Hepatic trauma is a common cause for admissions in the Emergency Room. Currently, non-surgical management is the standard treatment in haemodynamically stable patients with a success rate of around 85–98%. This haemodynamic stability is the most important factor in selecting the appropriate patient. Adjuncts in non-surgical management are angioembolisation, image-guided drainage and endoscopic retrograde cholangiopancreatography. Failure in non-surgical management is relatively rare but potentially fatal, and needs to be recognised and aggressively treated as early as possible. The main cause of failure in non-surgical management is persistent haemorrhage.
The aim of this paper is to describe current evidence and guidelines that support non-surgical management of liver injuries in blunt trauma.
El trauma hepático es una causa frecuente de admisión en la sala de urgencias. El manejo no operatorio es actualmente el tratamiento estándar en los pacientes hemodinámicamente estables, con buenos resultados en el 85 al 98% de los casos. La estabilidad hemodinámica es el factor más importante que influye en la elección del paciente apropiado. Los adyuvantes en el tratamiento no operatorio son: angioembolización, drenaje guiado por imagen y colangiopancreatografía retrógrada endoscópica, entre otros. La falla de tratamiento no operatorio es una complicación poco frecuente pero potencialmente mortal que requiere el reconocimiento temprano para establecer un manejo intensivo. La principal causa de falla de tratamiento no operatorio es la hemorragia persistente.
El objetivo del presente artículo es describir la evidencia existente y las guías clínicas que apoyan el manejo no operatorio del trauma hepático no penetrante.
Traumatic injuries are the main cause of death in Mexico of patients from the age of 1–441,2 and the third cause of death world-wide, with more than 5 million deaths each year.3 In abdominal trauma, the liver is the most frequently affected organ due to its location and size.4 Traumatic liver injuries are more common in men than women at a ratio of 3:1.3 Falls from a height, motor vehicle accidents and firearm and knife wounds are the most frequent causes.1,5 The right hepatic lobe is the main site for injuries in 41% of cases, while the left hepatic lobe is affected in 9% and the remainder are bilateral.5 In northern Europe non-penetrating trauma is the most frequent cause in 92% of cases,5 but in the continent of America, penetrating trauma is the most common cause of liver injury in hepatic trauma patients.6
Anatomical classification of liver trauma injuriesThe segmentary anatomy of the liver bears little importance in trauma, except to describe the site of the injury.7 In order to provide a common and unified language to facilitate clinical decision-making in cases of trauma, the American Association for Surgery of Trauma published their Organic Injury Scale system in 1994 (AAST-OIS), based on the degree of anatomic disruption of each organ; it describes 6 grades of injury: 1 minimal, 2 mild, 3 moderate, 4 severe, 5 massive and 6 lethal.8,9
The AAST-OIS classifies liver injuries as:
Grade I. Subcapsular haematoma<0% not expansive of surface area or capsular laceration with no bleeding<1cm in depth.
Grade II. Subcapsular haematoma involving 10–50% not expansive of surface area, or capsular laceration with active bleeding 1–3cm in depth.
Grade III. Subcapsular haematoma>50% of surface area or laceration>3cm in depth.
Grade IV. Ruptured parenchymal haematoma with active bleeding, or laceration, or parenchymal haematoma involving 25–75% of a hepatic lobe or affecting 1–3 Couinaud segments.
Grade V. Parenchymal laceration involving>75% of one hepatic lobe or more than 3 Couinaud segments in the same lobe. Vascular injury of the suprahepatic veins, retrohepatic vena cava or portal vein.
Grade VI. Hepatic avulsion.6,8–10
Grade IV and V (AAST-OIS) liver injuries are referred to as complex injuries.11 Because AAST-OIS grade VI injuries are lethal, many authors suggest that they should not be taken into account for practical purposes in Emergency Room care, as all these patients die at the site of the accident and their diagnosis is confirmed at autopsy.6 Non-complex AAST-OIS grade I–III hepatic injuries are the most common.5,10
Pathophysiology of traumatic liver injuriesTwo types of mechanisms cause liver injury: penetrating trauma, and non-penetrating or blunt trauma.6 A Brazilian study found a frequency of penetrating lesions of 61.6% of patients, and non-penetrating injuries occurred in 38.4%.10 Penetrating trauma occurs because of the inverse proportional relationship of energy and applied surface area. The high levels of kinetic energy inflicted with an injuring object on a small area of distribution cause vascular or biliary intrahepatic transection forces, capsular rupture and parenchymal injury.6 With blunt trauma, injuries occur due to deceleration forces and direct contusion. According to Newton's First Law or the law of inertia, bodies remain in a state of rest or uniform and rectilinear motion unless they have to change this state due to forces inflicted upon them. Thus, a patient who is travelling in a motor vehicle and is involved in a traffic accident with frontal impact, for example, has to stop their movement, but their organs will continue their movement forwards causing subcapsular haematoma or rupture of the parenchyma due to uniform displacement and its traction by the ligaments that fix it to the retroperitoneum, the diaphragm and the vascular pedicles. In the case of injuries due to direct contusion, the application of high levels of energy over a directly proportional surface area in the liver will also cause haematomas and subcapsular and parenchymal lacerations or vascular tears.6,12
Non-operative management of blunt liver traumaTwo principal aspects govern the current treatment of liver trauma injuries: haemodynamic stability and the mechanism of trauma.13 The treatment of patients with blunt liver trauma has changed greatly since 1990. Exploratory laparotomy as routine treatment has been replaced by non-operative management, which is currently standard for liver trauma injuries in most trauma centres.14 Many studies confirm that most patients with liver trauma can be managed non-operatively.15 One study found that 86.3% of patients can be managed without laparotomy.16 Haemorrhage due to haematoma or liver laceration stops spontaneously in 80% of patients.13 Trauma kinematics, the number of injured organs, penetration of the abdominal cavity and haemodynamic stabilities are decisive factors in decision-making on how to manage liver injuries, but they do not constitute absolute contraindications for the non-operative management of liver trauma injuries.17
Haemorrhage is the principal cause of death, therefore it is important to identify its origin and magnitude in haemodynamically stable patients for whom non-operative treatment has been decided. This presents a diagnostic challenge which might delay the start of intensive management and prevent the fatal triad of hypothermia, acidosis and coagulopathy, which are indicators of irreversible progression.
The advantages of the non-operative management of liver injuries (providing this is possible) are: reduction in hospital care costs, early discharge from hospital, avoiding non-therapeutic laparotomies, a reduction in intra-abdominal complications and fewer blood transfusions.16
Eastern Association for the Surgery of Trauma Clinical Guidelines 2012The methodology developed by the Agency of Healthcare Policy and Research of the United States Department of Health and Human Services was to consider the following classes of evidence6: evidence class I, prospective randomise studies, multicentre; evidence class II, prospective non-comparative studies, and evidence class III, retrospective studies, case series, databases, registries and case reviews. The following recommendations are accepted based on the level of evidence, level I recommendations are convincingly justifiable based on strong class I and II scientific evidence; level 2 recommendations are reasonably justifiable based on class II and III evidence; level 3 recommendations are considered to be those that are backed by class III studies useful for educational purposes or to direct further research. Based on the above, the experts from the Eastern Association for the Surgery of Trauma established the following recommendations after analysing 94 manuscripts from 1996 to 2011:
Level 1 recommendations- a)
Patients who are haemodynamically unstable or with peritonitis should be taken urgently for laparotomy.
- a)
Routine exploratory laparotomy is not indicated in the haemodynamically stable patient with no signs of peritonitis.
- b)
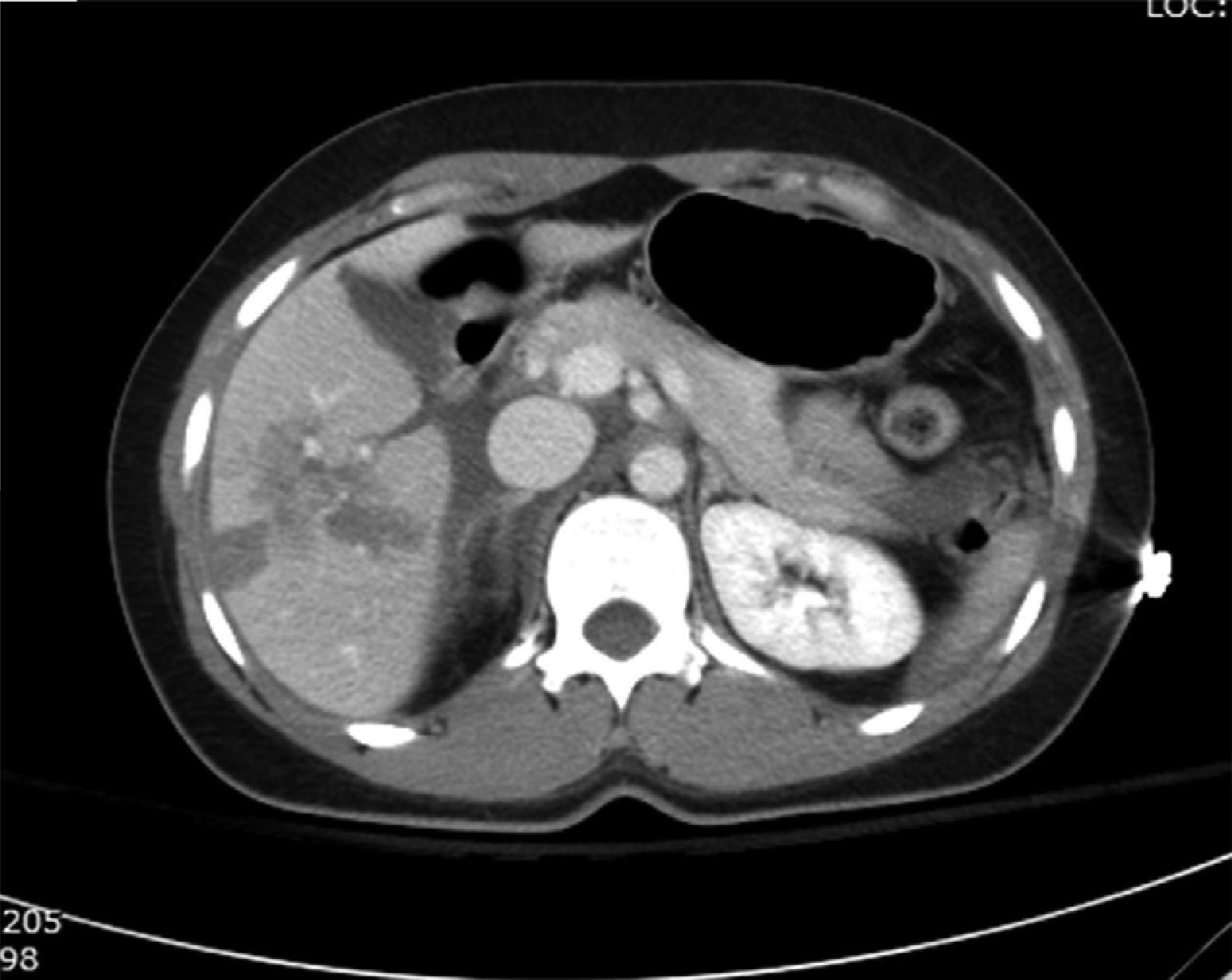
In the haemodynamically stable blunt abdominal trauma patient without peritonitis, an abdominal computed tomography scan with intravenous contrast should be performed to identify and assess the severity of the liver injury.
- c)
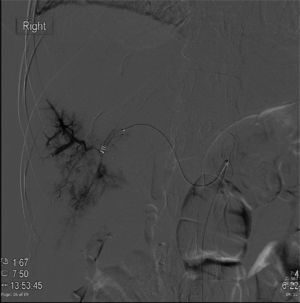
Angiography with embolisation may be considered as first-line intervention in patients who are transient responders to resuscitation (Fig. 1).
- d)
The severity of the injury, the neurological status, age and associated injuries are not absolute contraindications to a trial of non-operative management in haemodynamically stable patients.
- e)
Angiography with angio-embolisation should be considered as first-line treatment in stable patient with evidence of active extravasation (blush) on the abdominal CT scan (Fig. 1).
- f)
Non-operative management of hepatic trauma should only be undertaken in an environment that has the capacity for continuous monitoring, serial clinical evaluations and an operating room available for emergency laparotomy (Figs. 2 and 3).
- a)
After hepatic injury, persistent systemic inflammatory response, increasing abdominal pain, a drop in haemoglobin or the presence of jaundice should be assessed by computed tomography.
- b)
Interventional modalities such as endoscopic retrograde cholangiopancreatography, percutaneous drainage or even laparoscopy may be used to resolve complications secondary to non-operative management of liver trauma.
- c)
Pharmacological prophylaxis to prevent venous thromboembolism in patients with isolated blunt hepatic trauma can be used without increasing the failure rate of non-operative management.
The authors have no conflict of interest to declare.
Please cite this article as: Noyola-Villalobos HF, Loera-Torres MA, Jiménez-Chavarría E, Núñez-Cantú O, García-Núñez LM, Arcaute-Velázquez FF. Tratamiento no operatorio de las lesiones hepáticas por trauma no penetrante: artículo de revisión. Cir Cir. 2016;84:263–266.