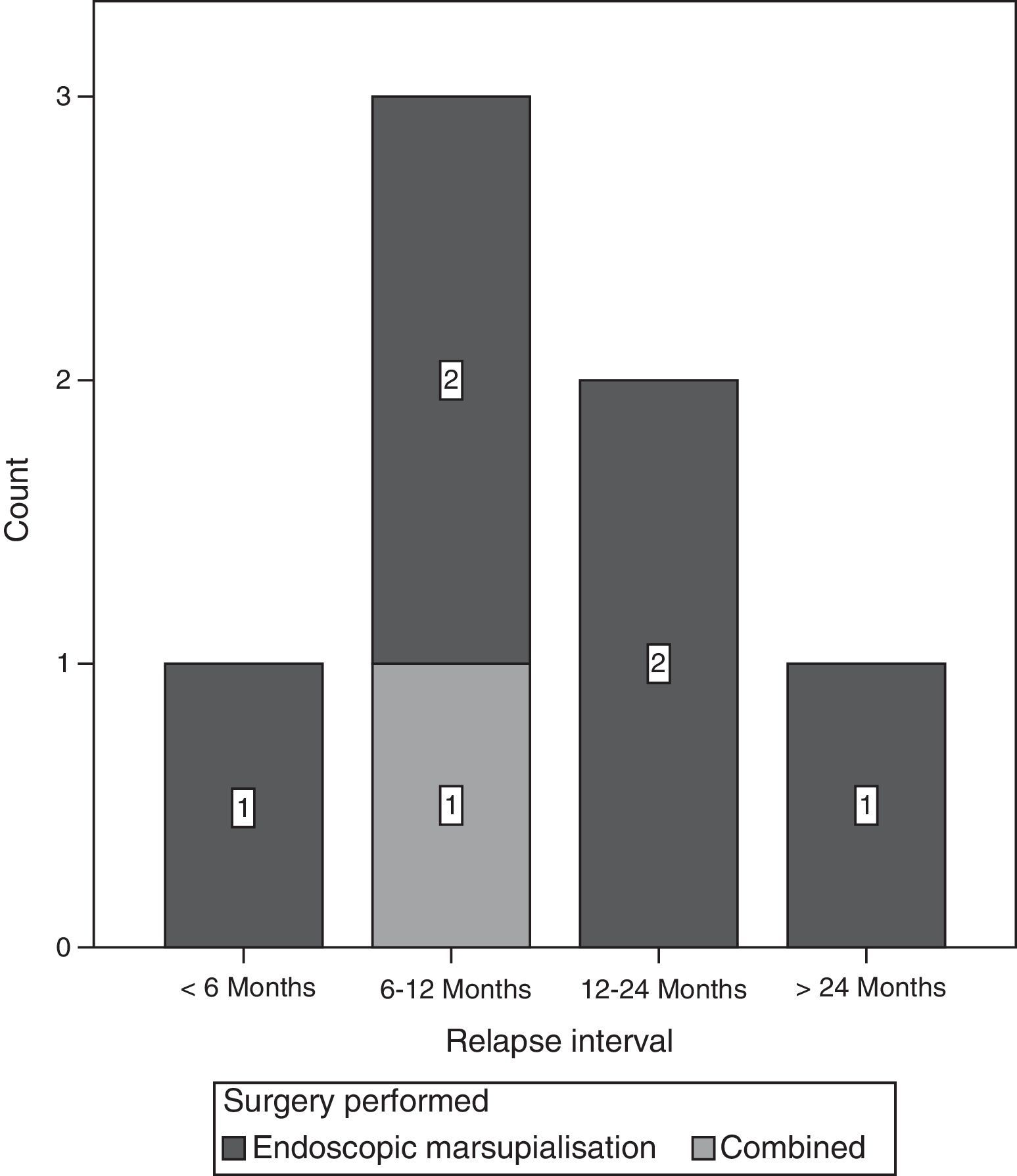
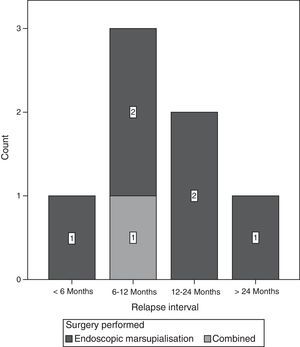
The most frequent time interval to relapse of the lesion was from 6 to 12 months after surgery (Fig. 6).
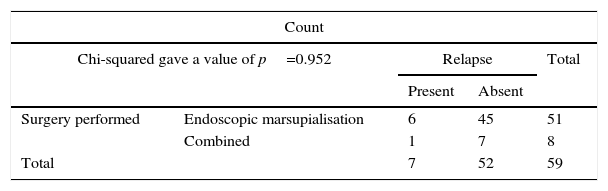
Statistical analysis. The association between the type of surgery performed and relapse was determined with a value of χ2=0.004, and a p value of 0.952, without being statistically significant.
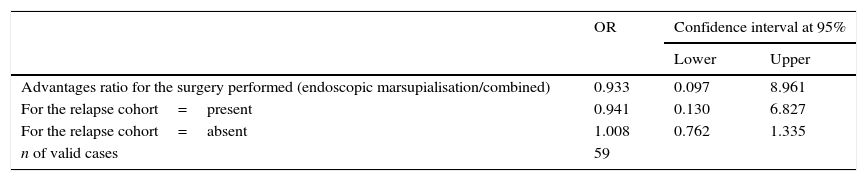
As the study design was transversal, risk was calculated using the odds ratio [OR], giving a value of OR=0.933, with a confidence interval of 0.097–8.961, going above the unit (Table 1).
The association (by χ2 mean) between the type of surgery performed and the presence of relapse. No statistically significant association was detected.
| Count | ||||
|---|---|---|---|---|
| Chi-squared gave a value of p=0.952 | Relapse | Total | ||
| Present | Absent | |||
| Surgery performed | Endoscopic marsupialisation | 6 | 45 | 51 |
| Combined | 1 | 7 | 8 | |
| Total | 7 | 52 | 59 | |
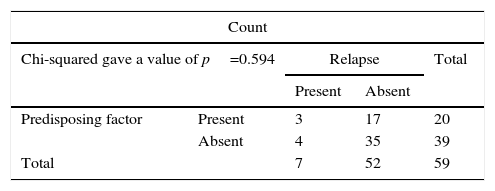
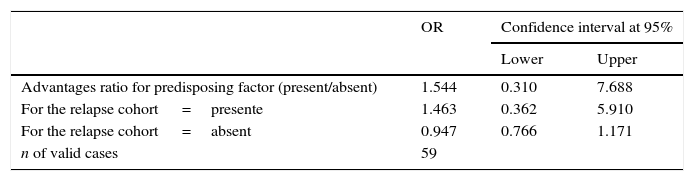
The association of the presence or absence of the predisposing factor with relapse was determined by univariate statistics, with a value of χ2=0.284 and a p value of 0.594.
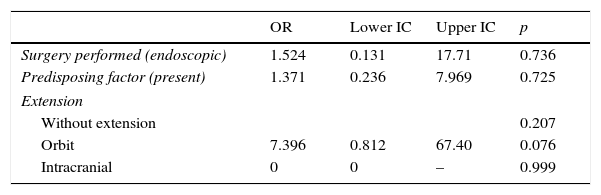
Risk was calculated by means of the odds ratio (OR), giving a value of OR=1.544, with a confidence interval of from 0.310 to 7.688, going above the unit (Table 2). Multivariate analysis was performed by means of logistic regression with a model that included the type of surgery performed, the presence of a predisposing factor and the extent of the lesion. Using this analysis no statistically significant association was found with the dependent variable (relapse) or the independent variables included (Table 3).
The association (by chi-squared mean) between the presence of a predisposing factor and the presence of relapse. No statistically significant association was detected.
| Count | ||||
|---|---|---|---|---|
| Chi-squared gave a value of p=0.594 | Relapse | Total | ||
| Present | Absent | |||
| Predisposing factor | Present | 3 | 17 | 20 |
| Absent | 4 | 35 | 39 | |
| Total | 7 | 52 | 59 | |
The literature describes several series where the majority of cases treated endoscopically show a relapse rate that varies from 0.9% to 2.2%; in other studies with fewer patients this relapse rate rises to from 11% to 13% of cases.6 The aim of this study is to determine the possible association between the type of surgery performed and lesion recurrence. The hypothesis was that endoscopic surgery would give rise to a lower rate of complications and relapse in comparison with open surgery; however, none of the patients evaluated in the analysis was subjected to open surgery, as they were treated using only endoscopic marsupialisation or combined surgery.
The study analysed 64 patients with a diagnosis of mucocele for possible inclusion from 2006 to 2013. Of these, 59 patients fulfilled the selection criteria. 5 patients were excluded because their transoperative findings did not confirm the diagnosis made prior to surgery. Of these, 3 cases were mycotic rhinitis (fungal bolus), with one chronic rhinositis with polyps and one verrucous tumour (Tables 4 and 5).
Logistic regression: dependent variable (relapse).
| OR | Lower IC | Upper IC | p | |
|---|---|---|---|---|
| Surgery performed (endoscopic) | 1.524 | 0.131 | 17.71 | 0.736 |
| Predisposing factor (present) | 1.371 | 0.236 | 7.969 | 0.725 |
| Extension | ||||
| Without extension | 0.207 | |||
| Orbit | 7.396 | 0.812 | 67.40 | 0.076 |
| Intracranial | 0 | 0 | – | 0.999 |
No statistically significant association was found between any risk factor and relapse. There is a tendency towards association between extension into the orbit and relapse (p=0.076) although this is not statistically significant.
In our study the mucocele relapse rate amounted to 9% of our population. 13.7% of this total percentage of relapse corresponded to the group treated with an endoscopic approach; nevertheless, no significant association was found between our variables. It would therefore not be fully correct to state that there is no association between the type of surgery and lesion relapse, given that it is important to mention that the said results may be distorted by certain intrinsic aspects of the study. One example of this is that only 2 types of surgery were performed, and that of these 2 the vast majority (51 of the 59 cases) were endoscopic. This places the other (combined) technique at a disadvantage and thereby prevents the detection of any possible significant association, even if there really is one. The ideal and recommendable situation in studies of this type is for there to be a balance between the number of techniques performed.
In the literature reports of frontoethmoidal involvement predominate (60–80%), followed by maxillary (10%) and sphenoidal involvement (6–11%). In our study, on the contrary, there were more cases of maxillary sinus involvement (37%) followed by frontoethmoidal involvement (33.9%). In the bibliography consulted the factors associated with the predominance of a maxillary sinus location are found in Japan, where they all appeared after the Caldwell-Luc procedure, although this relationship was not found in our study.6
Many theories exist regarding the origin and development of paranasal sinus mucoceles, including: chronic rhinosinusitis, allergic rhinitis, trauma and previous surgery. In our study 54% of patients had no predisposing factor, and this is comparable to what is described in the literature.4 Regarding the future, this study marks the start of a line of research in which it is planned to undertake new studies with larger balanced populations, with a different methodological design. Ideally they will be multicentre studies that will make it possible to determine with greater precision and exactitude any possible association between the variables studied.
ConclusionsThe majority of patients were treated by endoscopic surgery, and no patient was treated using open surgery. There was relapse of the mucocele in 9% of the population. No statistically significant association was found between the type of surgery and relapse. Nor was any significant association shown to exist between the presence or absence of a predisposing factor and relapse.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflict of interestsThe authors have no conflict of interests to declare.
The authors would like to thank Dr. C. José Waizel and the editors of the journal for their opinions and suggestions arising from reading this manuscript.
Please cite this article as: Waizel-Haiat S, Díaz-Lara IM, Vargas-Aguayo AM, Santiago-Cordova JL. Experiencia en el tratamiento quirúrgico de mucoceles de senos paranasales en un hospital universitario. Cir Cir. 2017;85:4–11.