An alternative treatment for obstructive and refluxing obstructive megaureter with ureterovesical junction maintenance through laparoscopy is proposed.
Material and methodsThe series consists of 8 cases, all of them studied because of prenatal hydronephrosis or febrile urinary tract infection. Seven were diagnosed with obstructive megaureter and one with obstructive refluxing megaureter. The procedure consisted in incising the stenotic portion of the ureter longitudinally and maintaining its posterior wall attached to the bladder, the anterior wall of the ureter was anastomosed transversally to the bladder mucosa in order to liberate the obstruction.
ResultsTwo of the 8 cases were women and 6 were male. They were aged between 5 months and 11 years (average age of 2.9 years). The surgical time varied between 90 and 120min, with a 48h hospital stay. The permanence of the vesical catheter and the double J stent was of 48h and 6 weeks, respectively. A female patient developed febrile urinary tract infection one week after the surgical procedure. The rest of the patients remained asymptomatic, with normal urinalysis and quarterly urine culture results.
Six months after the procedure, the ultrasound showed improvement of the ureteral diameter and of the pyelocaliceal ectasia. The average follow-up was of 2 years.
DiscussionThe handling of stenosis with longitudinal incision of the ureter and transverse anastomosis to the bladder mucosa, seems promising. The laparoscopic approach allows to identify clearly the longitude of the stenotic segment and join with relative precision such opening with the one of the vesical mucosa.
Se propone una alternativa de tratamiento del megauréter obstructivo y obstructivo refluyente sin desinserción ureteral por laparoscopia.
Material y métodosLa serie consta de 8 casos, todos ellos estudiados por hidronefrosis prenatal o infección urinaria febril. Siete tuvieron megauréter obstructivo y uno megauréter obstructivo refluyente. La plastia ureterovesical laparoscópica consistió en incidir longitudinalmente la porción estenótica del uréter y mantener la pared posterior del mismo unida a la vejiga. Luego se anastomosó la pared anterior del uréter abierto a la mucosa vesical en sentido transversal con el objeto de liberar la obstrucción.
ResultadosDe los 8 casos, 2 eran mujeres y 6 hombres, de entre 5 meses y 11 años de edad (promedio de 2.9 años). El tiempo quirúrgico varió de 90 a 120min, con una estancia hospitalaria de 48h. La permanencia de la sonda vesical y la del catéter doble «J» fueron de 48h y de 6 semanas, respectivamente. Una paciente desarrolló infección urinaria febril a la semana del procedimiento quirúrgico. El resto se mantuvieron asintomáticos urinarios, con examen general de orina y urocultivo trimestrales normales.
El ultrasonido al sexto mes mostró mejoría del diámetro ureteral y de la ectasia pielocaliceal. El seguimiento promedio fue de 2 años.
DiscusiónEl manejo de la estenosis con incisión longitudinal sin desinserción del uréter y con anastomosis transversal a la mucosa vesical podría ser prometedor. El abordaje laparoscópico permite identificar claramente la longitud del segmento estenótico y empatar con relativa exactitud dicha apertura con la de la mucosa vesical.
Stenosis of the ureterovesical junction (SUJ) is an obstructive disorder of the distal ureter at the inlet to the bladder resulting in megaureter. A dilated ureter greater than 7mm in diameter with or without concomitant pyelocaliceal dilation is known as megaureter. In 1976 an international paediatric urology seminar in Philadelphia classified megaureter into refluxing, obstructed,and non-refluxing non-obstructed.1,2 In 1980 King amended this classification adding a fourth group, the refluxing obstructed megaureter.3
Although there are reports of minimally invasive procedures for treating megaureter, including inserting a stent at the stenotic site, implanting a double J stent, and then balloon dilation the length of the narrow ureter and endoureterotomy, continuous surgical reconstruction being the most recommended procedure. This procedure traditionally involves vesical disinsertion of the ureter, excision of the site of the obstruction and then afterwards, only if the diameter exceeds one centimetre, ureteral plication or reduction in order to ensure the sufficiency of the reimplant in the bladder.4–6
We propose a celioscopic treatment alternative for obstructive and refluxing obstructive megaureter, preserving the ureterovesical junction in cases where it is necessary to reduce the diameter of the ureter.
Material and methodsDuring the period between October 2010 and March 2015, 8 patients with a history of prenatal hydronephrosis or urinary tract infection with a fever ≥38°C, fetid urine, haematuria, dysuria and impaired general health were explored by urinary tract ultrasound, cystouretrogram, excretory urography and diuretic renal gammagraphy MAG 3.
Seven patients were diagnosed with obstructive megaureter, and one patient had right-sided refluxing obstructive megaureter and grade IV contralateral vesicoureteral reflux.
One of the female patients with a prenatal diagnosis of megaureter presented a febrile urinary tract infection at 4 months old and one month later underwent right-sided endoscopic ureterovesical dilation and a double J stent was inserted, with no improvement on the ultrasound. Moreover, during follow-up the child continued to have urinary infection symptoms, so she was operated in the same way as the other 7 patients with the procedure described below.
Description of surgical techniqueA celioscopic approach was used with subxiphoid or umbilical optics according to the age of the patient and 2 ports at the sides of the rectus abdominis muscle of 3–5mm.
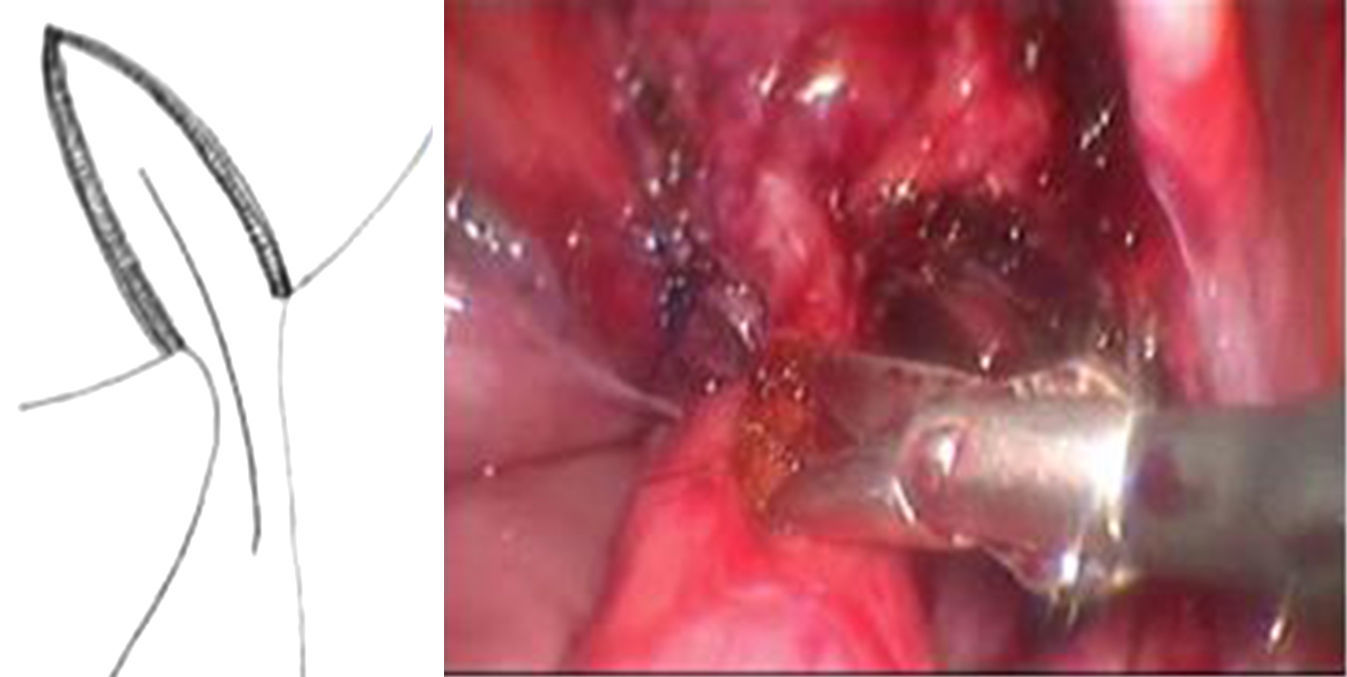
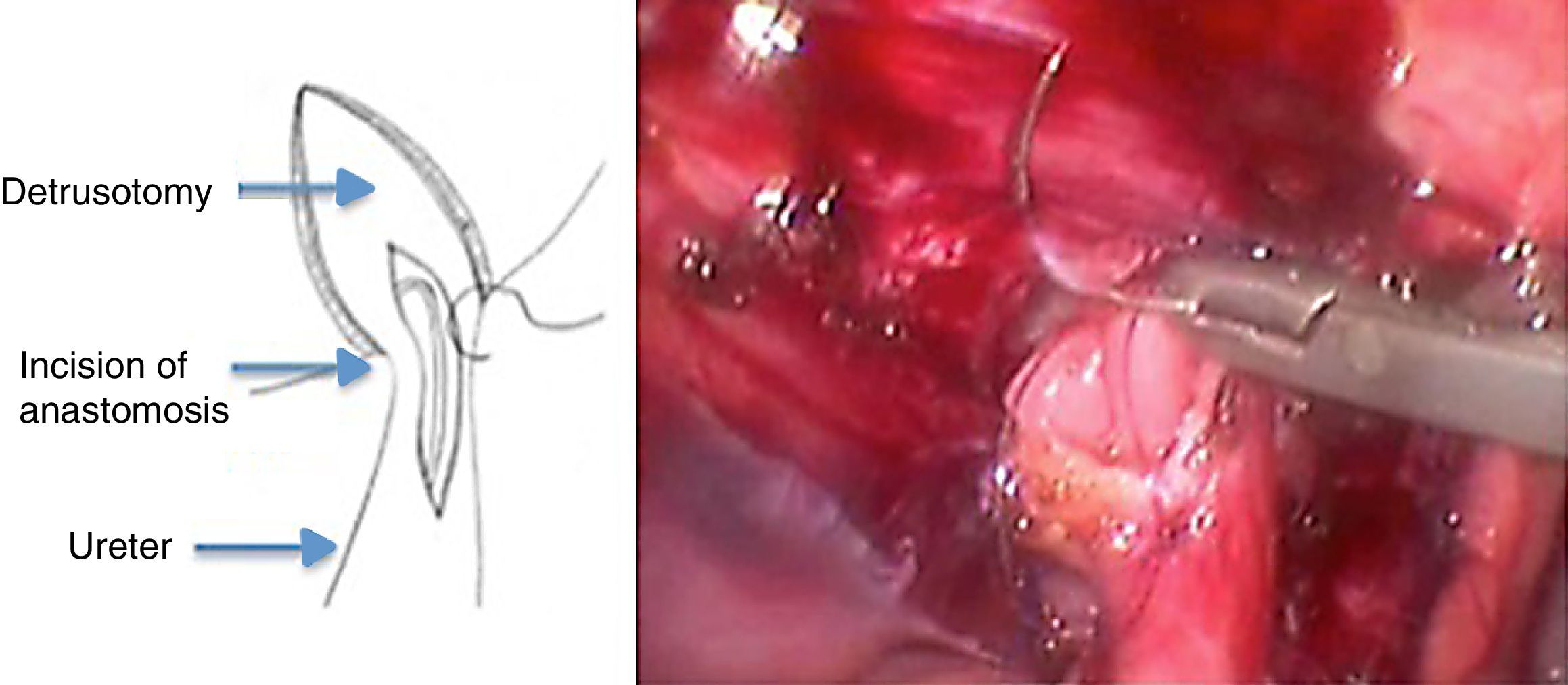
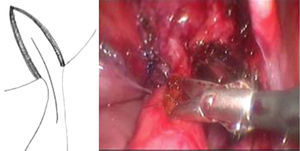
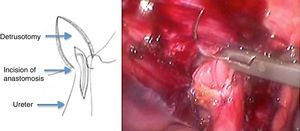
A detrusotomy of a length proportional to the diameter of the ureter up to the ureterovesical junction was made. Once the mucosa had herniated a longitudinal incision was made that included the beginning of the dilated ureteral segment dilated in its anterior half, then the area of stenosis and finally the adjacent vesical mucosa. The length of the cut of the ureterovesical junction was enough to resolve the obstruction when the anastomosis of the ureter to the vesical mucosa was performed transversally (Fig. 1).
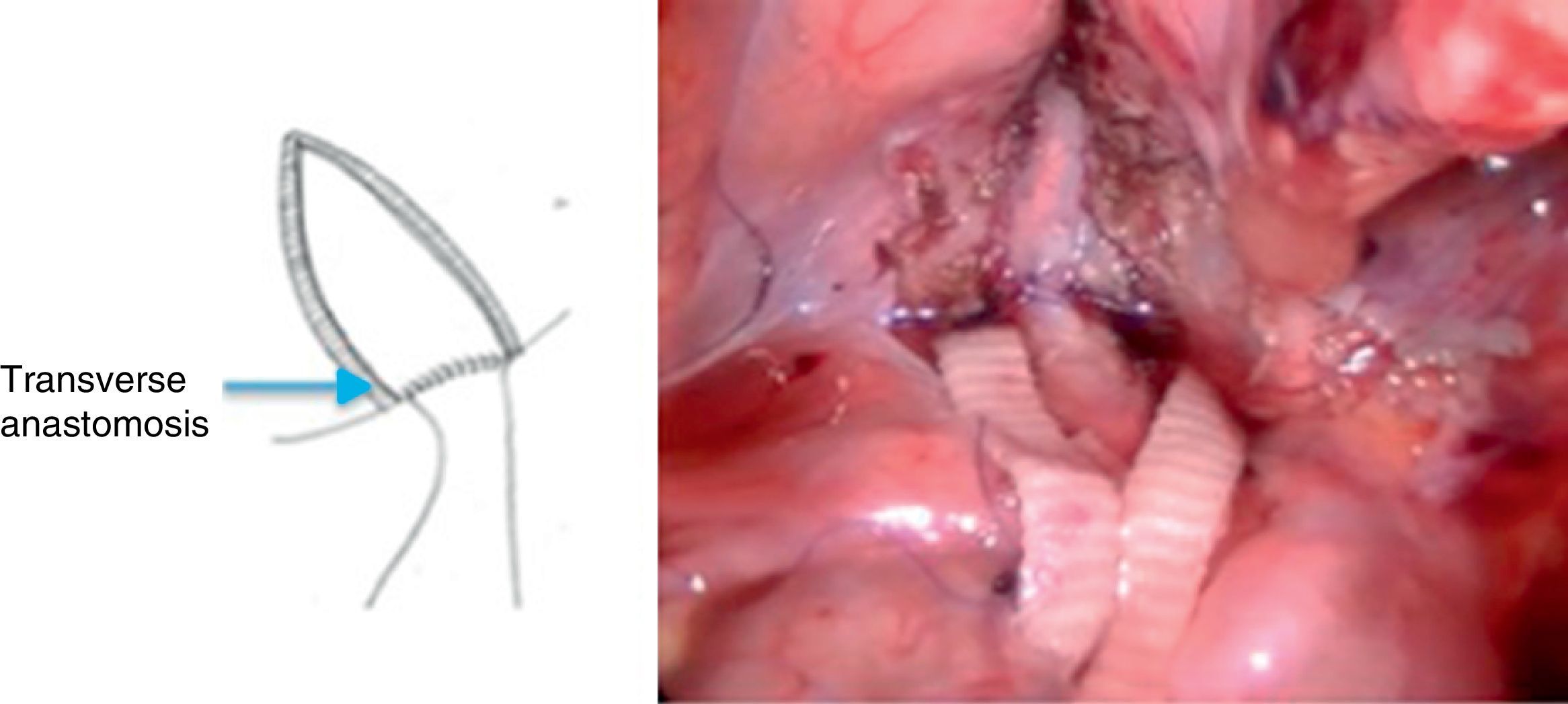
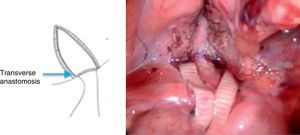
After placing a double J stent, a Heineke-Mikulicz-type anastomosis was performed with Monocryl or Vicryl 5-0 separate stitches or monofilament continuous suture (Figs. 2 and 3).
Finally, Lich-Gregoir detrusorrhaphy was undertaken with separate polyester or Monocryl sutures 3-0 to 4-0.
ResultsThe patients were aged from 5 months to 11 years; all of them had a history of febrile urinary tract infection. Six were male and 2 female. One of the girls had a history of prenatal hydronephrosis and repeated urinary tract infections, and endoscopic dilation of the right ureterovesical junction with a stent at the age of 5 months.
The operation times were from 90 to 120min; hospital stay and length of time the urinary catheter was in situ was 48h. Cephalothin was used at therapeutic doses for 7 days and prophylactically for 8 weeks. The double J stent was removed after 6 weeks.
Follow-up was from 8 to 52 months, with a mean of 2 years. One patient developed a febrile urinary tract infection one week after her surgery, which was resolved by changing the antibiotic to intramuscular ceftriaxone for 5 days. The 6 remaining patients remained free from urinary symptoms, with negative general urine tests and quarterly urine cultures.
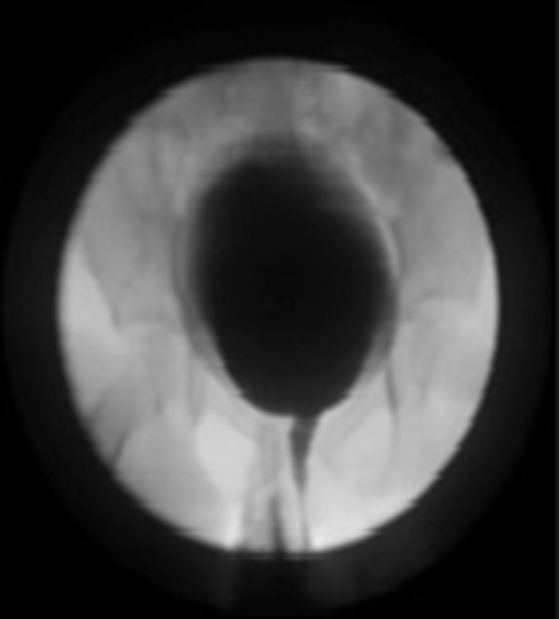
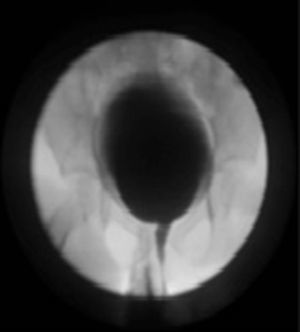
In all cases, ultrasound and intravenous urography at six months showed an improvement in the diameter of the ureter and of the pyelocaliceal ectasia (Figs. 4 and 5).
Seven of the patients underwent micturating cystoureterogram despite having no urinary tract symptoms and with the abovementioned improvement on imaging, with the intention of showing the absence of vesicourteteral reflux. A micturating cystoureterogram was not performed on the one remaining patient because he migrated to a different country, where doctors did not consider it necessary given his excellent condition (Fig. 6).
Only the patient who developed a febrile urinary tract infection one week after the operation underwent MAG 3 5 months afterwards. This patient showed improved excretion curves and improved pyeloureteral appearance on follow-up ultrasound and excretory urography.
DiscussionMinimally invasive procedures designed for the treatment of obstructive megaureter report improvement or relief of hydronephrosis in 50–70% of ureters, with an average follow-up of 3 years. These techniques include insertion of double J stents, balloon dilation followed by placement of double J stent and endoureterotomy. None of these procedures mention systemic cystography for postoperative monitoring to show an absence of reflux.7–9
Kajbafzadeh et al. report a success rate of 71% for the endoureterotomy they describe to treat obstructive megaureter in short distal stenotic segments. This procedure consists of incising the meatus, the ureteral wall and the detrusor muscle at 6 O’clock, placing a double J stent into the ureteral lumen after cutting. However, because it is difficult to calculate the extension of the cut to release the obstruction without causing a complication, this method is limited to stenotic ureteral segments of up to 1.5cm in length.9
As with endoureterotomy, longitudinal ureterovesical plasty with transversal suture (Heineke-Mikulicz) might be considered of little use for the abovementioned long stenoses since, because it results in a wide meatus it might lead to residual reflux. Fortunately, in our experience post-operative cystogram has not shown reflux, and furthermore, the length of the ureterovesical stenosis with resulting megaureter rarely exceeds 1.5cm in length.
Bondarenko recently described a laparoscopic extravesical transverse ureteral reimplantation that included Starr-type remodelling after excision of the site of stenosis.10
Like Agarwal et al., we believe that laparoscopic ureteral tailoring, in the cases of megaureter that require it, might also be facilitated by keeping the ureter joined to the bladder wall rather than disinserting it in order to tailor it.11 The posterior wall of the open ureter resulting from longitudinally incising the stenotic area, might remain joined to the bladder and at the end of the reduction, on the ureteral diameter, a transverse anastomosis made that goes from the anterior ureteral circumference to the vesical mucosa instead of completely disinserting the ureter from the bladder.
Approaching an obstructive and obstructive refluxing megaureter that does not require cutting or plication, in other words, with diameters between 7mm and 11mm, by incising the anterior stenotic portion longitudinally and not completely disinserting the posterior ureter wall appears promising. Laparascopic vision of the ureter up to its junction with the vesical mucosa enables, on the one hand, the length of the stenotic segment to be better identified, and on the other, to relatively accurately even up this opening with that of the vesical mucosa. Once transversal suturing of the entire thickness of the ureteral circumference anterior to the vesical mucosa has been accomplished, it will be possible to calculate whether it is necessary to extend the detrusotomy in relation to the ureteral diameter after relieving the obstruction, and obtain the 5 to 1 proportion that will prevent reflux.12,13
Another advantage of incising the anterior wall of the stenotic segment is that in theory this will enable intravesical advancement of the ureter through a stitch in the trigone towards the wall of the open ureter.14
ConclusionLongitudinal incision of the stenotic area of the ureter with a transverse Heineke-Mikulicz-type anastomosis seems to be a novel and simple alternative to relieve an obstructed megaureter.
This procedure, which we term laparoscopic ureterovesical plasty, showed good clinical, ultrasound and pyelographic results. Micturating cystogram performed intentionally on 7 or the 8 patients showed no residual vesicoureteral reflux.
Although our series is limited in terms of the number of patients, the good outcomes obtained to date might encourage it to be performed on a more significant number of infants.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Landa-Juárez S, Guerra-Rivas A, Salgado-Sangri R, Castillo-Fernandez AM, de la Cruz-Yañez H, Garcia-Hernandez C. Plastia ureterovesical laparoscópica para el tratamiento del megauréter. Cir Cir. 2017;85:196–200.