Prolonged air leak after pleural decortication is one of the most frequent complications.
ObjectiveThe aim of this study is to compare the effects of prolonged air leak between the digital chest drainage (DCD) system and the classic drainage system in patients with empyema class IIB or III (American Thoracic Society classification) in pleural decortication patients.
Material and methodsA total of 37 patients were enrolled in a prospective randomised control trial over one year, consisting of 2 blinded groups, comparing prolonged air leak as a main outcome, the number of days until removal of chest drain, length of hospital stay and complications as secondary outcomes.
ResultsThe percentage of prolonged air leak was 11% in the DCD group and 5% in the classic group (p=0.581); the mean number of days of air leak was 2.5±1.8 and 2.4±2.2, respectively (p=0.966). The mean number of days until chest tube removal was 4.5±1.8 and 5.1±2.5 (p=0.41), the length of hospital stay was 7.8±3.7 and 8.9±4.0 (p=0.441) and the complication percentages were 4 (22%) and 7 (36%), respectively (p=0.227).
DiscussionIn this study, no significant difference was observed when the DCD was compared with the classic system. This was the first randomised clinical trial for this indication; thus, future complementing studies are warranted.
La fuga aérea prolongada después de una pleuro-decorticación en una de las complicaciones más frecuentes.
ObjetivoEl objetivo de este estudio es comparar la fuga aérea entre el sistema de drenaje torácico digital (DCD) y el sistema de drenaje clásico, en pacientes con empiema de clase IIB o III (clasificación de la Sociedad Americana de Tórax) intervenidos mediante pleuro-decorticación.
Material y métodosDe manera prospectiva, comparativa y aleatorizada, 37 pacientes fueron estudiados en un periodo de un año. Divididos en 2 grupos, se comparó la fuga aérea postoperatoria, analizándose el número de días de internamiento, el día de retiro de los drenajes, así como las complicaciones en ambos grupos.
ResultadosEl porcentaje de fuga aérea prolongada fue del 11% en el grupo DCD y del 5% en el grupo de drenaje clásico (p=0,581); el número de días con fuga aérea fue de 2,5±1,8 y 2,4±2,2, respectivamente (p=0,966). El número de días para retiro de drenaje fue 4,5±1,8 y 5,1±2,5 (p=0,41), la estancia intrahospitalaria fue de 7,8±3,7 y 8,9±4 días (p=0,441) y el porcentaje de complicaciones fue 22 y 36%, respectivamente (p=0,227).
DiscusiónEn este estudio se observa una tendencia positiva pero no significativa a favor del uso de los DCD cuando se comparan con el drenaje clásico. Estudios más largos y multicéntricos son requeridos.
Empyema is one of the most common surgical chest conditions in Mexico. A great many of these patients (45%) require surgical treatment, which represents around 90 cases of pleural decortication.1
Air leak after complete decortication is to be expected, and even more so in advanced empyema.2 However, digital chest drainage (DCD) digital has shown good results in the management of prolonged air leak in various surgical procedures.3 A reduction in days of drainage and hospital stay has been demonstrated with these drains.3–7 Probably one of their greatest advantages is the elimination of interobserver variability on assessing air leak for removal of the drains.7,8 The DCD system has even been used in ambulant patients with prolonged air leak.7,9
DCD use in pleural decortication has not been described in the literature. Therefore, the aim of our study was to evaluate its potential benefits, which will be valuable information for surgeons, since this technology is increasingly available in chest surgery departments.
Material and methodsA prospective, comparative and randomised study of 37 patients treated with pleural decortication due to empyema classified as IIB or III by the American Thoracic Society, in the period from March 2013 to February 2014. The sample size was calculated according to the published data.7 The statistical power was set at 5% and the beta error at 80%, with a minimum of 16 patients per group. The DCD group had 18 patients, and there were 17 in the traditional group.
The patients included in the study had IIB or III empyema, which had not been resolved by the placement of a drain. Patients with other grades of empyema, those who underwent thoracoscopic surgery, and those with a physical status classification greater than ASA III prior to anaesthesia were excluded.
The Thopaz-Medela™ (Switzerland) system was used for the DCD group; traditional Atrium Ocean™ drains were used (U.S.A.) for the control group.
All the patients signed their informed consent which included them in this study protocol, in compliance with the guidelines of the institution's ethics committee.
The surgical technique was standard for all the patients: a posterolateral thoracotomy was performed and then pleural decortication, as described by Delorme and Deslauries.10 Two rigid 32 F Argyle™ drains were placed, one anterior and the other posterior, attached to a Y connector, configured at a postoperative suction of −15cm H2O, immediately after closure of the thoracic wall. The criteria for removal of the drains were: air leak less than 40ml/min in the past 12h for the DCD patients, and lack of air leak for the traditional drains according to the Modified Robert David Cerfolio (MRDC) classification, both with complete lung reexpansion confirmed by chest X-ray. With regard to the amount of fluid collected, the drain was removed when the loss was less than 2ml/kg in 24h (Table 1).
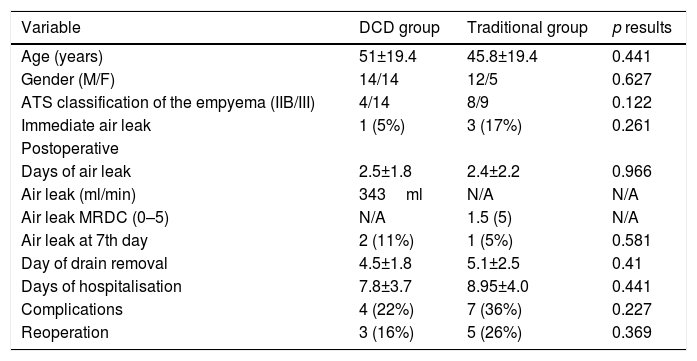
Variables of the study groups.
| Variable | DCD group | Traditional group | p results |
|---|---|---|---|
| Age (years) | 51±19.4 | 45.8±19.4 | 0.441 |
| Gender (M/F) | 14/14 | 12/5 | 0.627 |
| ATS classification of the empyema (IIB/III) | 4/14 | 8/9 | 0.122 |
| Immediate air leak | 1 (5%) | 3 (17%) | 0.261 |
| Postoperative | |||
| Days of air leak | 2.5±1.8 | 2.4±2.2 | 0.966 |
| Air leak (ml/min) | 343ml | N/A | N/A |
| Air leak MRDC (0–5) | N/A | 1.5 (5) | N/A |
| Air leak at 7th day | 2 (11%) | 1 (5%) | 0.581 |
| Day of drain removal | 4.5±1.8 | 5.1±2.5 | 0.41 |
| Days of hospitalisation | 7.8±3.7 | 8.95±4.0 | 0.441 |
| Complications | 4 (22%) | 7 (36%) | 0.227 |
| Reoperation | 3 (16%) | 5 (26%) | 0.369 |
MRDC: Modified Robert David Cerfolio Classification; DCD: digital chest drainage.
Air leak persisting longer than 7 days was considered prolonged.4 The days until removal of the drain, the days of hospital stay, and the number and type of complications appearing in each group were quantified.
XLSTAT for Mac was used for the statistical analysis and the Student's t-test for the continuous variables. Statistical significance was set at p=0.05.
ResultsThe demographic characteristics are similar. Ninety-two patients were recruited during the time period, of whom 57 were excluded due to an exclusion criterion. None of the patients under study were excluded, and none of the patients needed to be discharged home with a drain or Heimlich valve.
The amount of air leak was not comparable because the leak measurement scale was different on each device: in ml/min of air for DCD, and on a scale of 0–5 for the Atrium-Ocean™ drains.
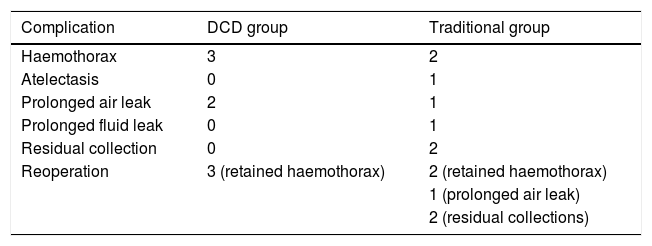
The overall leak percentage was 8%: 11% in the DCD group and 5% in the traditional drainage group (p=0.581). The mean air leak days were 2.5±1.8 and 2.4±2.2, respectively (p=0.966). The drains were removed on days 4.5±1.8 and 5.1±2.5 (p=0.41), the days of hospital stay were 7.8±2.7 and 8.9±4.0 (p=0.441). Finally, the complication rate was 22% (4 patients) vs 36% (7 patients), respectively (p=0.227). Three patients (16%) of the DCD group had to be reoperated due to coagulated haemothorax vs 5 patients (26%) from the control group (p=0.369) (Table 2).
Surgical complications.
| Complication | DCD group | Traditional group |
|---|---|---|
| Haemothorax | 3 | 2 |
| Atelectasis | 0 | 1 |
| Prolonged air leak | 2 | 1 |
| Prolonged fluid leak | 0 | 1 |
| Residual collection | 0 | 2 |
| Reoperation | 3 (retained haemothorax) | 2 (retained haemothorax) |
| 1 (prolonged air leak) | ||
| 2 (residual collections) |
The Chi2 test was used and no significance was found between the groups.
DCD: digital chest drainage.
It was not possible in this study to identify any statistically significant result on comparing the Thopaz-Medela™ with the Atrium-Ocean™, however positive tendencies were observed in terms of reduced days of drainage, days of hospital stay and the number of patients who required reoperation due to retained haemothorax. To our knowledge, this is the first study to assess the results of DCD in patients post pleural decortication. Therefore we have no literature with which to contrast our results. There are already studies that show reduced days of chest drainage in other types of diseases using DCD.5,6 However, there are also papers that refer to the heterogeneity of the groups studied, which means that sometimes it is questionable whether a reduction in days of drainage really has been achieved.11
Our study only included empyema at stages IIB and III. These are patients that present the most serious technical problems, due to pleural thickening. Therefore, postoperative blood loss and air leak are common complications that can even require reoperation. In our study we observed a reduction in reoperation in the DCD group: this could be attributed to the capacity of the device itself to maintain continuous suction in the pleural space, which stops clots forming in the chest and, therefore, the drains do not become obstructed. When traditional drains are placed, suction is often interrupted, for example when the patient is being moved, on ambulation, etc. It is also important to stress that drains can occasionally be kinked and obstructed by the patient's own movements, which interrupts suction. This event is alerted immediately by the alarm mechanism of the DCD, which means the problem can be rapidly solved and suction is not interrupted. In terms of continuous suction, with DCD we can guarantee and monitor that the suction programmed in the device is real. Occasionally, when depending on wall suction, the variability can be unquantifiable.
We found no significant differences in the time of removal of the drain, in contrast to other studies, with a notable reduction in days of drainage. We can explain this because with empyema air leak is often not the only criterion for drain removal; the amount of fluid drained and its characteristics are also very important.
We consider that a weakness of our study is the small sample size. However, the sample size calculations indicate that 16 patients in each group could be sufficient. This information, added to the lack of studies in the literature with the same diagnostic and treatment characteristics that we propose in our study, lead us to believe that our results could be valid. However, more numerous series or multicentre studies might draw more solid conclusions.
To conclude our study, we can state that there is a positive tendency for DCD, but there are no significant differences in terms of days of chest drainage, days of hospital stay or complications and the need for reoperation between the DCD and the traditional systems.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work centre on the publication of patient data.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Conflict of interestThe authors have no conflict of interests to declare.
Please cite this article as: Mier JM, Cortés-Julián G, Berrios-Mejía J, Víctor-Valdivia Z. Beneficios del drenaje torácico digital en pleurodecorticación por empiema. Estudio prospectivo, comparativo aleatorizado. Cir Cir. 2017;85:522–525.