Liver haemangiomas are the most common benign tumours, commonly presented in women and considered giant when their diameter surpasses 4cm. They are mostly asymptomatic and incidentally found. They manifest with abdominal pain and mass effect. These tumours can be managed by observation, enucleation, resection, and embolisation.
ObjectiveTo determine the experience in our unit as regards the treatment and post-surgical outcomes of patients with liver haemangiomas.
Materials and methodsA retrospective study was performed on 14 patients with a histopathological diagnosis of liver haemangioma. An analysis was made using the sociodemographic, tumour-related and surgical related variables, as well as any complications.
ResultsOf the 14 patients analyse, there were 7 males and 7 females, with a median age of 43.43±15.03 years, and a mean tumour size of 6.86±3.5cm. Eight (51.7%) of the tumours were located in the right lobe, 3 (21.4%) in the left lobe, and 3 (21.4%) in the caudate lobe. Resection was performed in 7 patients (50%), enucleation in 5 patients (35.7%), and biopsy in 2 patients (14.3). No relationship was found between sex, pathology, or tumour location. No morbidity or mortality was found.
ConclusionsLiver haemangiomas in our unit have similar characteristics to those described in other studies. Surgical treatment in our hospital offers a positive outcome.
Los hemangiomas hepáticos son los tumores hepáticos benignos más comunes, predominan en las mujeres y se consideran gigantes los mayores de 4cm. Son asintomáticos y generalmente su hallazgo es incidental. Sus síntomas pueden ser: dolor abdominal y efecto de masa. Los hemangiomas se pueden observar, enuclear, resecar o embolizar.
ObjetivoDeterminar la experiencia de nuestra unidad, en cuanto al tratamiento otorgado y su evolución posquirúrgica, de los pacientes con hemangiomas hepáticos.
Material y métodosEstudio retrospectivo, en 14 pacientes con diagnóstico histopatológico de hemangioma hepático. Se analizaron variables sociodemográficas y relacionadas con el tumour y el acto quirúrgico, así como las complicaciones.
ResultadosSe analizaron 14 pacientes, 7 hombres y 7 mujeres con una edad media de 43.43±15.03 años; el tamaño promedio de los hemangiomas fue de 6.86±3.5cm. Ocho (57.1%) se encontraron en el lóbulo derecho, 3 (21.4%) se encontraron en el lóbulo izquierdo y 3 (21.4%) se encontraron en el lóbulo caudado. Se realizó resección en 7 pacientes (50%), enucleación en 5 pacientes (35.7%) y biopsia en 2 pacientes (14.3%). No se encontró relación entre la patología, el sexo y la localización del tumour. No hubo morbimortalidad.
ConclusionesLos hemangiomas hepáticos en nuestro hospital guardan características similares a las descritas en otros estudios y el tratamiento quirúrgico en nuestro hospital ofrece buenos resultados.
Liver haemangiomas are the most common benign tumours, with a prevalence of 0.4–7% in autopsies. They are found in 1–20% of the population in general and their incidence of discovery through abdominal ultrasound performed for other indications is 1.7%. The tumours may be single in 30–35% or multiple in 10–40%.1–6 The majority of haemangiomas are small (under 1cm in diameter) and are considered giant when their diameter surpasses 4cm, which represents 10% of them. The average presentation age ranges from 40 to 60 and they are more commonly presented in women (woman:man 5:1).1,3,4,7,8
The majority of liver haemangiomas are asymptomatic, especially when they are below 4cm, and may be safely treated by observation.2,4 The predominant symptom is abdominal pain, mainly in the upper right quadrant. They may also present as a form of biliary colic pain, with obstructive jaundice and gastric obstruction. Physical examination in the majority of cases reports normal, except in some cases where the size of the haemangioma means that it becomes a palpable mass. Other less common symptoms are chylous ascites, fever. Kasabach Merritt syndrome may also present.3,4,8,9
At present, surgery is the most effective therapy for definitive treatment of liver haemangiomas. However, optimal management for patients with giant haemangiomas remains controversial.3 Choosing enucleation over formal resection depends on several factors: the most important is diagnostic certainty and anatomical considerations such as the location and extension of the lesion. Resection may be preferred for the potentially malignant tumours and for tumours which replace a liver segment.3
Successful treatment of giant liver haemangiomas, as previously mentioned, depends on diagnostic confirmation and when the tumour does require surgery to determine which type of surgery is required. Other indications for surgery include: uncertain diagnosis, growth of the haemangioma, professions where the person may suffer trauma of the abdomen, dyspepsia, persistent thrombocytopenia and rupture with intraperitoneal haemorrhage.9,10
The aim of this study was to determine the most frequent type of surgery administered to patients with liver haemangiomas and assess their post surgical evolution in our unit.
Material and methodsA retrospective, transversal, analytical study was conducted which included 14 patients, with histopathologic diagnosis of liver haemangioma, who had had surgery with resection, enucleation or had undergone biopsy between April 1, 2008 and 30 April, 2015 in the Unidad Médica de Alta Especialidad, Hospital de Especialidades No. 14, Centro Médico Nacional Adolfo Ruiz Cortínez, Instituto Mexicano del Seguro Social (Veracruz, Mexico). Prior to seeking authorisation from the local Ethics and Research Committee of our unit, clinical files were reviewed and the following variables extracted: age, gender, body mass index (BMI), size and location of haemangioma, date of surgery, referral for surgery, type of surgery, Pringle manoeuvre, blood loss, number of blood packs transfused, days in hospital, operating time and complications. All the patients were studied with standard ultrasound and contrast computed tomography. Patients with a final diagnosis which was different to liver haemangioma were excluded and those patients who had an incomplete or illegible clinical record were also excluded.
Associations or significant differences regarding the tumour and its management were sought, depending on the gender, in addition to location and size.
Statistical analysisStatistical analysis of continuous and discreet variables was measured in averages, standard deviation and range. Categorical variables were measured in frequencies and percentages. To compare continuous and discreet variables the Student's t-test or Wilcoxon analysis was used.
The Chi square test and ANOVA were used to compare categorical variables. p<0.05 was considered to be statistically significant. SPSS version 21 software was used for analysis.
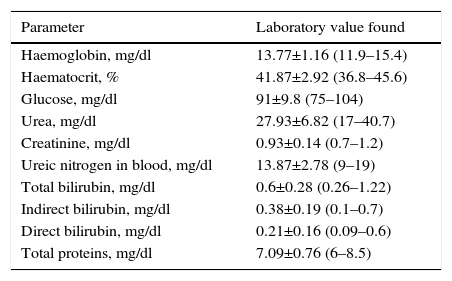
ResultsOf the 14 patients, 7 were men (50%) and 7 were women (50%). The mean presentation age was 43.43±15.03 years (15–64), mean weight was 70.94±13.37kg (52–98), average BMI was 26.64±4.61kg/m2 (21.8–39), average size of haemangiomas was 6.86±3.5cm (2–15), 2 of them (14.28%) were under 4cm. Eight (57.1%) were found in the right lobe, 3 (21.4%) were found in the left lobe and 3 (21.4%) were found in the caudate lobe. Preoperative laboratory values are shown in Table 1.
Pre-surgical laboratory results of patients treated with surgery for liver haemangioma.
| Parameter | Laboratory value found |
|---|---|
| Haemoglobin, mg/dl | 13.77±1.16 (11.9–15.4) |
| Haematocrit, % | 41.87±2.92 (36.8–45.6) |
| Glucose, mg/dl | 91±9.8 (75–104) |
| Urea, mg/dl | 27.93±6.82 (17–40.7) |
| Creatinine, mg/dl | 0.93±0.14 (0.7–1.2) |
| Ureic nitrogen in blood, mg/dl | 13.87±2.78 (9–19) |
| Total bilirubin, mg/dl | 0.6±0.28 (0.26–1.22) |
| Indirect bilirubin, mg/dl | 0.38±0.19 (0.1–0.7) |
| Direct bilirubin, mg/dl | 0.21±0.16 (0.09–0.6) |
| Total proteins, mg/dl | 7.09±0.76 (6–8.5) |
The most frequently used type of surgery was resection, for a total of 7 patients (50%), followed by enucleation for 5 patients (35.7%) and lastly biopsy in 2 patients (14.3%). Biopsies were only carried out on the caudate lobe. The primary indication for surgery was pain (57.1%), followed by doubtful diagnosis (28.6%) and dysphagia (14.3%). The average time in surgery was 174.38±41.09min (105–240), with a mean hospital stay of 5.36±2.6 days (2–10), average blood loss of 517.86±533.35ml (100–2150) with a mean transfusion of 0.57±1.01 blood packs (0–3). The Pringle manoeuvre was performed in 5 cases (35.7%). There were no complications related to surgery in any of the patients included in the study, nor were there any perioperative deaths.
Patients with haemangioma located in the right hepatic lobe had significantly lower levels of blood urea nitrogen (12.32±2.09mg/dl) than those where it was located in the left lobe (17.20±1.55mg/dl) (p=0.01). Patients with haemangiomas located in the right lobe presented with significantly lower levels of total bilirubin (0.50±0.18mg/dl) compared with those where it was located in the left lobe (0.95±0.25mg/dl) (p=0.03). Patients with haemangioma located in the caudate lobe presented with significantly lower levels of indirect bilirubin (0.23±0.5mg/dl) than those where it was found in the left lobe (0.64±0.04mg/dl) (p=0.009). No significant difference was found regarding gender or tumour location, size, type of surgery, time in surgery, perioperative bleeding, hospital stay duration, number of blood packs transfused or use of the Pringle manoeuvre.
DiscussionThe findings from our study indicate that the presentation of liver haemangiomas in our hospital is similar to that described with regards to socio-demographic factors and tumour characteristics. Our findings indicate that surgical treatment has a satisfactory outcome in any of its modalities.
Similar results to that published with regard to presentation age were found. However, in our study no preference towards any gender was discovered, which differs from that reported by Lerner et al.2 with an 88% predomination of women, and by the Asian series,5 where the frequency of presentation in women is 73.8%. Location of the tumour was primarily in the right hepatic lobe, similar to that published in the Western and Mexican series2,9 and different from the Oriental series5 who reported a greater frequency in the left hepatic lobe. Regarding haemangioma size, in our study the mean was lower than in other series.2,5–7,10,11
The most frequently reported referral for surgery in our series was for abdominal pain, similarly to that reported in other series.1,6,11–13 The patients who underwent surgery on suspected diagnosis were referred from other hospitals and their imaging studies with inconclusive radiologic diagnoses, were produced outside our unit. We therefore chose to offer surgical treatment to the patient. The type of surgical intervention most frequently performed was resection, similar to that published by Singh et al.10 However, they favoured enucleation as the procedure of choice. Ozden et al.11 reported greater frequency of enucleation and they are in favour of performing it, since they consider it a fast and safe procedure. In our findings we found no significant differences with regards to the type of surgery performed, similar to that reported by the Italian series.13
In our series there was less blood loss and surgery time was lower compared with others,5,6,9 because the size of the haemangiomas was smaller, and the number of reported cases were fewer than in other studies, taking into account that they include 2 biopsies. Hospital stay in our series was similar to that published by Singh et al.10 who in his group of enucleations presented a mean of 5.6 days and lower than the figure of their group of resections with a mean of 10 days. Hospital stay duration in our study was lower since transoperative haemorrhage was comparatively lower, as was the number of cases. There were no complications or mortality in our series, unlike those of other authors, who reported morbidities from 13.1% to 41.6%.1,2,5,9,10
Few Mexican studies describe the natural history and treatment of liver haemangiomas in Mexico, and most are report cases.
In 2003 Martínez González6 resected/enucleated 24 haemangiomas (22 cavernous haemangiomas and 2 haemangiomatoses) in 2 hospitals, mainly in women, with a 91.6% resolution of symptoms. Another Mexican series of patients with liver haemangioma corresponded to that published by Moctezuma Velázquez in 2014,9 in which during a period of 18 years, 57 patients with liver haemangiomas were studied in a follow-up period of 66 months. 56.14% of them corresponded to giant liver haemangiomas. Ten patients were asymptomatic and only 9 patients underwent surgery and 2 were treated with biopsy, without there being any incidence of perioperative morality.
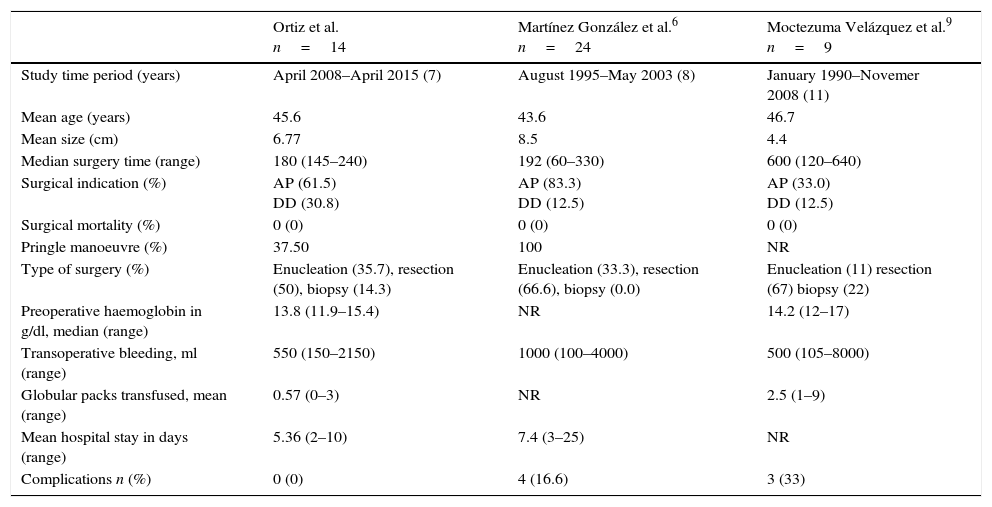
Table 2 compares our results with those of the series published in Mexico. Unlike the results published by other authors,6,9 we only include patients who underwent surgery, since we only receive inter-consultancy patients when there is a referral for surgery. It is of note that the mean hospital stay in our patients is lower, with no complications, although tumour size is also smaller.
Comparison of the characteristics of patients and of the surgical treatment with other series published in Mexico.
| Ortiz et al. n=14 | Martínez González et al.6 n=24 | Moctezuma Velázquez et al.9 n=9 | |
|---|---|---|---|
| Study time period (years) | April 2008–April 2015 (7) | August 1995–May 2003 (8) | January 1990–Novemer 2008 (11) |
| Mean age (years) | 45.6 | 43.6 | 46.7 |
| Mean size (cm) | 6.77 | 8.5 | 4.4 |
| Median surgery time (range) | 180 (145–240) | 192 (60–330) | 600 (120–640) |
| Surgical indication (%) | AP (61.5) DD (30.8) | AP (83.3) DD (12.5) | AP (33.0) DD (12.5) |
| Surgical mortality (%) | 0 (0) | 0 (0) | 0 (0) |
| Pringle manoeuvre (%) | 37.50 | 100 | NR |
| Type of surgery (%) | Enucleation (35.7), resection (50), biopsy (14.3) | Enucleation (33.3), resection (66.6), biopsy (0.0) | Enucleation (11) resection (67) biopsy (22) |
| Preoperative haemoglobin in g/dl, median (range) | 13.8 (11.9–15.4) | NR | 14.2 (12–17) |
| Transoperative bleeding, ml (range) | 550 (150–2150) | 1000 (100–4000) | 500 (105–8000) |
| Globular packs transfused, mean (range) | 0.57 (0–3) | NR | 2.5 (1–9) |
| Mean hospital stay in days (range) | 5.36 (2–10) | 7.4 (3–25) | NR |
| Complications n (%) | 0 (0) | 4 (16.6) | 3 (33) |
AP: abdominal pain; DD: doubtful diagnosis; NR: not reported.
Our study has several limitations. It is a retrospective study, with a limited sample size and we include 2 patients in this study upon whom biopsy was performed. However, our surgical outcomes reflecting surgery time and no morbidity or mortality are an improvement upon those previously published in Mexican literature.
ConclusionsLiver haemangiomas in our hospital have similar characteristics to those described in other studies and the surgical treatment in our hospital offers good outcomes. The patients with liver haemangioma surpassing 4cm with symptoms are referred for surgery (resection or enucleation).
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Ortiz-Bayliss AB, Martínez-Mier G, Alvarado-Arenas RA, Lajud-Barquín FA. Tratamiento quirúrgico de los hemangiomas hepáticos en una unidad médica de alta especialidad del sureste de México. Cirugía y Cirujanos. 2016;84:477–481.