The first reported case of intestinal perforation secondary to metastatic lung carcinoma was reported in 1957. Intestinal metastases are present in up to 1.8% of the cases, with small bowel obstruction as the most common clinical presentation.
Clinical caseAn 89 year-old male, who was diagnosed with a high-grade pulmonary mucoepidermoid tumour 2 months previously. The patient was admitted to the hospital for 3 days due to diffuse colic abdominal pain of moderate to severe intensity, accompanied by nausea and gastric vomiting, as well as 2 episodes of bloody bowel movements. On physical examination, the patient was noted to have tachycardia and tachypnoea, as well as clinical signs of acute abdomen. He had white cells of 24,900 per mm3, and 87% neutrophils. Exploratory laparotomy was performed, which showed a bowel perforation associated with a tumour mass 15cm beyond the angle of Treitz. Bowel resection and primary anastomosis were performed. The histopathological analysis reported the diagnosis of a high-grade mucoepidermoid tumour with small bowel and mesentery with disease-free surgical margins. Unfortunately the patient had a fatal outcome secondary to hospital-acquired pneumonia.
ConclusionThe cases of metastases to small bowel are extremely rare, and to our knowledge this is first case reported in Mexico. The patient described went to the emergency room with gastrointestinal bleed and intestinal perforation that required urgent surgical intervention with small bowel resection and primary anastomosis. Unfortunately the patient died secondary to hospital acquired pneumonia.
El primer caso de perforación intestinal por metástasis de cáncer pulmonar, fue reportado en 1957. Las metástasis intestinales se reportan hasta en el 1.8% de los casos. La presentación clínica más frecuente es la obstrucción intestinal.
Caso clínicoPaciente masculino de 89 años de edad, con antecedente de carcinoma mucoepidermoide de pulmón de alto grado, de 2 meses de diagnóstico. Acude al hospital con cuadro clínico de 3 días de evolución, con dolor abdominal de tipo cólico, difuso, de moderada a severa intensidad, acompañado de náuseas y vómito de contenido gastrobiliar y evacuaciones melénicas en 2 ocasiones. A la exploración física se encuentra: taquicárdico, taquipneico y con datos de abdomen agudo. Reporte de laboratorio: leucocitos 24,900 células por mm3, neutrófilos 87%. Se realizó laparotomía exploradora, encontrándose tumor perforado a 15cm del ángulo de Treitz. Se realizó resección intestinal y anastomosis primaria. Reporte histopatológico de carcinoma mucoepidermoide de alto grado, intestino delgado y mesenterio con límites quirúrgicos sin neoplasia. El paciente tuvo mala evolución por desarrollar neumonía nosocomial, lo que resultó en su fallecimiento.
ConclusiónSon pocos los casos de metástasis intestinal reportados a nivel mundial; en México este es el primer caso reportado. Clínicamente se manifestó con sangrado de tubo digestivo y perforación intestinal que requirió cirugía de urgencia, en la que se realizó resección intestinal con anastomosis primaria. Finalmente, el paciente falleció por neumonía nosocomial.
Lung cancer is the main cancer diagnosed in males, comprising 17% of the total number of new cancer cases and 29% of total cancer deaths. It is the fourth cancer diagnosed in females and in second place as a cause of death. Currently 50% present with metastatic disease at time of diagnosis, leaving no possibility of curative treatment.1,2 The main histological types include adenocarcinoma, squamous cell, small cell and large cell. Extra-thoracic metastases can present in advanced stages of lung cancer, the most frequent sites are: liver, adrenal glands, bone and brain. Gastrointestinal metastases are rare and include: stomach, small bowel, appendix, colon and anus.3,4
Bowel metastases are reported in up to 1.8% of lung cancer cases, which makes them rare. However, post mortem examinations (autopsies) on patients with lung cancer, show that they are not uncommon at a prevalence of 4.7–14%. Lung cancer metastases to the small bowel can manifest clinically as bleeding, obstruction or perforation.3–7 Occasionally bowel perforation can be due to the use of chemotherapy, as a result of necrosis in the tumour, in patients receiving palliative care for lung cancer.5
The first case of bowel perforation secondary to lung cancer metastasis was reported in 1957 by DeCastro et al.8
The treatment of choice is intestinal resection with primary anastomosis. However a perioperative mortality of 60% to 100% is reported.5
ObjectiveTo describe a rare case of jejunal perforation secondary to mucoepidermoid carcinoma of the lung.
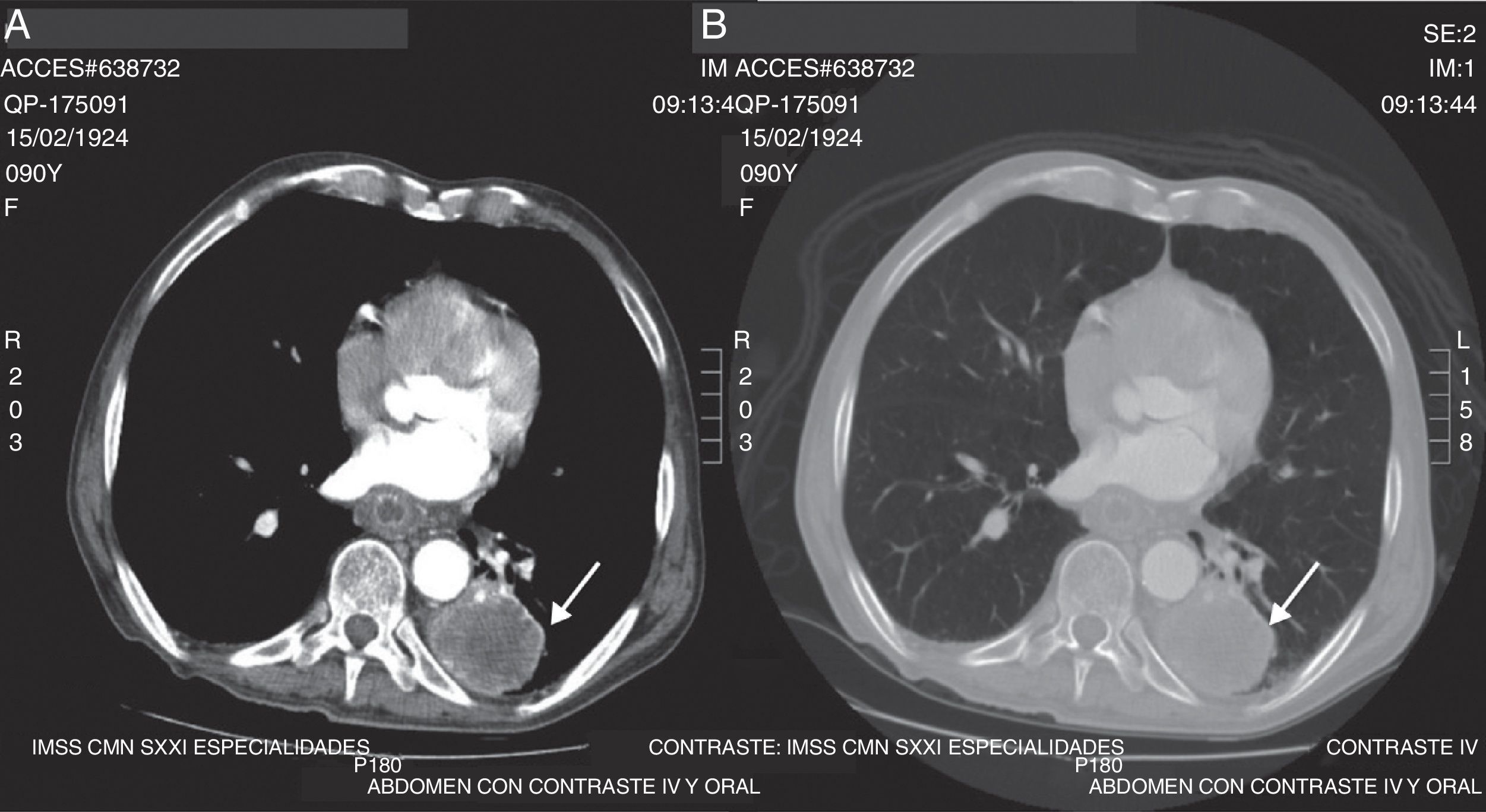
Clinical caseAn 89-year-old male patient with a history of tobacco use, smoking 183 packets per year, chronic obstructive pulmonary disease diagnosed 8 years previously and treated with salbutamol, budesonide and supplemental oxygen at 3l/min for 16h a day, aortoiliac aneurysm and high-grade mucoepidermoid carcinoma T2 N0 M0, clinical stage IB, diagnosed 2 months previously (Fig. 1).
Tomography of the chest with intravenous contrast. (A) Axial slice showing a lesion occupying the left base of approximately 47×44×103mm (arrow), hypodense, heterogeneous, with average attenuation values of 5–80 UH, with well-defined edges, which after administration of the contrast medium, shows peripheral enhancement. (B) Axial slice with lung window that shows the same lesion (arrow), with no evidence of other lesions in the lung parenchyma.
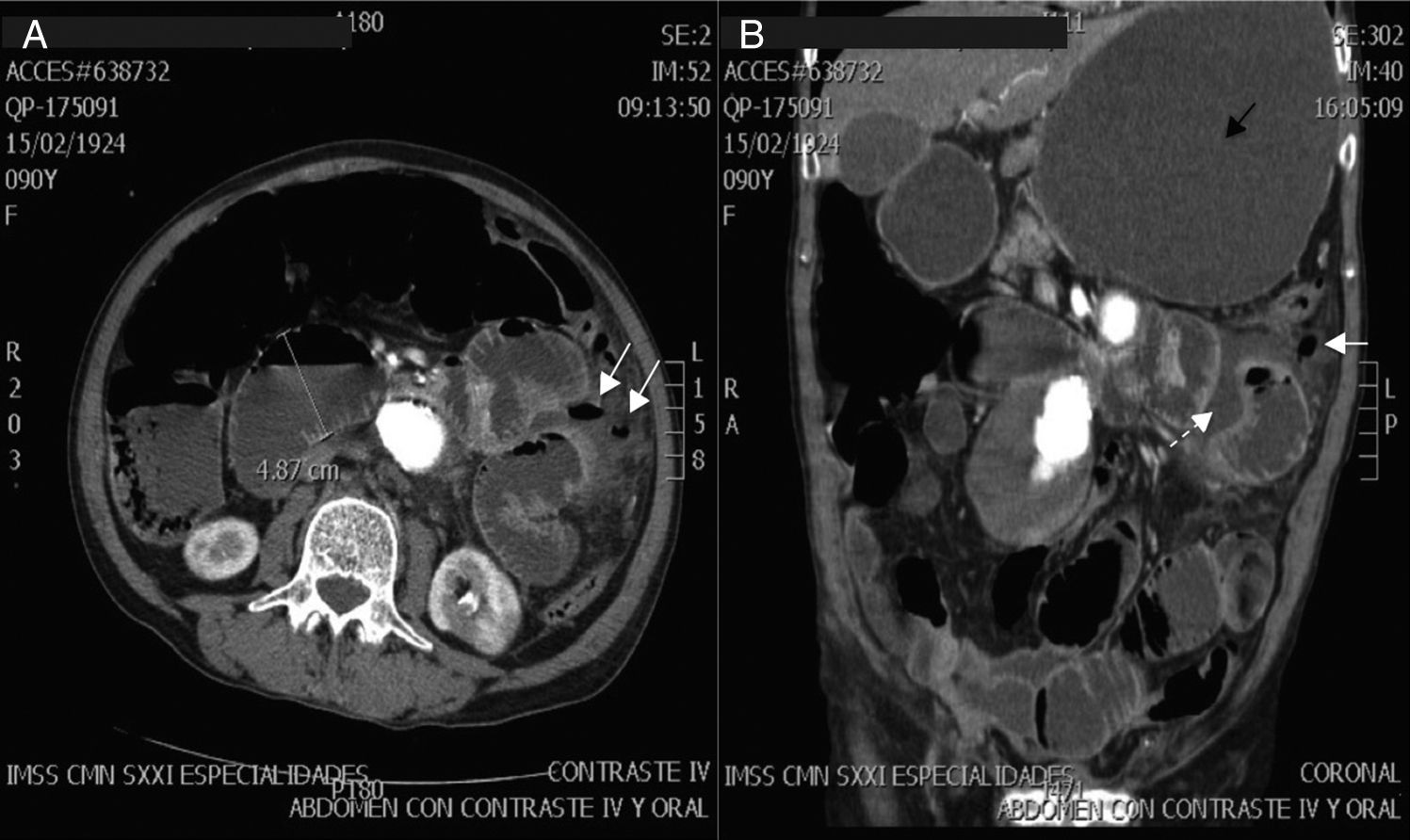
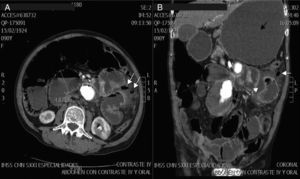
The patient was admitted to hospital with a 3-day history of symptoms including colicky abdominal pain located in all of the abdominal quadrants, of moderate to severe intensity, accompanied by abdominal distension, nausea and vomiting of gastro-biliary content on several occasions, added to which subsequently were two episodes of melena stools. On physical examination the patient was found to be in a poor general condition, dehydrated, tegument pallor, hyperthermia 38.1°C, tachypnoea at a rate of 28 respirations per minute, left baseline hypoventilation, tachycardia of 110 beats per minute, blood pressure 100/60mmHg, distended abdomen, with involuntary muscular resistance, rebound tenderness (Blumberg's sign), tympanic on percussion in all quadrants, diminished peristalsis, hypotrophic upper and lower extremities. The laboratory tests showed: glucose 129mg/dl, urea 78mg/dl, creatinine 1mg/dl, haemoglobin 13.1g/dl, leukocytes 24,900 cells per mm3, neutrophils 87%, prothrombin time 16.9s, partial thromboplastin time 30.3s. Simple abdominal X-ray revealed dilation of the small bowel loops, and ground glass opacity on the area of the left hypochondrium and flank (Fig. 2). Abdominal CAT scan with intravenous contrast, showed dilation of the stomach and small bowel loops, and proximal small bowel cluster with the presence of air corpuscles outside the loops and peripheral free fluid. An uncomplicated abdominal aortic aneurysm 63mm×68mm was also observed (Fig. 3).
Abdominal tomography with intravenous contrast. (A) Axial slice with findings of dilation of small bowel loops greater than 3cm, and air corpuscles located outside the intestinal lumen (arrows). (B) Coronal slice with major gastric dilatation (black arrow), free air (continuous white arrow) and free fluid in the cavity (dashed white arrow).
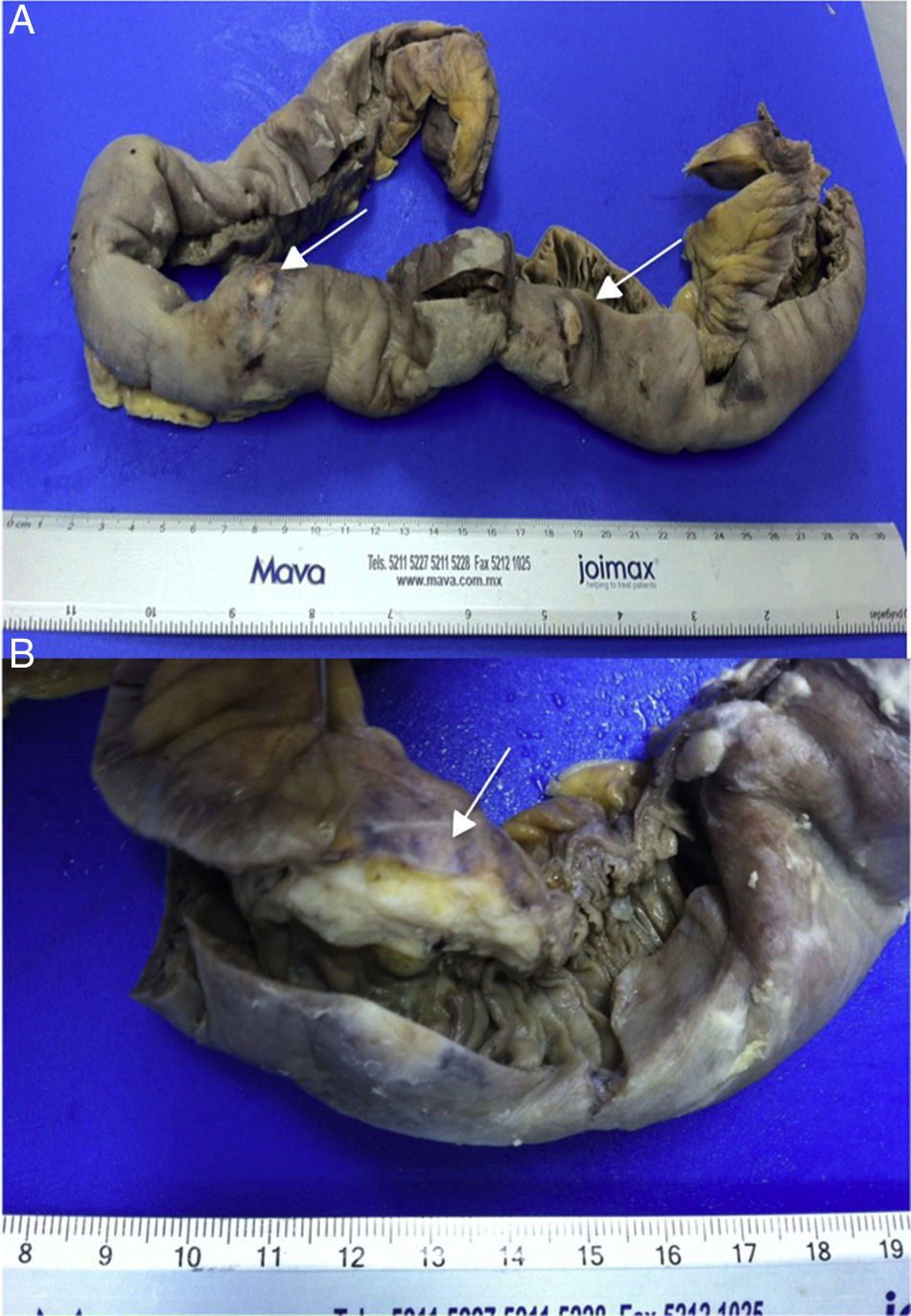
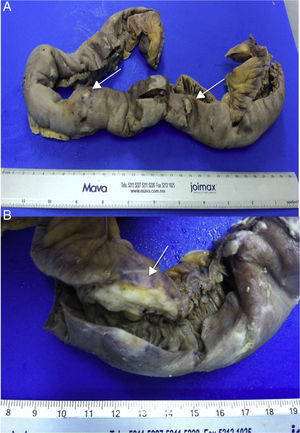
An exploratory laparotomy was performed and a tumour found of approximately 1.5cm, perforated 15cm from the angle of Treitz, and other lesions at 20, 50 and 80cm from the fixed loop and therefore an intestinal resection of the segment containing the 4 lesions was performed and manual end-to-end, side-to-side anastomosis on 2 planes. The histopathological report concluded: small bowel segment 60cm×3cm, serous membrane 2cm not intact located 1.2cm from the larger surgical margin and 4 white nodular lesions and greenish white plaques adhering to the surface, 4 ulcerated lesions were found on making the cut, the largest 2.5cm in diameter, white with irregular edges. High-grade mucoepidermoid carcinoma was diagnosed in the small bowel and mesenterium with cancer-free surgical margins (Fig. 4). After surgery, the patient made good progress abdominally, was kept on nil by mouth for 5 days, there were no signs of anastomotic leak, and therefore a liquid diet was started, which was well tolerated. However, he developed pneumonia and died on the tenth post-operative day.
DiscussionThe prevalence of intestinal metastases from lung cancer is 0.17–10.7%, according to the case series reported in the literature.7–9 There has been no meta-analysis to date to define the prevalence, because of the lack of homogeneity of inclusion criteria and because most reviews are case reports. At present, only Jian-Zhong Di et al.10 in 2014 have published a general prevalence of 7.1% by including a review of 100 cases. Metastases are more common in men, at 76%, compared to women.
By the time lung cancer is diagnosed, almost half the patients are inoperable. This is due to the presence of metastasis. It has been demonstrated from autopsies that intestinal metastases are not so rare, but it is rare for metastases to manifest clinically.9 When intestinal metastases become symptomatic, they can present various clinical scenarios such as, abdominal pain, obstruction, intestinal perforation, bleeding from the digestive tract, intussusception or, very rarely, a combination of all symptoms.5,7,9,10
In the literature, the clinical scenario of intestinal obstruction is described as the most common presentation4,5; however, other reviews report abdominal pain as the most frequent symptom.10 With the heterogeneous definition of the clinical symptoms, it is difficult to establish their frequency. In the largest review, of 100 cases, abdominal pain due to intestinal perforation is established as the most common symptom at 46%.10
Of all the scenarios described, intestinal perforation presents the highest morbidity and mortality11; if there is no intestinal perforation survival increases significantly.12 In this case, the patient not only presented acute abdomen secondary to intestinal perforation by an intestinal lung cancer metastasis, but also presented signs of bleeding from the upper digestive tract (melena). It is the combination of these 2 clinical manifestations that makes this case so rare.
The route of spread remains unclear. The most widely accepted proposal is haematogenous dissemination, however lymphatic dissemination is also considered.9,10
The ileum is the anatomic segment of small bowel that is most commonly affected by lung cancer metastasis, followed by the jejunum and finally the duodenum.5,9 The most frequently identified histology is non-small cell carcinoma a squamous cell subtype.3,5,9,10 After the literature review, in this patient we also identified that the site of perforation was rare. This was the jejunum and the histology report showed non-small cells (the most frequently reported); however, the mucoepidermoid variety is very rare. And what is more, the study of 100 cases published by Jian-Zhong Di et al.10 in 2014 did not report a single case.
The procedure of choice for symptomatic intestinal metastases is resection of the segment with the lesions, followed by a primary anastomosis. This can even be performed to prevent any of the complications such as perforation, obstruction or bleeding, however, prophylactic resection remains contraversial.5,10 The prognosis of patients with intestinal metastases from lung cancer is very poor.9 Perioperative mortality varies from 60% to 100%.5 The overall survival of patients with lung cancer and intestinal metastasis is poor, with a mean survival of 2.3 months.10
Perioperative complications due to lung cancer intestinal metastases include: severe infection and respiratory failure.3,13,14 In our case, when the patient presented with an acute abdomen, he require emergency surgery, in which the perforated section affected by the lung cancer metastasis was resected followed by a primary anastomosis. However, he did not make good progress during the postoperative period and developed nosocomial pneumonia resulting in his death. A classification has recently been created for postoperative complications termed the Clavien-Dindo15 grading system comprising 5 grades: grade V is the death of the patient, as in our case.
ConclusionIntestinal metastases caused by lung cancer are very uncommon and rarely manifest clinically, but when they do the morbidity and mortality rate is usually very high.
This is the first case reported in Mexico of intestinal perforation by mucoepidermoid lung cancer. The features that made the case so rare were that it presented with 2 clinical manifestations (bleeding from the digestive tract and intestinal perforation) and the histological type (mucoepidermoid cancer of the lung). The treatment of choice was performed, with intestinal resection and primary anastomosis, although ultimately the patient died from a postoperative complication of lower respiratory tract infection. Although clinically considered a rare entity, post mortem studies show a higher incidence, therefore it should be taken into account in the differential diagnosis of future cases in order to prevent future complications. The presence of intestinal metastases in patients with lung cancer should be considered, and once they have been identified the affected segment of the intestine should be resected prophylactically.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Moreno-Aguilera E, Galeana-Nogueda FI, Vera-Aguilera J, Vera-Aguilera C, Ley-Marcial LA. Perforación yeyunal secundaria a metástasis de carcinoma mucoepidermoide pulmonar. Reporte de caso y revisión de la literatura. Cir Cir. 2017;85:254–259.