In patients with unresectable gastric cancer and outlet obstruction syndrome, gastric partitioning gastrojejunostomy is an alternative, which could avoid the drawbacks of the standard techniques.
ObjectiveComparison of antroduodenal stent, conventional gastrojejunostomy and gastric partitioning gastrojejunostomy.
Material and methodsA retrospective, cross-sectional study was conducted on patients with unresectable distal gastric cancer and gastric outlet obstruction, treated with the three different techniques over the last 12 years, comparing results based on oral tolerance and complications. An analysis was performed on the results using the Student's t test for independent variables.
ResultsThe 22 patients were divided in 3 groups: group I (6 cases) stent, group II (9 cases) conventional gastrojejunostomy, and group III (7 cases) gastric partitioning gastrojejunostomy, respectively.
The stent allows a shorter “postoperative” stay and early onset of oral tolerance (p<0.05), however, the gastric partitioning gastrojejunostomy achieve normal diet at 15th day (p<0.05). The mortality rate was higher in the stent group (33%) compared with surgical techniques, with a morbidity of 4/6 (66.7%) in group I, 6/9 (66.7%) group II, and 3/7 (42%) group III. Re-interventions: 2/6 group I, 3/9 group II, and 0/7 group III. The median survival was superior in the gastric partitioning gastrojejunostomy, achieving an overall survival of 6.5 months.
ConclusionsThe gastric partitioning gastrojejunostomy for treatment of gastric outlet obstruction in unresectable advanced gastric cancer is a safe technique, allowing a more complete diet with lower morbidity and improved survival.
En pacientes con cáncer gástrico irresecable con obstrucción antral, la gastro yeyuno anastomosis con separación gástrica parcial es una alternativa, que evitaría los inconvenientes de las técnicas habituales.
ObjetivoComparar stent antroduodenal, gastro-yeyuno-anastomosis convencional y gastro-yeyuno-anastomosis con separación parcial gástrica.
Material y métodosEstudio retrospectivo durante 12 años, transversal en enfermos con cáncer gástrico distal irresecable y obstrucción gástrica; tratados con 3 técnicas diferentes, comparando sus resultados en función de la tolerancia oral y las complicaciones. Se analizaron los resultados con la t de Student para variables independientes.
ResultadosVeintidós pacientes divididos en 3 grupos: grupo I stent (6 casos), grupo II (9 casos) gastro yeyuno anastomosis convencional y grupo III (7 casos) gastro yeyuno anastomosis con separación gástrica parcial.
El stent permite una estancia «postoperatoria» más corta e inicio de la tolerancia de alimentos precoz (p<0.05). La gastro yeyuno anastomosis con separación gástrica parcial permite una dieta normal a los 15 días (p<0.05). La mortalidad fue superior en el stent (33%), comparada con las técnicas quirúrgicas. La morbilidad fue 4/6 (66.7%) en el grupo I, 6/9 (66.7%) en el grupo II y 3/7 (42%) en el grupo III. Las reintervenciones: 2/6 grupo I, 3/9 en el grupo II y 0/7 en el grupo III. La supervivencia media fue superior (6.5 meses) en grupo III.
ConclusionesLa gastro yeyuno anastomosis con separación gástrica parcial en la obstrucción gástrica por cáncer gástrico avanzado irresecable es una técnica segura, permitiendo una dieta más completa con menor morbilidad y mejor supervivencia.
In patients with unresectable gastric cancer and outlet obstruction syndrome, partial stomach-partitioning gastrojejunostomy is an alternative which could resolve the obstruction and is an alternative that might avoid the drawbacks of the standard techniques.
In cases of advanced, unresectable distal gastric cancer, with outlet obstruction, even in cases where an associated resection of the neighbouring tissues or organs has been performed, it is not realistic to expect increased survival; yet there are increased postoperative complications.1
Gastric cancer is the second most common cause of death worldwide. When it presents as gastric obstruction syndrome, it causes nausea, vomiting, loss of appetite and malnutrition, which have a negative impact on the survival and quality of life of these patients. It is also associated with a poor clinical course and prognosis even when curative resections are performed.2
Although chemotherapy is the initial treatment in cases of advanced gastric cancer, the symptoms associated with gastric obstruction cause digestive intolerance which makes oral chemotherapy regimens impossible, therefore, in this clinical situation, the most appropriate initial treatment appears to be surgical or endoscopic.2,3 In these cases, other palliative solutions include placing an antroduodenal stent or bypass surgery, and traditionally conventional gastrojejunostomy is indicated in order to improve quality of life and to enable these patients food intake. A good result is achieved in over 70% of cases.4,5 Conventional bypass surgery has been the standard palliative treatment for gastric outlet obstruction syndrome in unresectable gastric cancer. Occasionally this surgical drainage is not completely effective in relation to oral intake, because it is associated with neural factors which delay gastric emptying, which varies from 3% to 31% in recent studies6; therefore, up to a third of patients operated using this traditional technique experience no palliation of their symptoms. Antrectomy with gastrojejunostomy or the Devine exclusion procedure has proved an effective alternative to traditional gastrojejunostomy, as it enables better oral intake in these cases,7,8 however it does have some drawbacks in that it requires a drainage tube in the distal gastric remnant if the antrum is totally occluded, and it is impossible to perform this technique if the minor curvature has been infiltrated. In 1997 Kaminishi et al.,9 with a view to resolving these problems, presented a surgical technique modifying the Devine procedure which consisted of a partial stomach-partitioning gastrojejunostomy. Their results demonstrated a lower rate of tumour bleeding, lower delayed gastric emptying rates and greater and more complete oral tolerance than conventional gastrojejunostomy.
Endoscopic placement of a self-expanding metal stent is now another alternative. This results in a more rapid resolution of symptoms and a lower morbidity rate after the procedure, but the drawbacks with this option have been described as the recurrence of obstructive symptoms and a greater need for reintervention.10
ObjectiveThe aim of this study was to compare 3 palliative techniques used to treat unresectable gastric cancer and outlet obstruction syndrome. These techniques comprise the placement of an antroduodenal self-expandable metallic stent (group I), conventional gastrojejunostomy (group II) and partial stomach-partitioning gastrojejunostomy, Kaminishi's technique modified (group III). We assessed the outcomes of the techniques, principally focussing on efficacy in terms of oral intake, unfavourable incidents and impact on the patients’ progress.
Material and methodsA retrospective, cross-sectional study was performed in which the patients were divided into 3 groups in order to compare them according to their treatment. We reviewed patients treated with conventional gastrojejunostomy (group II) and partial stomach-partitioning gastrojejunostomy, (group III) with unresectable gastric cancer and outlet obstructive syndrome, from 1 February 2000 to 1 February 2012, in the University Health Complex of Salamanca, Spain. A group of patients was added randomly, with the same diagnosis and clinical situation, who had been fitted with a stent (group I). We attempted to ensure that this group was homogeneous in terms of number with the other 2 groups (Table 1).
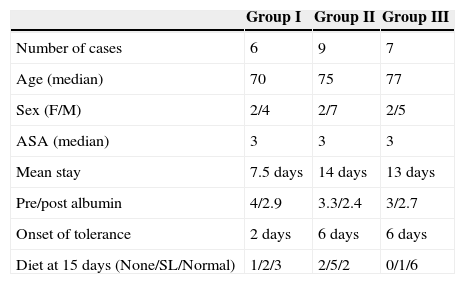
Demographic data, and relationship between onset of diet and type of diet between the different groups.
| Group I | Group II | Group III | |
|---|---|---|---|
| Number of cases | 6 | 9 | 7 |
| Age (median) | 70 | 75 | 77 |
| Sex (F/M) | 2/4 | 2/7 | 2/5 |
| ASA (median) | 3 | 3 | 3 |
| Mean stay | 7.5 days | 14 days | 13 days |
| Pre/post albumin | 4/2.9 | 3.3/2.4 | 3/2.7 |
| Onset of tolerance | 2 days | 6 days | 6 days |
| Diet at 15 days (None/SL/Normal) | 1/2/3 | 2/5/2 | 0/1/6 |
ASA: American Society of Anesthesiologists; M: Males; F: Females; SL: semi-liquid diet.
Patients were included who had been diagnosed with unresectable gastric cancer with clinical data of gastric obstruction, and defined as patients presenting with advanced, unresectable gastric cancer greatly exceeding the pylorus and the first duodenal portion, with spread to neighbouring and vascular structures or with distant metastasis, originating in the distal gastric third (antropyloric region) associated with nausea, vomiting and digestive intolerance.
Intake was assessed from its onset and at 15 days from the date of the procedure using the following scale: 0: no diet, 1: semi-liquid diet, 2: puréed or normal diet based on the scale of gastric obstruction.
Pancreatic-duodenal tumours, recurrent gastric tumours and patients who had been fitted with a gastroduodenal stent prior to surgery were excluded.
The results were analysed statistically using the Student's t test for independent variables.
Surgical technique- 1)
In group I the stent was placed under sedation; this was a self-expandable metallic stent in the antroduodenal region (Wallstent Boston Scientific™).
- 2)
A routine gastrojejunostomy was performed in group II, manual transmesocolic wherever possible, in the free gastric portion plus the dependent portion in order to enable gastric emptying.
- 3)
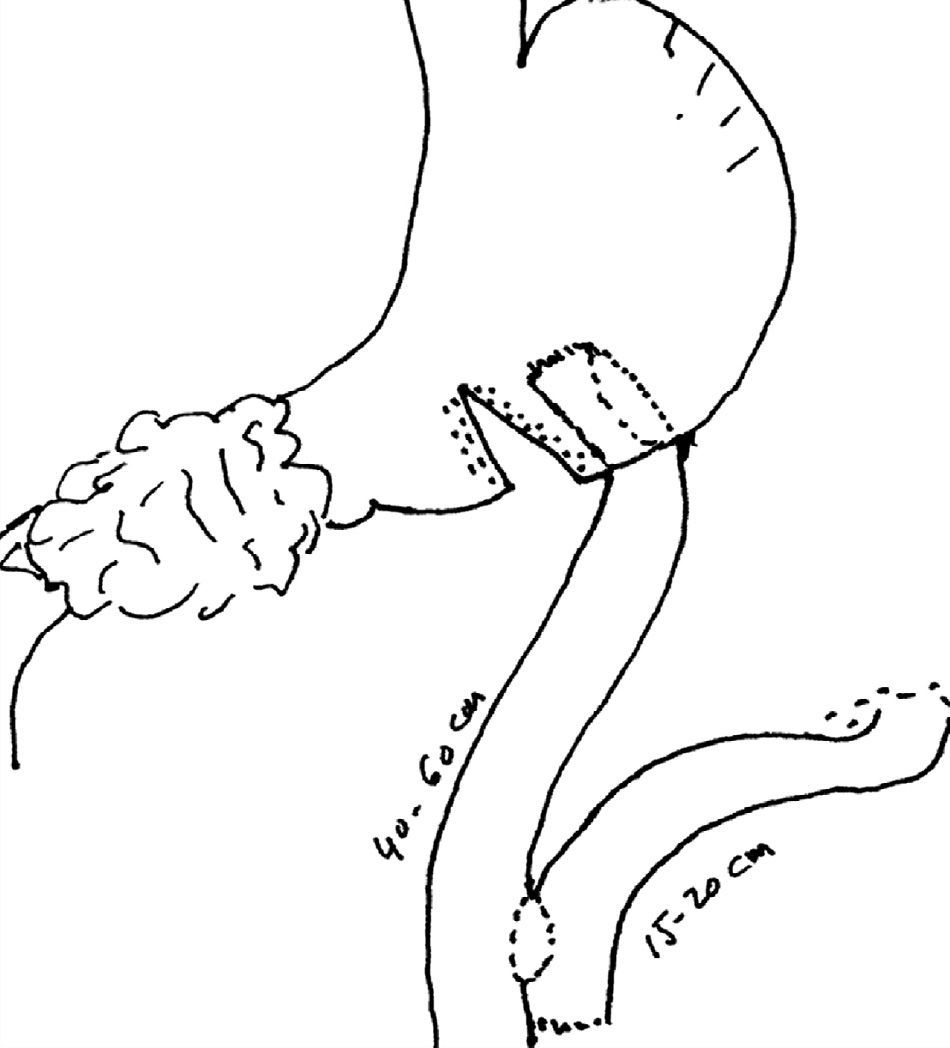
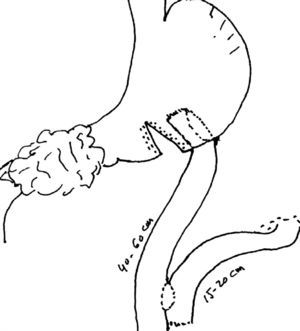
In group III the partial stomach-partitioning gastrojejunostomy was performed via a limited supraumbilical midline laparotomy of less than 10cm. After freeing and sectioning the gastroepiploic ligament in the greater gastric curvature, proximal and near to the tumour, the stomach was partially divided using an EndoGIA 60mm stapler towards the lower curvature leaving a distance of 3cm. The tract was reconstructed using (transmesocolic or anticolic) latero-lateral Roux en Y technique in the posterior gastric wall at 2cm from the proximal branch, parallel to the inverted V, and the foot of the loop was made using an EndoGia 35mm vascular stapler (Fig. 1).
At the end of this procedure we also placed a double-lumen naso-gastrojejunal tube with gastric aspiration (Compact® Stay-put 9/18FR Nestlé Health Care Nutrition) for early postoperative enteral feeding.
Neither conventional nor partial stomach-partitioning gastrojejunostomies were ever performed on macroscopic tumour tissue.
ResultsThe clinical characteristics of the 22 patients and their distribution into the different groups are summarised in Table 1, 16 men and 6 women, with an average age of 74. Table 1 also shows the demographic results and the most relevant data of the groups, and it can be observed that there are no significant differences in terms of age, gender and the American Society of Anesthesiologists between the groups.
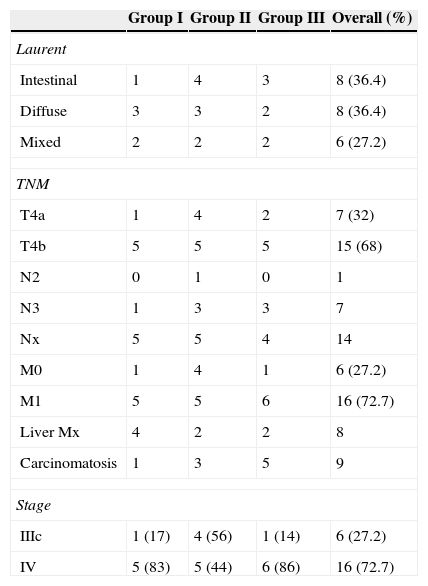
Table 2 shows the groups’ anatomopathological characteristics and tumour stage. The histological type according to Laurent's classification shows a homogeneous distribution between the groups, 36.4% being intestinal and the same percentage in the diffuse ones. Of the 22 patients, 16 (72.7%) presented distant disease at the time of intervention and were at stage IV, and locoregional involvement of the tumour was so extensive in 6 (27.2%), stage IIIc, it was considered unresectable; this circumstance occurred in 56% of the patients in group II, whereas in group I and group III it occurred in 17% and 14% respectively.
Histological characteristics and tumour stage.
| Group I | Group II | Group III | Overall (%) | |
|---|---|---|---|---|
| Laurent | ||||
| Intestinal | 1 | 4 | 3 | 8 (36.4) |
| Diffuse | 3 | 3 | 2 | 8 (36.4) |
| Mixed | 2 | 2 | 2 | 6 (27.2) |
| TNM | ||||
| T4a | 1 | 4 | 2 | 7 (32) |
| T4b | 5 | 5 | 5 | 15 (68) |
| N2 | 0 | 1 | 0 | 1 |
| N3 | 1 | 3 | 3 | 7 |
| Nx | 5 | 5 | 4 | 14 |
| M0 | 1 | 4 | 1 | 6 (27.2) |
| M1 | 5 | 5 | 6 | 16 (72.7) |
| Liver Mx | 4 | 2 | 2 | 8 |
| Carcinomatosis | 1 | 3 | 5 | 9 |
| Stage | ||||
| IIIc | 1 (17) | 4 (56) | 1 (14) | 6 (27.2) |
| IV | 5 (83) | 5 (44) | 6 (86) | 16 (72.7) |
None of the patients received neoadjuvant treatment; however, they had presented with obstructive syndrome from the outset or had received palliative adjuvant treatment and presented progression of the disease. Fifteen (68%) patients received chemotherapy subsequently, of the 7 (32%) patients who were not given chemotherapy 3 were from group I and group II respectively, and one from group III.
When the results of the techniques were assessed it was shown that the stent resulted in a shorter postoperative stay and earlier onset of oral tolerance (p<0.05) compared to the other techniques. In relation to the type of diet after 15 days, we found significant differences with partial stomach-partitioning gastrojejunostomy where a more complete diet was achieved after 15 days and with greater frequency (p<0.05).
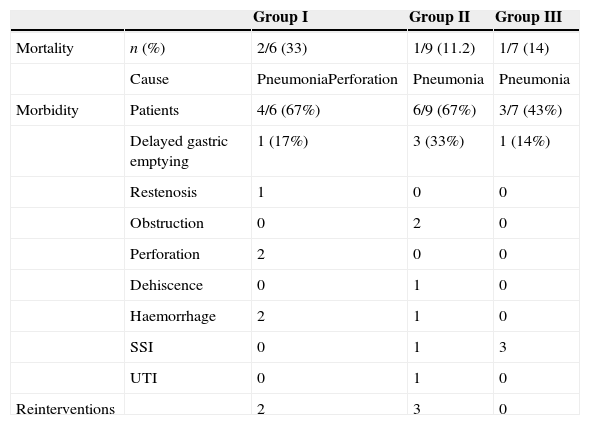
With regard to the complications which are summarised in Table 3, we observed that mortality was greater in the patients treated in group I (33%) 2/6, compared to those treated in group II (11.2%) 1/9, and to those of group III (14%) 1/7 respectively. In the surgical groups mortality was due to medical complications. Early morbidity was less frequent and severe than in group III; principally due to surgical site infection. Delayed gastric emptying presented more frequently in group II (33%).
Complications between the different groups.
| Group I | Group II | Group III | ||
|---|---|---|---|---|
| Mortality | n (%) | 2/6 (33) | 1/9 (11.2) | 1/7 (14) |
| Cause | PneumoniaPerforation | Pneumonia | Pneumonia | |
| Morbidity | Patients | 4/6 (67%) | 6/9 (67%) | 3/7 (43%) |
| Delayed gastric emptying | 1 (17%) | 3 (33%) | 1 (14%) | |
| Restenosis | 1 | 0 | 0 | |
| Obstruction | 0 | 2 | 0 | |
| Perforation | 2 | 0 | 0 | |
| Dehiscence | 0 | 1 | 0 | |
| Haemorrhage | 2 | 1 | 0 | |
| SSI | 0 | 1 | 3 | |
| UTI | 0 | 1 | 0 | |
| Reinterventions | 2 | 3 | 0 |
SSI: surgical site infection; UTI: urinary tract infection.
Five patients were reoperated: 3 (33%) patients from group II (one due to anastomotic dehiscence and the other two due to obstruction of the afferent loop) and 2 (33%) patients in group I: one case as a consequence of duodenal perforation and the other due to restenosis and perforation secondary to the restenosis. None of the patients in group III, required reintervention (Table 3).
Mean survival was 2.5 (0.5–6) months in group I, 3 (0–6) months in group II and 6.5 (0.5–20) months in group III, with no statistically significant value.
DiscussionPalliative surgery (gastric resection) for incurable stomach cancer depends on the general condition of the patient and the extent of progression of the cancer, it has been estimated that in 5–31% of patients with stomach cancer it is not possible to resect the primary lesion1; moreover when it presents as secondary obstruction syndrome, it is associated with spread to neighbouring organs in 47%, with lymph node involvement in 93%, carcinomatosis in 34% and with 15% liver metastases.3 These percentages are higher in our series, 41% carcinomatoses and 36% liver metastases. Routine treatment is conventional gastrojejunostomy which has the drawback that 10% to 50% of patients present significant delayed gastric emptying7,11,12 (33% in our experience).
In 1925, Devine13 introduced gastrojejunostomy with antral exclusion for the treatment of unresectable duodenal ulcer, which was subsequently applied to unresectable cancerous gastroduodenal lesions with the following benefits: making an anastomosis far from the primary tumour to isolate the tumour from food and acid in order to reduce the possibility of bleeding.14 The disadvantage of this technique was the need to decompress the isolated antrum with a probe.
In 1997, Kaminishi et al.9 modified Devine's technique, describing partial stomach-partitioning gastrojejunostomy to achieve minimal contact of food and gastric acid with the tumour, as well as improving gastric emptying, and enabling endoscopic assessment of the lesion.
In this article we present our experience with partial stomach-partitioning gastrojejunostomy as described by Kaminishi et al.9 modified, performing a termino-lateral gastrojejunostomy on the posterior wall, in the proximal portion of the gastric channel and a termino-lateral Roux en Y anastomosis at the foot of the loop (Fig. 1). The reason for modifying the original technique is to reduce the blind loop effect in the afferent loop of the gastrojejunostomy and enable gastric emptying. Several published studies indicate that the use of Roux en Y loop minimises delayed gastric emptying and reduces the postoperative hospital stay.15
Our results show fewer cases of delayed gastric emptying in group III (14%) compared to group II (33%) and group I (17%).
As demonstrated in other studies,9,16 the stent achieves a similar percentage of success in resolving symptoms and they coincide with our results in that this group of patients presented a shorter hospital stay and more rapid onset of oral tolerance (p<0.05) in comparison with the surgical techniques; but we observed in this study that the stent results are not maintained over time, as only 50% of cases tolerated a complete diet after 15 days. These results have also been described in other studies, where this technique is associated with more long-term complications, these include lower duration of the permeability of the prosthesis even when an additional one is placed, and lower survival, especially in patients with a better general condition11. This coincides with our results in that the patients of group I had greater mortality compared to the groups using surgical techniques (group II and group III).
In our opinion, this technique should be reserved for patients with a poor clinical situation and poor overall prognosis, whereas patients with a better clinical condition should be offered gastric bypass surgery. This opinion is shared by other authors, who recommend that a stent should be used when the patient's life expectancy is less than 2 months.3,17
Most publications which compare stents with gastrojejunostomy do not specify the type of surgical bypass performed in surgical patients, and they include patients with symptoms of gastric obstruction secondary to a cancer, but the origin of the primary tumour is variable, principally pancreatic, which has a poorer prognosis.11,18
Our results show that partial stomach-partitioning gastrojejunostomy ensures that the diet of these patients at 15 days is more complete, with greater frequency (85%) (p<0.05); this fact is related, as observed by Kubota et al., 19 to better quality of life and a better prognosis.
Onset of tolerance was on the sixth postoperative day with the surgical techniques. In group III we thought that onset of tolerance was delayed through the routine use of a double-lumen naso-gastrojejunal tube with gastric aspiration (Compact® Stay-put 9/18FR Nestlé HealthCare Nutrition) and early postoperative enteral feeding.
We have seen how with partial stomach-partitioning gastrojejunostomy fewer overall complications tend to develop, and they are less severe, there is less need for reintervention and there is even better survival than with the other 2 techniques, although with no significant differences. Okumura et al.3 achieved a mean overall survival of 8.8 months in 25 patients with obstructive gastric cancer treated with partial stomach-partitioning gastrojejunostomy, and this directly related with the presence of complications and the lack of chemotherapy treatment; patients with complications are often not given chemotherapy. Our mean survival was 6.5 months in group III.
We must state that this study is limited by the reduced number of patients in the different groups, but this is a consequence of the small percentage of patients with these circumstances; obstruction secondary to antropyloric adenocarcinomas which are unresectable is rare; in the series of Okumura et al.3 they comprised 6.3% of all the gastric cancers treated over 11 years. In the systematic review which was undertaken by Zheng et al.18 from 1996 to 2010, the cases of gastric cancer with these characteristics did not exceed 10 patients and this is reflected in this study after collecting cases retrospectively over 12 years. Remember that only patients with gastric cancer were included in the study, in order to be more homogeneous, although this technique can also be applied to duodenal and pancreatic tumours.6,20,21
In conclusion, partial stomach-partitioning gastrojejunostomy for the treatment of gastric obstruction in advanced, unresectable gastric cancer is a technique which is at least as safe as the compared techniques (conventional gastrojejunostomy and stent), and also allows a more complete diet in a greater number of patients with lower morbidity and better survival, and therefore should be the most appropriate technical option for patients with obstructive symptoms secondary to unresectable gastric cancer with an acceptable clinical situation and better prognosis.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Abdel-lah-Fernández O, Parreño-Manchado FC, García-Plaza A, Álvarez-Delgado A. Gastro yeyuno anastomosis con separación gástrica parcial en el tratamiento de la obstrucción gastroduodenal secundaria a cáncer gástrico avanzado. Cir Cir. 2015;83:386–392.