Aneurysm of the splenic artery is diagnosed when the diameter of the splenic artery is greater than 1cm. It occupies third place among abdominal aneurysms. It is more frequent in women (4:1). It is associated with trauma, haemodynamics and local hormonal effects during pregnancy, portal hypertension (including the Caroli syndrome), arterial degeneration, atherosclerosis, and liver transplantation. It is difficult to diagnose, and it generally presents as ruptured, thus once the diagnosis is made, the surgical approach is indicated due to its high mortality.
Clinical caseFemale of 66 years of age with a diagnosis of splenic artery aneurysm, with pulsing sensation at epigastric level of 8 months onset. On physical examination there is a palpable throbbing mass of 9cm of diameter approximately, for which she was admitted. The computed tomography angiography with reconstruction showed three splenic aneurysms. Two were tied and the larger one was repaired by endo-aneurysmorrhaphy.
DiscussionVisceral aneurysms are extremely rare. They are currently increasing and are the third leading cause of cardiovascular death, as morbidity/mortality is high. The surgical treatment must be done selectively according to their size. Selection of the surgical techniques depends on the anatomic location and the need for revascularisation, the aetiology and the experience of the surgeon.
ConclusionA review has been presented on the advances in diagnostic, and management, concluding that the best is to preserve the spleen, and whatever the technique it must be performed by trained surgeons.
El aneurisma de la arteria esplénica se diagnostica cuando el diámetro de la arteria esplénica es mayor de 1cm. Ocupa el tercer lugar de los aneurismas abdominales y es más frecuente en mujeres (4:1). Etiología: traumatismo, efectos locales hormonales y hemodinámicos del embarazo, hipertensión portal (incluyendo el síndrome de Caroli), degeneración arterial, aterosclerosis y postrasplante hepático. Es de difícil diagnóstico, generalmente comienzan como rotos, por lo que una vez hecho el diagnóstico el abordaje quirúrgico está indicado por su alta mortalidad.
Caso clínicoMujer de 66 años de edad con diagnóstico de aneurisma esplénico; sensación de pulsación a nivel de epigastrio de 8 meses de evolución. A la exploración física se palpa masa pulsátil de 9cm de diámetro aproximadamente, por lo que se decide su hospitalización. La angiotomografía con reconstrucción evidencia 3 aneurismas esplénicos. Dos se ligaron y en el mayor se realizó la endoaneurismorrafia, por no poder excluirlo.
DiscusiónLos aneurismas viscerales son sumamente raros; sin embargo, están actualmente aumentando, siendo la tercera causa de muerte cardiovascular. La morbimortalidad es alta y las posibilidades de supervivencia son escasas al detectarse tardíamente. Deben operarse selectivamente según su tamaño; la selección de las técnicas quirúrgicas depende: de la localización anatómica, de la necesidad de revascularización, de su etiología y, de la experiencia del cirujano.
ConclusiónSe hizo una revisión de los avances diagnósticos y de manejo, concluyendo que lo mejor es preservar el bazo y cualquiera que sea la técnica, debe realizarse por cirujanos capacitados.
Aneurysms of the splenic artery are rare but potentially fatal, with a prevalence of up to 10% in postmortem studies.1 Aneurysm of the splenic artery represents 60% of all splanchnic arteries, and is the third most common abdominal aneurysm, after aortic and iliac aneurysms.2 It is defined as an abnormal dilatation of the splenic artery of more than 1cm in diameter. According to Al-Habbal et al.3 it was described for the first time by Beaussier in 1770, who observed it in autopsies. It was not until 1920 that Hoegler made a preoperative diagnosis. The incidence of splenic artery aneurysms varies from 0.1% to 10.4% in the general population.4 It is 4 times more common in women than in men.3,5 Although the pathogenesis has not been fully clarified, risk factors include: trauma, local hormonal and haemodynamic effects during pregnancy, portal hypertension (including Caroli syndrome) in up to 13%,6,7 fibrodysplasia of the media and atherosclerosis. The development of a new splenic artery aneurysm after liver transplantation can present up to 16 years after transplantation.8
The diagnosis and appropriate treatment of splenic artery aneurysm is important because of the risk of rupture, which increases significantly with a diameter greater than 2cm, with 25–70% mortality depending on the underlying disease.9 Advances in imaging techniques and minimally invasive procedures have revolutionised treatment.
AnatomyThe splanchnic circulation includes the coeliac arteries, and upper and lower mesenteric arteries, which originate in the abdominal aorta. The splenic artery, branch of the coeliac trunk, bifurcates in the hilus of the spleen, it has a 5mm diameter in men, and originates at 1.5cm from the celiac trunk; it primarily irrigates the spleen and the pancreas, and the great curvature of the stomach, together with the short gastric vessels, and the left gastroepiploic artery.10 Seventy-five percent of splenic aneurysms affect the distal third of the artery and 20% the middle third. They are generally solitary and saccular in nature.11 The average size of splenic aneurysms on diagnosis is approximately 2cm; they rarely exceed 3cm.12
The natural history of splenic aneurysms is a gradual increase in size and rupture. Eighty percent are asymptomatic and are diagnosed as a finding or because they rupture, the other 20% which are symptomatic can present with abdominal pain in the epigastrium or in the left hypochondrium radiating to the left shoulder (Kehr's sign) and haemodynamic instability.13 Other symptoms can include anorexia, nausea or vomiting, which are frequently attributed to a co-existing hiatus hernia or other diseases such as gallstones and peptic ulcer disease. However diagnosis is almost always from a chance discovery,14 because a pulsatile mass is rarely palpated on clinical examination.
Spontaneous rupture of the aneurysm presents initially in 2–10% of patients;15 it is currently reduced to 3% with advances in diagnosis. Occasionally a double rupture can present within 48h; this phenomenon was described by Bockerman in 1930.4,15 Secondary erosion of the aneurysm into adjacent viscera can cause gastrointestinal haemorrhage in 13% of patients due to rupture to the stomach, colon or pancreatic duct. Erosion in the splenic vein can cause an arteriovenous fistula with portal hypertension, or even mesenteric steal syndrome and ischaemia of the small intestine.4
Spontaneous rupture is the most serious complication of splenic aneurysm, with 25% mortality; it is more frequent during pregnancy, when mortality rises to 75–90%.16
As the population's life expectancy rises, with the use of ultrasound and cross-sectional imaging,4,15 incidental diagnosis is also on the increase. Ultrasound has the advantage that it can be used during pregnancy.
Once a suspected diagnosis has been made, digital subtraction angiography is indicated, as it can define the precise location of the aneurysm, the collateral branches can be investigated, and the source of bleeding, and other visceral aneurysms can be documented or excluded.2,15
Ultrasound can be used for follow-up, however, multislice computed tomography is preferable. Indications for intervention are associated with the natural history of the disease, placing the emphasis on the factors which increase the risk of spontaneous rupture. Calcification, advanced age and normotension do not preclude rupture of the aneurysm.17
Treatment depends on the presentation, location and the size of the aneurysm, and can involve conventional or laparoscopic surgery, endovascular embolisation, and exclusion of the aneurysm by stent. It is important to make every effort to preserve the spleen in order to preserve immunological function, unless the aneurysm is located in the splenic hilus.17 However, there is evidence that ligature or embolisation of the splenic artery alters the function of the spleen, even if it is preserved.18 Open surgery approaches can include splenectomy with excision of the aneurysm, proximal and distal ligature of the splenic artery with or without resection of the aneurysm, and endo-aneurysmorrhaphy.5 Partial splenectomy can be performed for distal aneurysms, preserving the unaffected splenic parenchyma. The mortality rate associated with open surgery is 1.3%, with a morbidity rate of 9%.19
Aneurysms of the splenic artery can be approached via an anterior or a lateral route. Using the latter approach the short gastric and left gastroepiploic vessels can be compromised, which increases the risk of splenic infarction, and the lateral retroperitoneal approach preserves collateral splenic perfusion.20
Arca et al.5 conclude that a laparoscopic approach for a splenic aneurysm is a safe and feasible alternative, provided it is undertaken by an experienced surgeon using intraoperative ultrasound, which has been demonstrated to be less invasive than open surgery. A laparascopic approach is contraindicated in haemodynamically unstable patients or with other signs of rupture.5 As with the open approach, the laparascopic approach can be either anterior or lateral. A lateral approach might be appropriate for central and distal aneurysms.16
Transcatheter embolisation was first described by Probst et al. in 1978.21 The advances in digital subtraction angiography, and the development of a wide variety of arterial catheters and associated equipment have increased its successful application in 85–100% of cases. It is currently considered the first line of treatment for the majority of patients with splenic aneurysms, particularly for incidental asymptomatic aneurysms.22,23
After computed tomography, embolisation should occlude the source of the aneurysm.19,24 It is contraindicated in splenic aneurysms located in the splenic hilus,24 and is indicated when the aneurysm is difficult to manage and/or in high risk patients. Complications include migration of the coil and distal infarction, abscess formation and, rarely, rupture of the aneurysm.24 Recanalisation can occur in up to 12.5% of patients. Embolisation can also fail for technical reasons if the splenic artery is particularly tortuous. Some authors have reported a conglomeration of symptoms in embolised patients, which has been termed postembolisation syndrome,19 characterised by fever, abdominal pain, ileus, and occasionally pancreatitis, affecting up to 39% of patients.
Recent innovations in the treatment of splenic aneurysms include the use of endovascular stents. This is a minimally invasive technique, which excludes aneurysmatic dilatation of the artery, preserving normal blood flow. The size and tortuosity of the splenic artery, and the position of the aneurysm limit the use of a stent. They are more appropriate for proximal aneurysms.11 Stents have a significantly lower risk of splenic infarction compared to embolisation; they also have the advantage over embolisation in situations where preservation of the arterial flow to the spleen is necessary for other reasons.25
Combined therapy in stages (embolisation followed by surgical resection) is recommended in specific situations, especially in the management of giant aneurysms and in patients with significant comorbidities.26 The use of robot technology can enable a more precise surgical procedure, including anastomosis of small structures in selected patients.27
False aneurysms of the splenic artery constitute a completely different clinical scenario. Most authors recommend active management without delay, without taking size, symptoms or rupture into account. Patients with a false splenic aneurysm are usually affected by an underlying disease, which is generally pancreatitis or pancreatic fistulae. Mortality, after open surgical intervention on false aneurysms close to the pancreatic head is from 16% to 50% for those near the body and the tail.19,26 The recommended primary treatment should be the endovascular approach28 which can be used in the case of voluminous false aneurysms of the splenic artery.21,26 Rupture of a false aneurysm curing embolisation is exceptionally rare,22 failures have been reported, especially if the false aneurysm is associated with a pancreatic pseudocyst.10
Given the absence of media in the wall of the false aneurysm and the resulting weakness, the isolation technique using stents might be preferable to embolisation.29 Percutaneous injection of thrombin is another option in the treatment of false aneurysms in selected patients, especially if catheterisation cannot be performed. Hunang et al.30 have reported the successful treatment of a false aneurysm of the giant splenic artery, by percutaneous thrombin–collagen injection.
We present the case of a patient with multiple aneurysms of the splenic artery, which was operated using the open technique, preserving the spleen.
Clinical caseA 66-year-old woman, allergic to naproxen; a history of caesarean section 29 years ago, and osteosynthesis in her left foot from being run over, without specifying the date or complications. She started to experience a sensation of pulsation at the level of the epigastrium, and occasional abdominal pain in 2013, where angiotomography gave an image suggestive of an aneurysm of the splenic artery, for which she was referred to our unit.
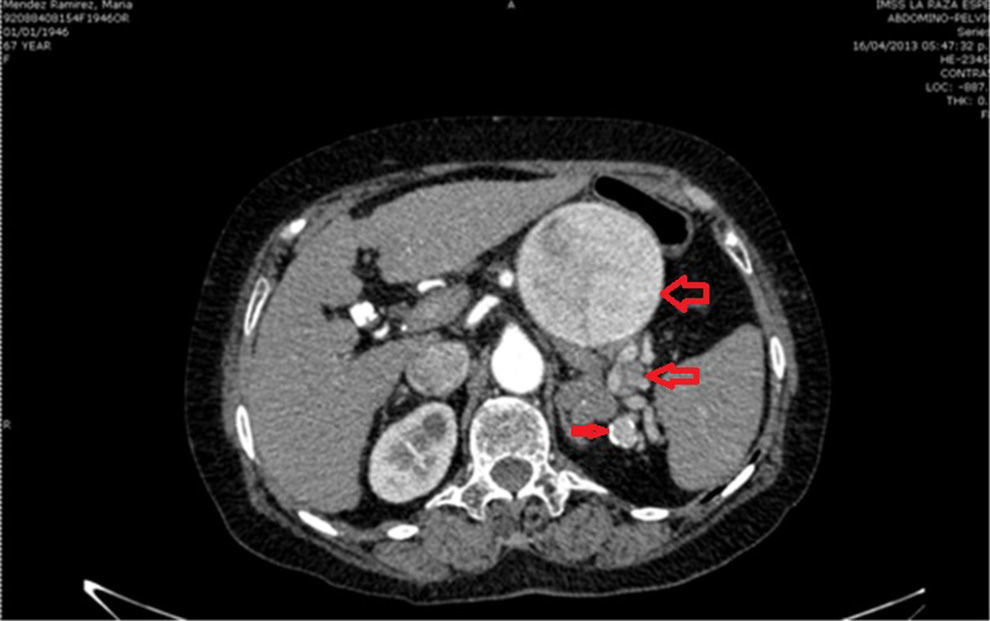
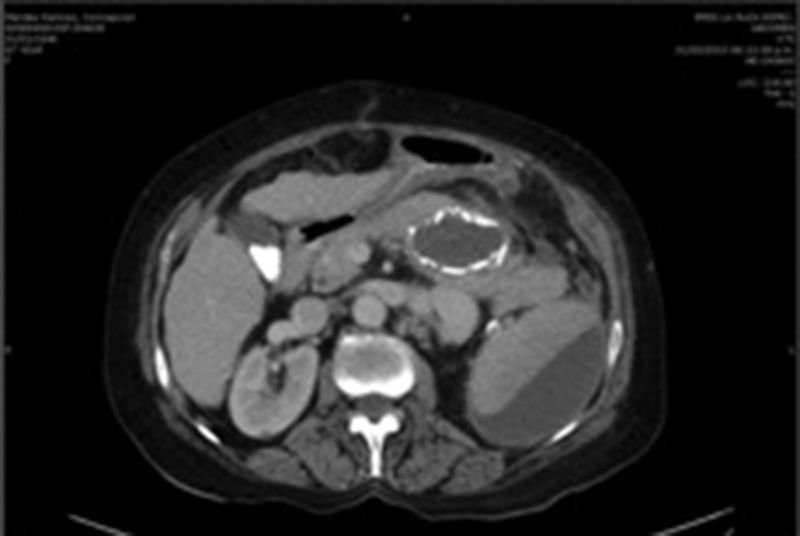
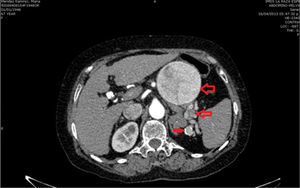
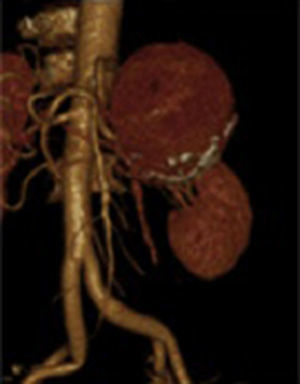
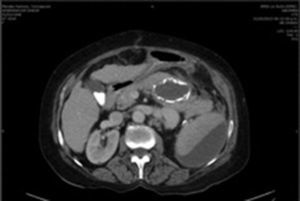
Due to the size of the lesion on physical examination, it was decided to admit the patient to hospital. On admission her laboratory test results were: glucose 118mg/dl, serum creatinine 0.6mg/dl, haemoglobin 15.3g/dl, leucocytes 4.3×109/l USI, platelets 109×109/l USI, prothrombin time 16.8s, and INR 1.25. A further angiotomography with reconstruction was requested, which revealed 3 uncomplicated aneurysmatic lesions, the first 8cm, the second 3.4cm and the third 1.6cm in diameter (Fig. 1), and therefore they were closely monitored. A preoperative study protocol was requested and open surgery suggested, owing to the diameter of the lesion and the comorbidities.
On physical examination the patient was: afebrile, haemodynamically stable, oriented, with good colour, and good mucosa and tegument hydration, carotid pulses were present with no murmurs, no cardiopulmonary involvement, flat abdomen, with a pulsatile tumour of approximately 7cm, negative DeBakey manoeuvre, no murmur or thrill, with no signs of peritoneal irritation. No abnormal signs in upper and lower limbs.
Respiratory function test with a risk of I/V. ASA III cardiac risk, Goldman's II, Lee I, 0.9% probability of cardiac complications.
The haematology unit indicated platelet transfusion before and after surgery.
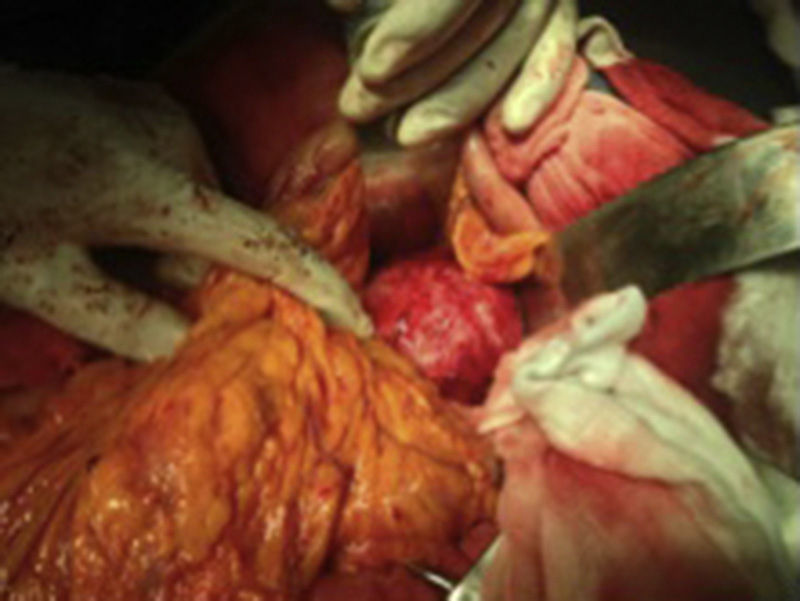
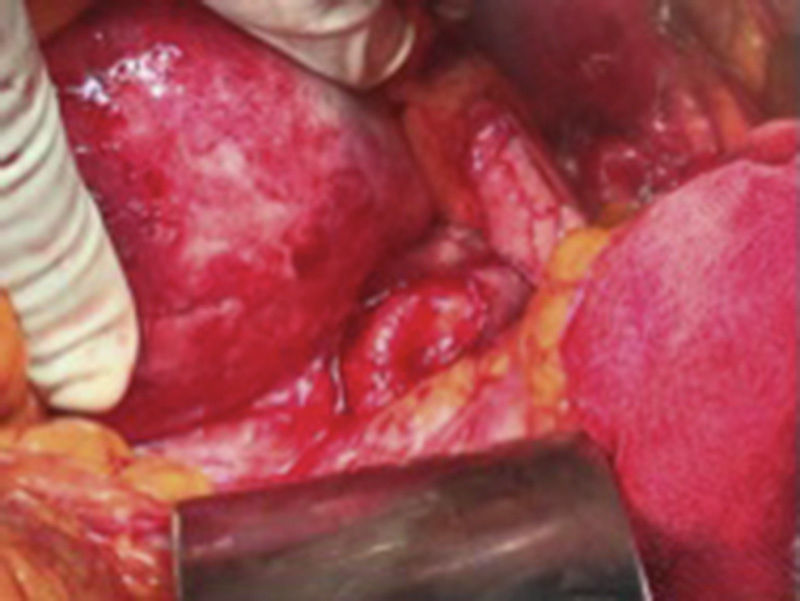
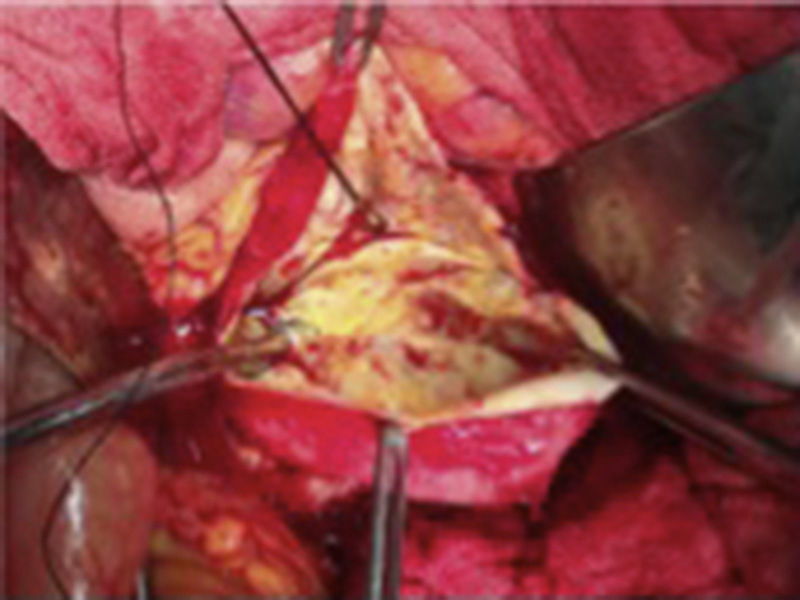
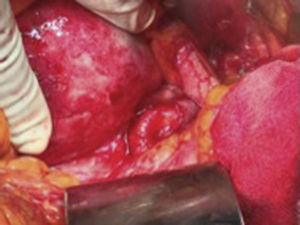
The patient was scheduled for open surgery, with a prior platelet count of 249×109/l USI, a midline supra and infraumbilical abdominal incision was made, and a tumour of 9cm in diameter was found firmly adhered to the posterior gastric surface, transverse colon and loops of the small bowel. Therefore it was decided to approach the tumour via the transcavity of the omentum at its posterior border (Fig. 2). Dissection was made until the splenic artery was identified near the spleen, a splenic aneurysm was observed of 3.5cm, it was excluded ligating the splenic artery proximally and distally to the lesion. On retrograde dissection another aneurysmatic dilatation was found of approximately 2cm, and was excluded in the same way. The splenic artery proximal to the major aneurysm of approximately 9cm was dissected (Fig. 3). The posterior surface of this aneurysm was firmly attached to the pancreas and the splenic vein. The lower ventral surface had firm adherences to the duodenum and jejunum, therefore the splenic artery was identified at its source alone, in order to ligate it. It was not possible to dissect the proximal end, as there were firm adherences of the coeliac trunk with the aneurysmal sac, therefore the aneurysmal sac was opened, and by control with Fogarty 3Fr balloon-tipped catheter of the proximal and distal ostium which still had blood flow, the endoaneurysmorrhaphy was performed (Fig. 4). The proximal ostium was in the shape of a bevelled buttonhole. Occlusion and haemostasis of the ostia were corroborated, and the proximal portion of the splenic artery was identified with its opening diagonally into the aneurysmal sac, as this was laterally attached to the aneurysm (Fig. 5). The few thrombi and part of the resected aneurysmal sac were sent for histopathological study and culture; the sac was then sutured. The spleen was observed to be hypertrophic with no evidence of areas of ischaemia during surgery.
The patient progressed well, afebrile, with abdominal pain of low intensity in the mesogastrium and left hypochondrium. Her platelet count lowered to 67.0 with leucocytosis of 11,000 and neutrophilia of 87.6, with no bandaemia, serum amylase of 500u/l, and therefore a contrasted computed tomography was requested after 48h which revealed hypodense areas involving almost 50% of the splenic parenchyma (Fig. 6). In subsequent biometries an increase in platelet count to 99.0 was observed.
The patient was discharged home well and tolerating an oral diet.
She was seen as an outpatient 15 days later and had progressed well, and was discharged from her local hospital after one month with no changes in clinical parameters.
DiscussionVisceral aneurysms are extremely rare. The first cases were described 200 years ago with a micotic aneurysm of the superior mesenteric artery. Case series reports are few and limited to no more than 10 patients.
Because they are so rare other possible differential diagnoses need to be considered, such as cystic pancreatic tumours, which are common in women, pancreatic pseudocysts, although these can be ruled out if there is no history of acute or chronic pancreatitis. Another extremely rare disease is neuroendocrine tumour.31
As we mentioned early, in the last 2 decades there has been a 7-fold increase in the frequency of abdominal aneurysms, and they are the third cause of cardiovascular death. Fifty percent of women with splenic aneurysms are multiparous. In our country, with an ageing population, a birth rate of 18.87 births per 1000 inhabitants, and increasingly frequent liver transplantations, this disease will have an increasing impact. Therefore this disease needs to be taken into consideration because its mortality is very high when detected late. We should be aware of its presence as the chances of survival are low.31
The splenic artery in men has an average diameter of 5mm, and according to the definition of aneurysm, it is termed an aneurysm when the diameter exceeds 50% of the normal diameter of the vessel involved. Even so, surgery is indicated when its diameter is 2cm. However, it is more common in women, who have smaller arteries with narrower diameters, and they are generally diagnosed when the aneurysm ruptures with very high mortality, and therefore most should be operated when they are diagnosed.
Ideally, blood flow should be re-established after the aneurysm has been resected or excluded, or the splenic artery dissected and ligated at its portion proximal and distal to the lesion, but in our case, the inflammatory process around the aneurysmal sac which was firmly adhered to the coeliac trunk, to the pancreatic tissue, and to the splenic vein prevented dissection of the splenic artery near to its source (Fig. 5), therefore, despite its originating in the middle third, the lesion had to be opened and endo-aneurysmorrhaphy performed of the 2 ostia (primum non nocere), and injury avoided to other structures such as the pancreas, the intestinal loops or compromising the integrity of the coeliac trunk; because as stated in the medical references “treatment depends on the manner of presentation, the location, and the size of the aneurysm”.32
A ruptured aneurysm can manifest acutely, into the pancreatic duct, and result in a clinical picture known as hemossucus pancreaticus.33
It has been mentioned that splenic artery aneurysms rupture more frequently, especially in pregnant women, and that it has been found in postmortem studies that they can be more common than aneurysms of the abdominal aorta.
Aneurysms should be operated selectively according to their size, and this procedure should be performed as an emergency when they rupture and unstable symptoms, contained ruptures, aneurysms that are embolising, and those that are infected cause shock.31
Various surgical treatment options are offered, and the selection of one of the diverse techniques will depend on the anatomical location of the aneurysm, on the need for revascularisation, its aetiology, and the experience of the surgeon.33 Preservation of the spleen is increasingly preferred, we should not fail to mention that multiple aneurysms present in 22%,29 and the laparoscopic approach is being used in order to avoid large-scale surgery, ligating the splenic artery with or without splenectomy.5
With splenic infarction, as the efficient volume of the spleen is reduced, blood elements increase which accumulate in the spleen, and result in an increased red blood cell, white blood cell and platelet count.
Complications which can present are abdominal pain, fever, rupture, splenic abscesses, pneumonia and septicaemia, and many patients with splenic infarction can remain asymptomatic.
Diagnosis can be made by means of ultrasound or computed tomography. The initial treatment is medical, with analgesics and anticoagulants. Surgery is only indicated for cases which present complications, such as splenic abscess or rupture, or when diagnosis is imprecise.34
Open surgery on visceral aneurysms is still the procedure of choice to repair aneurysms that have been diagnosed late; however, minimally invasive endovascular techniques can also offer advantages with conventional treatment, providing, as Suso et al. mention,35 they are performed by a surgeon of proven experience. It is important to highlight that endovascular techniques are not free from risk, they can cause the secondary aneurysm to rupture with the increase in pressure when inserting the embolic material, result in incomplete thrombosis of the aneurysm, and fail to obliterate the collateral branches which might be keeping the aneurysm “pressurised”,36 and cause the inadvertent occlusion of another vessel, migration of the coils, and infection.
Elective resection of splenic aneurysms carries a risk of complications, such as: ischaemia of the spleen (up to 29%)36 which requires splenectomy.
ConclusionsAneurysms of the splenic artery that are at low risk of rupture can be managed without intervention, with radiological follow-up every 6 months with ultrasound or computed tomography, in order to evaluate the progression of the aneurysm.
Surgical intervention should be considered if the aneurysm is symptomatic, if it has enlarged over 2cm in diameter or if it is found during pregnancy or at a reproductive age.
All false aneurysms of the splenic artery should be treated as rapidly as possible.
The choice between embolisation and placing a stent depends on: the size, shape and site of the splenic artery aneurysm, and the experience of the surgeon.
Due to the anatomy of her splenic artery, our patient was not a candidate for embolisation, because if an occluding device or covered stent had been placed it would occlude the coeliac trunk.
A laparoscopic approach might be considered if exposure to radiation is contraindicated (pregnancy), or when endovascular techniques fail or are not available.
Ruptured or complicated splenic aneurysms should be resolved by means of conventional open surgical technique. The inclusion of interventionist radiology might enable a combined approach (surgical and radiological), in the treatment of complex or difficult ruptured aneurysms.
Conflict of interestsThe authors have no conflict of interest to declare.
Please cite this article as: Bizueto-Rosas H, Barajas-Colón JA, Delgadillo-de la O I, Malo-Martínez NP, Pérez-González HA, Hernández-Pérez NA. Aneurismas esplénicos múltiples; exclusión quirúrgica con conservación del bazo. Cirugía y Cirujanos. 2016;84:58–64.