The rheumatoid arthritis is a clinical entity capable to cause hearing impairment that can be diagnosed promptly with high frequencies audiometry.
ObjectiveTo detect subclinical sensorineural hearing loss in patients with rheumatoid arthritis.
Material and methodsCross-sectional study on patients with rheumatoid arthritis performing high frequency audiometry 125Hz to 16,000Hz and tympanometry. The results were correlated with markers of disease activity and response to therapy.
ResultsHigh frequency audiometry was performed in 117 female patients aged from 19 to 65 years. Sensorineural hearing loss was observed at a sensitivity of pure tones from 125 to 8000Hz in 43.59%, a tone threshold of 10,000 to 16,000Hz in 94.02% patients in the right ear and in 95.73% in the left ear. Hearing was normal in 8 (6.84%) patients. Hearing loss was observed in 109 (93.16%), and was asymmetric in 36 (30.77%), symmetric in 73 (62.37%), bilateral in 107 (91.45%), unilateral in 2 (1.71%), and no conduction and/or mixed hearing loss was encountered. Eight (6.83%) patients presented vertigo, 24 (20.51%) tinnitus. Tympanogram type A presented in 88.90% in the right ear and 91.46% in the left ear, with 5.98–10.25% type As. Stapedius reflex was present in 75.3–85.2%. Speech discrimination in the left ear was significantly different (p=0.02) in the group older than 50 years. No association was found regarding markers of disease activity, but there was an association with the onset of rheumatoid arthritis disease.
ConclusionsPatients with rheumatoid arthritis had a high prevalence of sensorineural hearing loss for high and very high frequencies.
La artritis reumatoide es una entidad clínica capaz de ocasionar hipoacusia neurosensorial, pudiendo ser diagnosticada oportunamente con audiometría de altas frecuencias.
ObjetivoDetectar hipoacusia neurosensorial subclínica en pacientes con artritis reumatoide.
Material y métodosEstudio transversal en pacientes con artritis reumatoide, donde se realiza audiometría de hasta altas frecuencias de 125-16,000Hz y timpanometría. Los resultados fueron correlacionados con marcadores de actividad de la enfermedad y la respuesta al tratamiento.
ResultadosSe realizó audiometría particularmente de altas frecuencias en 117 pacientes femeninas con edad de 19-65 años. La hipoacusia neurosensorial fue observada a una sensibilidad de tonos puros de 125-8000Hz en el 43.59% y umbrales de tonos de 10,000-16,000Hz en el 94.02% de los pacientes en oído derecho y en el 95.73% en oído izquierdo. Audición normal en 8 (6.84%) pacientes, hipoacusia en 109 (93.16%), asimétrica en 36 (30.77%), simétrica en 73 (62.37%), bilateral en 107 (91.45%) y unilateral en 2 (1.71%); no encontramos hipoacusia de conducción o mixta. Ocho (6.83%) pacientes cursaron con vértigo, 24 (20.51%) con tinitus. Timpanograma tipo A presente en el 88.90% en oído derecho y en el 91.46% en oído izquierdo, el 5.98-10.25% tipo As; reflejo estapedial en el 75.3-85.2%. Hubo diferencia significativa (p=0.02) en discriminación del lenguaje en oído izquierdo en mayores de 50 años. No encontramos asociación con marcadores de actividad de la enfermedad. Se observó asociación con el inicio de la artritis reumatoide.
ConclusionesLos pacientes con artritis reumatoide tienen alta prevalencia de hipoacusia neurosensorial para altas frecuencias.
Autoimmune sensorineural hearing loss or immune-mediated inner ear disease was described by McCabe in 1979 and has been the subject of clinical and experimental research over the last 2 decades.1,2 It presents in under 1% of all auditory and vestibular impairment; it is characteristically bilateral, fluctuating and progressive over weeks or months, and responds to corticosteroids.3
Several tests which detect auto-antibodies and specific antibodies against inner ear cochlear membrane antigens have been described, with somewhat unsatisfactory study results.4–6 No tests were conducted in this study as it was considered that the ability to detect early sensorineural hearing loss with very high frequency audiometry could be relevant. Since vestibular tests were non-specific for autoimmune problems, they were not included in this study.
Rheumatoid arthritis is a chronic inflammatory disease characterised by oedema and destruction of the joint's synovial membrane, leading to severe disability and premature death.7 Extra-articular manifestations of rheumatoid arthritis include: skin, eyes, heart, lung and hearing alterations leading to sensorineural hearing loss through inner ear involvement up to 24–60% in high frequencies of 6000–8000Hz.8 Due to it being an auto-immune disorder, one extra-articular manifestation can be sensorineural hearing loss.9 it is frequently taken for granted that the patient requires several drugs which could be potentially ototoxic.10 Inflammatory arthritis of the incudostapedial and incudomalleolar joint may present in the middle ear causing stiffness in the sound transmission mechanism.11
Öztürk et al.12 demonstrated that sensorineural hearing loss presenting in patients with rheumatoid arthritis is significant in high frequencies, associating it with neuritis, vasculitis, ototoxicity of medication used for the rheumatoid arthritis and the length of the disease.
The aim of our study was to conduct audiometric assessment of the cochlear function as a whole and more specifically in high frequencies in a female population with rheumatoid arthritis. The references contain reports on studies conducted with conventional audiometry tests which fail to measure thresholds of 10,000–16,000Hz and are unable to detect the existence of injury in this area of the cochlear when it is possible that early detection may alter its development, as reported by Conway et al.13 Our study also aimed at describing the characteristics and severity of sensorineural hearing loss and its subsequent risk factors whilst playing a part in early subclinical detection of hearing loss.
Material and methodsAn observational, cross-sectional and analytical study was conducted in an exclusively female population of 117 patients aged between 19 and 65 who had been diagnosed with rheumatoid arthritis, according to the internationally consensured project criteria, also known as EULAR/ACR 2010 (aimed at standardising epidemiological therapeutic criteria and results) in the Rheumatology and ENT Services of the University Hospital. Although the study was conducted in an open population of 119 patients, only 2 were male and it was therefore decided to exclude them from the study. A complete medical history and thorough physical examination were made, and the following patients were excluded from the study: those with a history of hearing loss under 24h; those who presented with barotrauma, brain trauma or otic trauma; those diagnosed with Meniere's disease, acoustic trauma, otosclerosis, chronic otitis media, presbycusis, exposure to ototoxic medication, chronic exposure to intense noise, cardiovascular disease or chronic neurological disease. Clinical and demographic characteristics and disease activity were taken from the medical records, along with age, how long they had been diagnosed with rheumatoid arthritis, treatment and current dosage; number of inflamed, painful joints; visual analogue scale: speed of globular sedimentation; rheumatoid factor: C-reactive protein and presence of anti-CCP antibodies. All patients were also in possession of clinical hearing records and both tympanic membranes presented as normal under examination.
The control group consisted of 75 volunteers with a similar age and gender distribution, who presented without pathology in the hearing examination, as normal during tympanometry and who were without occupational noise exposure.
Hearing testThe audiometric study was carried out with an Acoustic Systems soundproof camera, model RE-142 manufactured in U.S.A., and (Interacustic AC40) audiometry and (Audiotest 425h Interacustic) tympanometry which measured air conduction thresholds at 125–16,000Hz frequencies and bone conduction thresholds at 500–4000Hz frequencies. Pure-tone speech audiometry was used measuring speech discrimination thresholds (speech audiometry) and word recognition. Tympanometry with acoustic reflex and static acoustic compliance for both ears was used.
Normal hearing was defined as the limit of perception under 20 decibels (dB) at all frequencies and also the type of auditive threshold and verbal discrimination according to the classification by the American Academy of Otolaryngology Committee on Hearing and Equilibrium.14 60dB was accepted as the maximum hearing loss threshold at 16,000Hz. Tympanometry was considered normal with middle ear pressures of ±75daPa (deca Pascal: unit of pressure), compliance at 0.28–1.5ml, and acoustic reflex was considered normal when it occurred with stimulation at 70–95dB in 500; 1000; 2000; and 4000Hz.
Statistical analysisResults were collected on an Excel database programme, with analysis performed using the IBM SPSS 20 programme. The p<0.05 value was considered significant. From all the variables assessed traditional descriptive statistics such as measures of central tendency, dispersion and position in the case of quantitative variables and measures of observed frequencies in qualitative type variables were obtained. Study values were segmented according to the presence or absence of hearing loss, contrasted using hypothesis testing for means and proportions, depending on the case for each type of variable (quantitative and qualitative, respectively) at a confidence level of 95%; determination of association, correlation and risk was determined by χ2, Pearson or Spearman at the same confidence level.
The study was submitted to the Committee for Ethics and Research of the University Hospital and registered with the key OT13-005; no conflict of interests arose.
ResultsThe group under study comprised a female population of 117 patients (234 hearing tests were carried out) aged between 19 and 65 (with a mean age of 47.49±11.25), and in 8 (6.84%) patients hearing was normal. Sensorineural hearing loss was observed at high frequencies in 109 (93.16%) patients; a prevalence of sensorineural hearing loss was noted for frequencies of up to 8000Hz in 43.59% and for high frequencies in 94.02%, with frequencies at 10,000–16,000Hz having the highest effect. When the study took place 103 (88%) patients were being treated with methotrexate, 63 (53.8%) with hydroxychloroquine and only 37 (31.6%) with prednisone. Length of exposure to medication was reviewed in the medical records in order to assess the risk of ototoxicity and no administration of salicylates was noted.
Eight (6.84%) patients presented with vertigo, and 24 (20.5%) with tinnitus, with a bilateral predominance; with respect to disease activity, 63.2% (74 patients) presented a DAS28 over 2.5 and 34.2% below this figure. The joints of 58.1% of patients were affected, 41.9% in more than 2 major joints, 17.9% in 1–3 minor joints and 8.5% in 4–10 joints. 37.6% of the group studied had suffered from joint symtomatology for under 5 years and 61.4% for over 6 years.
Among the hearing characteristics in our study group we observed normal hearing as below 20dB in only 8 patients (6.84%), 109 (93.16%) had sensorineural hearing loss without conductive system components, with a recording of a higher effect at high frequencies; there was a symmetrical sensorineural hearing loss in 73 patients (62.37%), and an asymmetrical sensorineural hearing loss in 36 (30.77%) patients. Of the 109 patients with sensorineural hearing loss, 2 (1.71%) presented with unilateral sensorineural hearing loss and 107 (91.45%) with bilateral.
The mean age of the 8 patients with rheumatoid arthritis with normal hearing was 25.6 whilst the mean age of those over 31 (109 patients) with sensorineural hearing loss was 39.9 (p<0.0001).
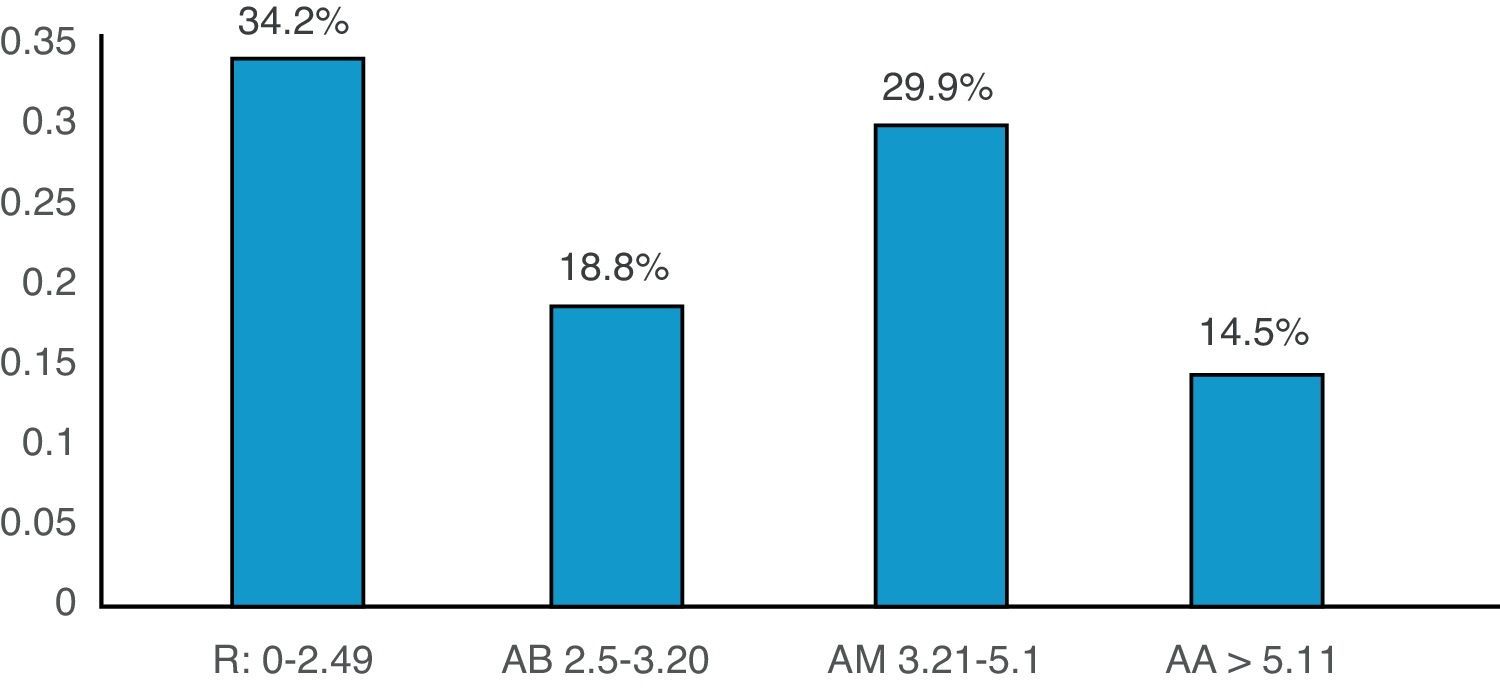
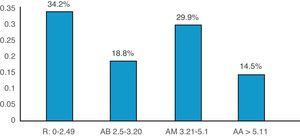
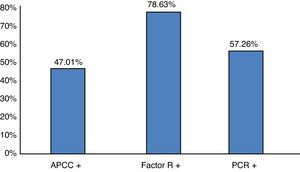
Patients were divided into 3 age groups for the study (under 30, from 31 to 50 and from 51 to 65 years of age), and analysis was conducted of their association or correlation with the duration of their rheumatoid arthritis, body mass index, disease activity score (Fig. 1), presence of anti-CCP antibodies, rheumatoid factor, C-reactive protein (Fig. 2), ESR rate, and blood sugar level. No significant differences were found.
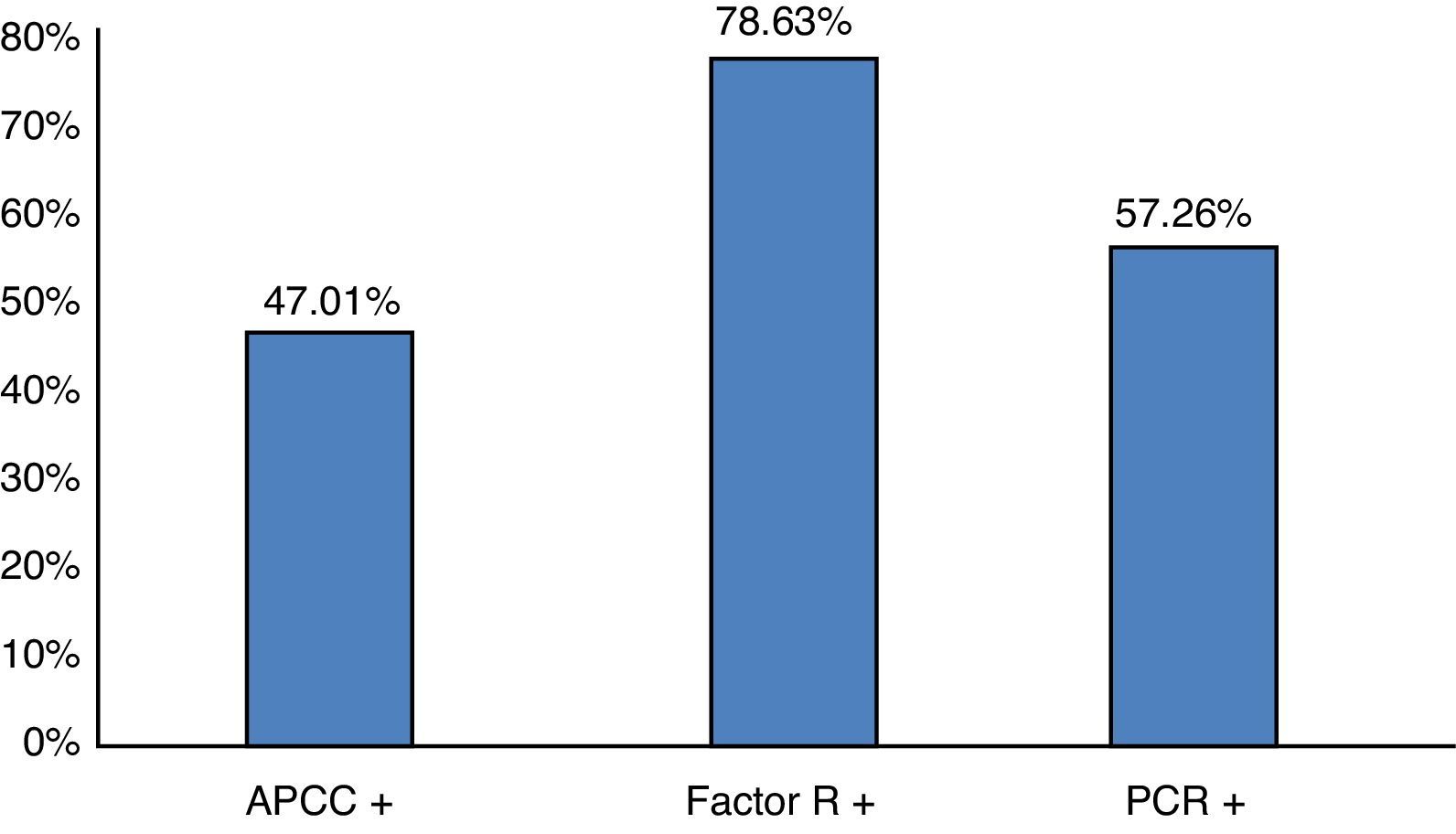
Percentage distribution of the population under study according to positive results in the serological assessment of rheumatoid arthritis activity. CCAB: cyclic citrullinated antipeptide antibody; RF: rheumatoid factor; CRP: C-reactive protein. n=117 patients. Source: clinical record. Gr.2.
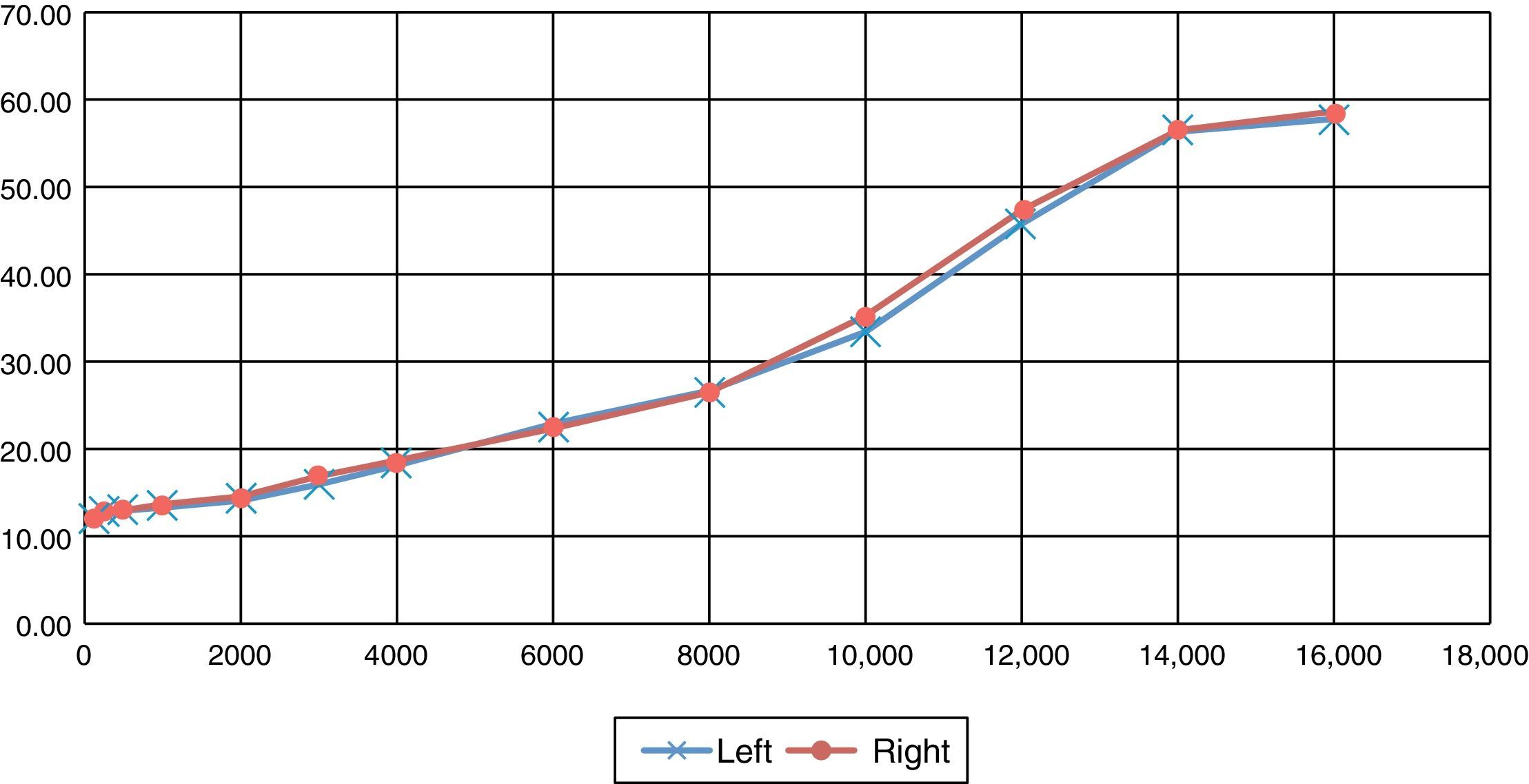
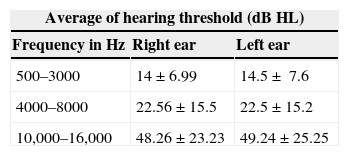
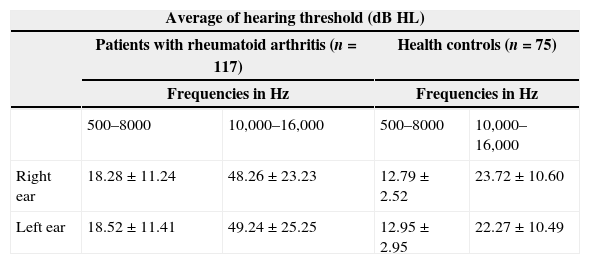
Hearing in both ears was compared at frequencies of 500–3000Hz, 4000–8000Hz and 10,000–16,000Hz with no significant differences being found and with standard averages and deviations in hearing thresholds within the normal limits at frequencies of 500–3000 and at 4000–8000Hz of 22.56±15.5 in the right ear and 22.5±15.2 in the left ear. The hearing threshold observed in frequencies at 10,000–16,000Hz was 48.26±23.23 in the right ear and 49.24±25.25 in the left ear, with hearing loss for these frequencies as observed in Table 1.
Averages and standard deviation in pure-tone audiometry tests in medium frequencies (500–3000Hz), high frequencies (4000–8000Hz) and very high frequencies (10,000–16,000Hz) in right and left ears of patients with rheumatoid arthritis.
| Average of hearing threshold (dB HL) | ||
|---|---|---|
| Frequency in Hz | Right ear | Left ear |
| 500–3000 | 14±6.99 | 14.5±7.6 |
| 4000–8000 | 22.56±15.5 | 22.5±15.2 |
| 10,000–16,000 | 48.26±23.23 | 49.24±25.25 |
Hearing thresholds were analysed for all patients with rheumatoid arthritis and health controls (mean age of 32.23±8.82), comparing the right ear with the left ear at tones of 500–8000Hz with no differences being observed; at frequencies of 10,000–16,000Hz there was a significant difference of p<0.0001 of greater hearing loss at high frequencies in patients with rheumatoid arthritis vs. health control group, as shown in Table 2.
And standard deviation in pure-tone audiometry tests in medium and high frequencies (500–8000Hz) and very high frequencies (10,000–16,000Hz) in right and left ears in patients with rheumatoid arthritis and health controls.
| Average of hearing threshold (dB HL) | ||||
|---|---|---|---|---|
| Patients with rheumatoid arthritis (n=117) | Health controls (n=75) | |||
| Frequencies in Hz | Frequencies in Hz | |||
| 500–8000 | 10,000–16,000 | 500–8000 | 10,000–16,000 | |
| Right ear | 18.28±11.24 | 48.26±23.23 | 12.79±2.52 | 23.72±10.60 |
| Left ear | 18.52±11.41 | 49.24±25.25 | 12.95±2.95 | 22.27±10.49 |
t Student test p<0.0001.
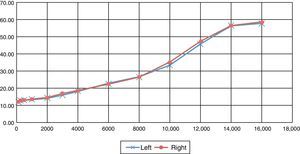
The hearing threshold was measured and compared in frequencies of 125 up to 16,000Hz in patients with rheumatoid arthritis, with no significant differences being found in the hearing levels of each ear (p>0.05). In the middle ear we measured the average, median and range of levels of static compliance with a reporting of 0.77±0.52ml in the right ear and 0.78±0.57ml in the left ear with no significant difference between both ears; in the group over 50 years of age a significant difference of p<0.02 was found in the right ear in the discrimination percentage in both ears per age group.
Tympanometry of the right ear showed a curve A in 91.46% and in the left ear a curve A in 88.90% of patients; As (A short) in the right ear of 5.98% and of 10.25% in the left ear; Ad (A deep) in the right ear of 2.56% and 0.85% in the left ear; there were no patients with curve B in our study. Auditory reflex was present in the right ear in 85.2% of patients and in the left ear in 75.3% of patients, and was only absent in 14.8% and in 24.7% respectively in our group studied. We believe that rheumatoid arthritis involves the transmission mechanisms of the ossicular chain.
DiscussionKastanioudakis et al.15 reported that sensorineural hearing loss is mainly observed at low and medium frequencies, whilst it may be associated with high frequencies when vasculitis is present in its ethioipathogenesis. García Callejo16 and Halligan et al.17 reported a prevalence of sensorineural hearing loss in patients with rheumatoid arthritis of 42.7% and 45% with standard eudiometry testings for frequencies of up 8000Hz; in our study, similarly to the before-mentioned authors, we observed a prevalence of 43.59% at these frequencies, with a significant hearing loss in 95% of patients at frequencies of 10,000–16,000Hz. Hearing loss observed was greater than at 20dB, with loss being characteristically symmetrical and bilateral as shown in Fig. 3; it is possible that these results are due to the fact that the rheumatoid arthritis is systemic and affects both ears.
In our study, symptomatic sensorineural hearing loss was observed in 20.5% of the patients studied, comparable with the references. In our study 8 patients presented with vertigo (6.8%), 24 (20.5%) with tinnitus. This was bilateral in 14 (11.9%) and unilateral in 10 (8.5%). We did not find any cases of occular disease suggestive of Cogan syndrome.
Several authors describe sensorineural hearing loss, particularly at high frequencies.18 In our study we observed that sensorineural hearing loss was present at high frequencies. The hearing thresholds were compared from 125 to 16,000Hz measuring up to the limits of the audiometry, with mild hearing loss at thresholds of 4000–8000Hz (standard average and deviation of 22.56±15.5dB), compared with hearing thresholds at frequencies of 10,000–16,000Hz (48.26±23.23dB), with 43.6% of sensorineural hearing loss detected in conventional audiometry at thresholds of 125–8000Hz and 95.7% at thresholds of 10,000–16,000Hz. Hearing thresholds were compared at all frequencies in the right and left ear, with no statistically significant findings being found between the right and left ear. By age group, in patients under 30 years of age it was observed that with the conventional audiometry no sensorineural hearing loss was recorded, in contrast to the audiometry at high frequencies which detected hearing loss in 66.6% (7 patients) at that time; in the group aged between 31 and 50 sensorineural hearing loss was observed with conventional audiometry in 30.9% vs. high frequency audiometry in 96.3% (56 patients) and in the 51–65 age group with conventional audiometry in 64.15% vs. 98.1% (54 patients).
Although several authors highlight the sensorineural nature of the hearing loss, others consider the middle ear to be the primary disease target.19,20 Hüttenbrink21 refers to degenerative changes which have taken place in the incus and malleus joints and which may alter the ossicular function in response to pressure changes in the middle ear, with protection mechanisms possibly being reduced as a result.21–23 In our study the average, median and range of levels of static compliance were measured, reporting 0.77±0.52ml in the right ear and 0.78±0.57ml in the left ear without any significant difference between both ears. The As curve in the tympanogram reflects part of the functional status of the tympanic membrane and ossicular chain, which increases in patients with rheumatoid arthritis. In our results, the graph in the tympanometry revealed curve As only in 7 right ears (5.98%) and 12 left ears (10.2%), and curve A in 91.4% of right ears and 88.9% of left ears. Acoustic reflex was present in 99 right ears (85.2%) and 88 left ears (75.3%), absent in 18 right ears 14.8%) and 29 left ears (24.7%), which means that there are few patients with rheumatoid arthritis who present with involvement of the ossicular chain.
Other research studies reported a link between sensorineural hearing loss and disease activity24,25; in this study 78.3% had positive rheumatoid factors, 57.26% reactive-C protein, 47.01% presence of anti-CCP antibodies; DAS28 with low (34.2%), medium (28.8%), high (29.9%) and very high (14.5%) activity, with a limited value in the diagnosis of auto-immune disease of the inner ear and no statistical significance relating to sensorineural hearing loss (p>0.05).
In our study out of 117 patients, 103 (88.0%) were being treated with methotrexate, 63 (53.8%) with hydroxychloroquine and 64 (54.70) patients with both drugs. No significant ototoxicity relationship was found (p>0.05).
ConclusionsThe aim of this study was for early or subclinical identification of sensorineural hearing loss in patients with rheumatoid arthritis.
Sensorineural hearing loss observed in hearing thresholds at very high frequencies in our sample population was significantly high, compared with the thresholds below 8000Hz observed in the same patients with rheumatoid arthritis and the control group.
Our results demonstrate the usefulness of evaluating hearing at very high frequencies, for subclinical detection of any degree of alteration in the hearing in this patient group with rheumatoid arthritis. Since the findings from this study did not reveal any particular relationship with rheumatic disease activity or any difference in serological variables researched, the opportunity exists for the prediction and early treatment of some degree of cochlear injury prior to it becoming invasive, as development may be unpredictable; we therefore suggest further research be conducted.
We agree with the characteristics of sensorineural hearing loss in low tones observed in several conditions such as Meniere's disease. Patients with rheumatoid arthritis are referred for consultation with hearing loss, and sensorineural hearing loss in these patients is initially affected at very high frequencies, especially those above 10,000Hz. For this reason we recommend that patients with rheumatoid arthritis undergo examination aimed at discovering the presence of hearing loss and an audiometry test at high frequencies, thus providing early information of the cochlear function and if sensorineural hearing loss were to be observed, its development could be altered, without the need to wait until it was affected by medium frequencies at 500–3000Hz with its concomitant effects on communication and language discrimination.
Although the purpose of our study was not to determine the casuality between rheumatoid arthritis and the high incidence of hearing loss at high hearing thresholds, this preliminary approach has enabled us to determine lines of inquiry. This is relevant because although the condition at these high frequencies has no impact on the quality of life of the patient, if untreated, it could be the beginning over time of an irreversible hearing loss damaging communication thresholds.
It is probable that findings from this study may assist the physician in using high frequency audiometry to intentionally look out for this hearing impairment in patients with rheumatoid arthritis, and alter its development through treatment, thereby preventing any further impairment.
Conflict of interestsThe authors have no conflict of interests to declare.
We wish to thank Dr. M.S.P. César Luna Gurrola for his participation in the preparation, review and statistical interpretation of this article.
Please cite this article as: Treviño-González JL, Villegas-González MJ, Muñoz-Maldonado GE, Montero-Cantu CA, Nava-Zavala AH, Garza-Elizondo MA. Hipoacusia neurosensorial subclínica en pacientes femeninas con artritis reumatoide. Cir Cir. 2015;83:364–370.