Attempts are being made in recent years to replace open surgery with endoscopic techniques in some obese patients when medical treatment fails, as they are considered to be less-invasive procedures. To date, there is little scientific evidence regarding their effectiveness.
Clinical casesThe cases are reported of 2 patients who attended our surgery looking for an effective bariatric surgical treatment after failed endoscopic sleeve gastroplasty.
ConclusionsLaparoscopic sleeve gastrectomy after failure of an endoscopic technique does not offer great variation from the standard technique.
Durante los últimos años, las técnicas endoscópicas intentan sustituir a la cirugía en algunos pacientes con obesidad, cuando el tratamiento médico fracasa, basándose en que son técnicas menos agresivas. Hasta la fecha, existe muy poca evidencia científica de su efectividad.
Casos clínicosPresentamos 2 casos de pacientes intervenidos mediante gastroplastia vertical endoscópica que, tras su fracaso, acuden en busca de un tratamiento quirúrgico bariátrico efectivo.
ConclusionesLa gastrectomía vertical laparoscópica tras el fracaso de una técnica endoscópica no supone una gran variación sobre la técnica estándar.
Attempts have been made in recent years to replace open surgery with endoscopic techniques in some morbidly obese patients, as they are considered to be less-invasive, reversible and less costly procedures.1,2 Among these techniques is endoscopic sleeve gastroplasty, a novel alternative, which attempts to improve the outcome of the Primary Obesity Surgery Endolumenal procedure (POSE), by deploying continuous suture to mould the stomach into a tube shape. This is an overstitch suture system (Apollo Endosurgery) which is fitted over the end of the endoscope and which, after being orally inserted, reduces the stomach by trying to imitate a laparoscopic sleeve gastrectomy through a series of transmural stitches from the gastric lumen, following a hands free technique and placing the stitches very close to one another, from the prepyloric antrum up to the gastroesophageal junction. The POSE, in contrast, folds the stomach in 8–9 locations in the fundus, and 3–4 in the antrum, with specific loose stitches. Supposedly, the resulting plicature using these new techniques leads to greater gastric reduction and at the same time produces a slowdown of gastric emptying, helping to produce a satiating effect.3,4
ObjectiveWe present the cases of 2 patients, on whom the Apollo technique was used and who, after one year of follow-up and failure of quantifiable results, sought a surgical solution.
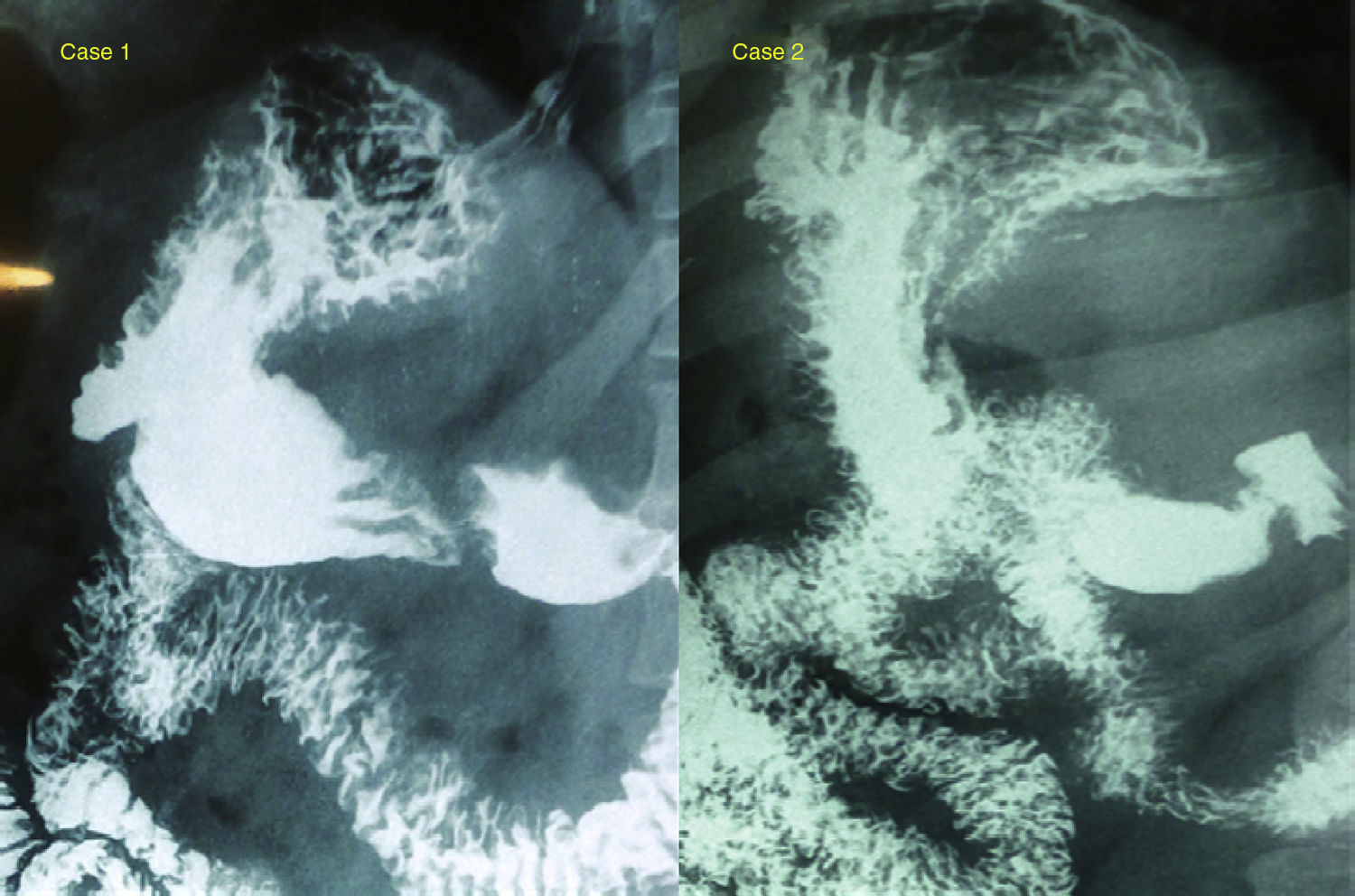
Clinical casesCase 1A male patient aged 37, with a body mass index (BMI) of 42kg/m2 and obstructive sleep apnoea syndrome, on whom 7 months previously the Apollo technique had been used for gastric reduction, without incident. The patient presented with a quantifiable weight gain of 9kg during the following 7 months and therefore attended our surgery in search of a solution. After a complete study by our multidisciplinary team, which included a gastroduodenal radiologic study that reported him as having a “normal stomach” (Fig. 1), laparoscopic sleeve gastrectomy surgery was performed on the patient.
Esophageal and gastroduodenal transit. Case 1: regular stomach walls, with no excess images, defect or extrinsic compressions; no signs of reflux or hiatus hernia. Emptying without incident. Case 2: regular stomach walls, with no excess images, defect or extrinsic compressions; no signs of gastroduodenal reflux or hiatus hernia.
A female patient aged 33, with a BMI of 45 and no comorbidities, into whom 30 months previously an intragastric balloon (for 6 months) had been inserted but without any outcome. After this (13 months later) the Apollo technique for gastric reduction was practised. One year after this technique, the patient was 14kg heavier than the day of the operation and she therefore attended our surgery to be treated for her obesity. Following a complete multidisciplinary study, which included a gastroduodenal radiologic study that reported her as having a “normal stomach” laparoscopic sleeve gastrectomy surgery was scheduled.
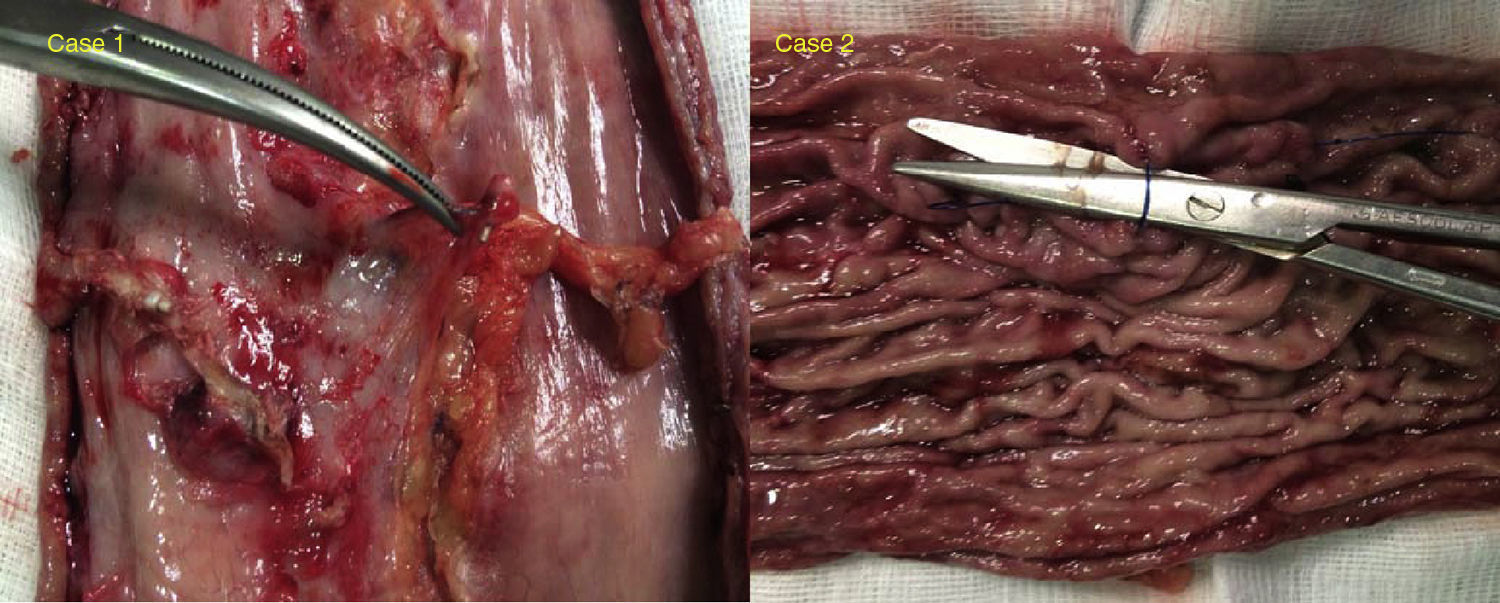
During surgery on both patients adhesions to the parietal peritoneum, liver, and the pancreatic body were observed. These were released to continue the surgical procedure. During the dissection of increased curvature, there was some digitation which corresponded to the endoscopic suture, but no plicature or torsion imaging was observed, with the exception of the above-mentioned adhesions and several areas of thickening (the above-mentioned digitation mainly referred to in the antrum). The impression was that of finding a practically normal stomach. Surgery was performed by completing dissection to the angle of His and performing the gastrectomy with staples, reinforced with 2.0 barbed sutures. There were no difficulties during the operations that differed from a patient who had not previously had gastric surgery. Examination of the extracted specimen revealed several slightly folded areas (in fundus and antrum), with no obvious reduction of gastric capacity (Fig. 2). The patients were discharged from hospital 36h after surgery without incident. During follow-up the patients lost weight at a normal post-bariatric surgery rate without any presence of complications. After one year of follow-up the percentage of excess BMI lost was 62% and 73% respectively.
DiscussionThe development of new endoscopic techniques and improvements in the designs of existing ones has meant that during recent years, the procedures using this route have attempted to replace surgery for some patients with obesity when medical treatment fails. Rejection of surgery or contraindications, excessive risk or the presurgical period to reduce morbidity in surgery may be some of the situations where these systems would be indicated. The suture systems (POSE, TOGa, Apollo, etc.) form a considerable number of endoscopic techniques which during recent years have reproduced the manipulations and physiological effects minimally invasive surgery has on the treatment of morbid obesity.1,5 They try to reduce the stomach's ability to store food, thus inducing early satiety, and delay gastric emptying by applying folds in the stomach wall.
Until now, only one study has been published by Espinós et al.6 which included 45 obese patients with a mean BMI of 36.7, where the follow-up was a mere 6 months. They present a reduction of BMI of 5.8 (31.3) and a SPSS of 49.4%. They conclude that the POSE appears to be a safe and effective procedure with regards to weight loss, no pain, scarring and recovery from surgery. Vilallonga et al.7 in their response to the before-mentioned article, are aware of the scarcity of publications which appear to defend the efficacy of fundus plicature or even gastric antrum plicature, which supposedly activates satiety receptors or slows down gastric emptying. They believe that the mechanisms relating to satiety, motility or even gastric volume are complex and cannot simply be explained by an unquantifiable reduction of the gastric fundus.
López-Nava et al.8 recently published their results in a series of 20 patients with a follow-up of 6 months after endoscopic sleeve gastroplasty. They report a preoperative and follow-up BMI of 35.6 and 31.9kg/m2, respectively.
Deitel and Greeinstein9 propose the use of the lost BMI percentage to evaluate results, so much so that they consider it an excellent result if there is over 65%, a good result if it is between 50% and 65% and a failure when it is below 50%. None of the studies mentioned use this formula to assess outcome. Furthermore conclusions cannot be reached with such small cohorts and a follow-up of only 6 months. Randomised, controlled and well-designed studies are needed to determine the efficacy and safety both in the short and long term.
As studies on laparoscopic sleeve gastrectomy have been published which report a slight swelling of the gastric tube one year after surgery, so too should studies be carried out to show what the outcome of gastric plicature with the endoscopic techniques would be in the mid to long term, either through further endoscopies or with barium transit tests.10 The increased pressure maintained over the gastric tube could lead to failure of the technique through the opening of the sutures, without the patient showing any signs of complications. This was such in the presented cases as both patients practically presented with an opening the length of the gastroplasty suture.
ConclusionsIt is possible that we will increasingly find more patients for whom treatment of this type has failed and they will come looking for a definitive solution to their weight loss. As we have shown with these two cases, laparoscopic sleeve gastroplasty after the failure of an endoscopic technique does not offer great variation from the standard technique. However, we would recommend a careful, meticulous technique since the percentage of complications could rise in these patients, similarly to revision surgery. Adhesions should therefore be released to maintain normal gastric anatomy, and fibrous, swollen areas should be located to avoid sectioning in this region, as much as possible. Although it has not been demonstrated that the risk of fistulas is reduced, we would recommend enhancement with suturing in the section line in this type of patient.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Ferrer-Márquez M, Ferrer-Ayza M, Rubio-Gil F, Torrente-Sánchez MJ, Martínez Amo-Gámez A. Revisión quirúrgica bariátrica tras gastroplastia vertical endoscópica. Cir Cir. 2017;85:428–431.