Deaths due to tuberculosis have reached 2.5 million cases per year worldwide. Poncet's disease is an infrequent form of tuberculosis characterised by a clinical picture of polyarthritis.
Clinical caseA 24-year-old male presented with morning stiffness, arthralgias, bilateral symmetric arthritis of the proximal interphalangeal joints, wrists, knees, ankles, and shoulders, and adenomegalies at the cervical, submandibular, left supraclavicular, axillary and inguinal levels, without fever. Laboratory results were as follows: ESR 44mm/h, C-reactive protein 4.35, normal levels of complement C3 and C4, negative rheumatoid factor and anticyclic citrullinated peptide antibodies, positive antinuclear antibodies with fine speckled pattern (1:320) and cytoplasm (1:160) pattern and negative anti-Smith, -double-stranded DNA, Sjogren's syndrome-antigen A and Sjogren's syndrome-antigen B. Histological report of cervical node tissue revealed granulomatous lesions compatible with tuberculosis. Rheumatoid arthritis and systemic lupus erythematosus were ruled out. Anti-tuberculosis agents were initiated that resolved the clinical picture. Diagnosis of Poncet's disease was confirmed.
ConclusionThe differential diagnosis between tuberculosis and autoimmune inflammatory joint diseases is a clinical challenge.
Las muertes por tuberculosis a nivel mundial han superado los 2,5 millones de casos por año. La enfermedad de Poncet es una forma poco frecuente de tuberculosis, caracterizada por un cuadro de poliartritis.
Caso clínicoVarón de 24 años de edad, quien presentó rigidez matinal, artralgias, artritis bilateral simétrica de interfalángicas proximales, carpos, rodillas, tobillos, hombros y adenomegalias a nivel cervical, submandibular, supraclavicular izquierda, axilar e inguinal, sin fiebre. Resultados de laboratorio: velocidad de sedimentación globular 44mm/hora, proteína C reactiva 4.35, niveles de complemento C3 y C4 normales, factor reumatoide y anticuerpos anti-péptido C citrulinado negativos, anticuerpos antinucleares positivos con patrón moteado fino 1:320 y citoplásmico 1:160; anticuerpos anti-Smith, anti-ADN de doble cadena, antígeno A de síndrome de Sjogren's y antígeno B de síndrome de Sjogren's negativos. Reporte histológico del tejido ganglionar cervical con lesiones granulomatosas compatibles con tuberculosis. Se descartaron artritis reumatoide y lupus eritematoso sistémico. Se inició tratamiento antifímico remitiendo el cuadro clínico. Se concluyó el diagnóstico de enfermedad de Poncet.
ConclusiónEl diagnóstico diferencial entre tuberculosis y enfermedades articulares inflamatorias de etiología autoimune es un reto clínico.
Human tuberculosis is the major cause of morbimortality in many countries1,2; deaths due to tuberculosis worldwide have exceeded an annual 2.5 million cases.1
Poncet's disease is a rare form of tuberculosis, characterised by a clinical picture of polyarthritis associated with pulmonary or extrapulmonary tuberculosis, with no evidence of infection by mycobacteria inside the affected joints.3,4 According to Lesprit et al.5 it was described by Poncet at the end of the 19th century; one of the most important differential diagnoses for this disease is rheumatoid arthritis, as the clinical picture is similar and the rheumatoid factor is present in both cases.6
From a clinical perspective arthritis is the most common symptom of Poncet's disease,7 which can have a bilateral and symmetrical pattern, other manifestations can present on the skin and the mucosa in the form of erythema nodosum,8,9 erythematous rash,10 papulonecrotic lesions,11 mouth ulcers and conjunctivitis.6
Clinical caseA 24-year-old male patient, with a smoking index of 7, alcohol consumption from the age of 15, becoming intoxicated every 8 days; he reported regular cannabis consumption for one year, and using cocaine for one month a year previously, heterosexual with just one partner. He started to become unwell in February of 2013 and was attended in May of the same year with morning stiffness, pain in the shoulder, elbow, carpal, proximal interphalangeal, coxofemoral, knee, ankle and metatarsophalangeal joints; with a weight loss of 10kg over the past 3 months, hair loss and epistaxis; he reported no fever. On physical examination enlarged lymph nodes were palpated at cervical, submandibular, left supraclavicular, axillary and inguinal levels. Arthritis in the carpal, proximal interphalangeal and knee joints was confirmed clinically; with a bilateral pattern. The laboratory reported globular sedimentation rate 37mm/h and C-reactive protein 1.5; based on the inflammatory context the patient was started on prednisone 20mg daily.
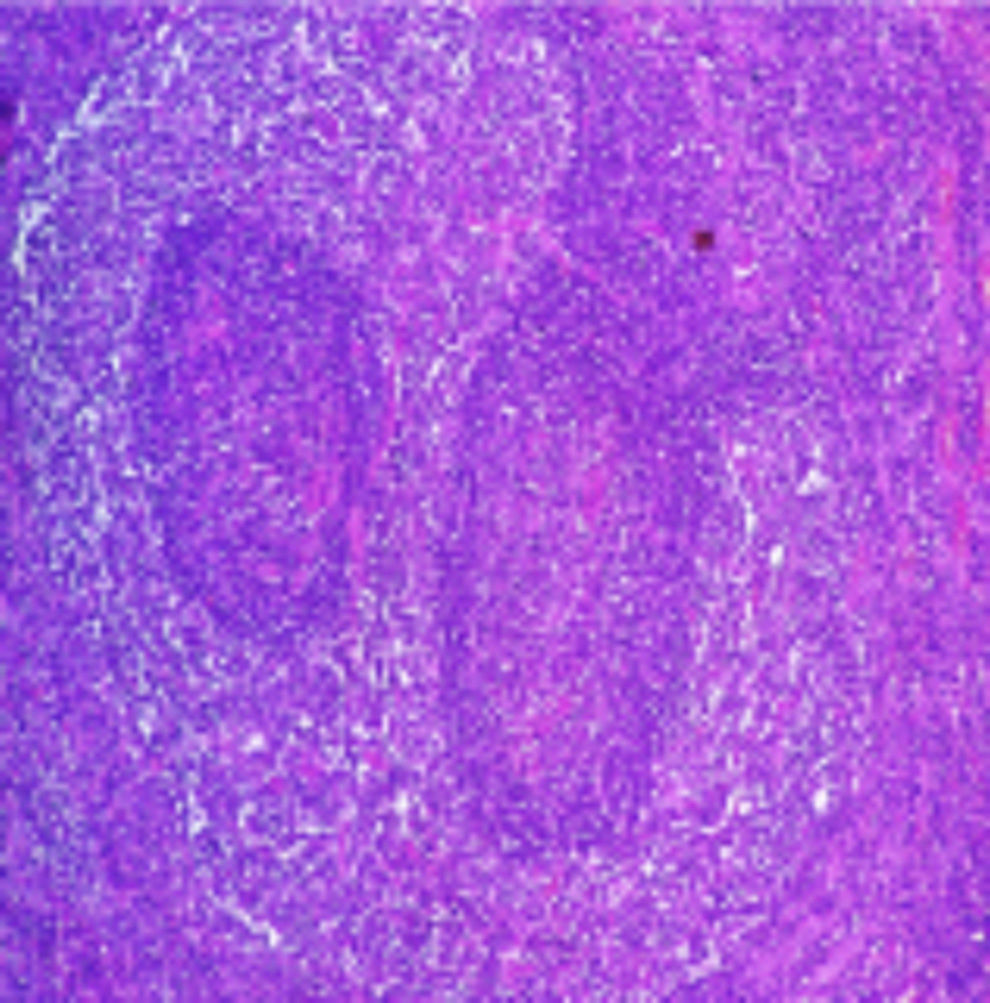
In June, he continued to suffer asthenia, adynamia, arthralgia in the ankle metacarpophalangeal joints and arthritis in the carpal joints, second and third right proximal interphalangeal joints. The complementary laboratory report showed rheumatoid factor and negative anti-CCP antibody, globular sedimentation rate 44mm/h, reactive protein 4.35, normal C3 and C4 complement levels, positive antinuclear antibodies with a fine speckled pattern 1:320 and cytoplasmic antinuclear antibodies 1:160, the specific anti-Smith antibodies, double chain anti-DNA antibodies, Sjogren's syndrome antigen A and Sjogren's syndrome antigen B were negative; the diagnosis up until that time had been seronegative rheumatoid arthritis, and therefore methotrexate at a weekly dose of 7.5mg was added to his treatment. At this visit antinucleosome antibodies, TORH profile, viral panel, PPD, to evaluate the possibility of biological therapy, were requested, and a biopsy was taken of the cervical lymph node. During July the patient maintained treatment with steroids and methotrexate, adding plaquenil 200mg every 24h; in September the patient reported no enlarged lymph nodes, persistent joint pain in his elbows, knees and ankles, arthritis in his carpal and interphalangeal joints of less intensity. The laboratory reported a persistent increase in globular sedimentation rate at 37mm/h. The histological report from the cervical lymph node biopsy reported the presence of granulomatous lesions compatible with tuberculosis, special tests Ziehl Neelsen, PAS, GROCOTT stains were negative (Fig. 1), thus ruling out any other granulomatous conditions, with these results antiphthisic treatment was started, with a favourable clinical response to treatment and remission of the clinical manifestations. One year after the patient had completed the anti-tuberculous therapy he was asymptomatic. The histological findings along with the therapeutic response enabled a definitive diagnosis of Poncet's disease to be made and the steroids and disease-modifying medication for rheumatoid arthritis were discontinued.
DiscussionTuberculous rheumatism or “Poncet's disease” is a form of the expression of tuberculous infection. Tuberculosis presents in various forms and depend on the inherent condition of the host (age, immunosuppressed state, malnutrition, genetics, co-existing diseases, vaccination against tuberculosis) or associated with Mycobacterium tuberculosis (virulence of the bacteria, tissue or organ).12 Clinical suspicion of tuberculosis in general requires the presence of M. tuberculosis to be confirmed with BAAR tests, or Löwenstein-Jensen medium. Current procedures based on molecular biology have demonstrated their efficacy in identifying M. tuberculosis.13,14 The pathogenesis of tuberculous rheumatism is not known, it is postulated that it might be mediated by immune mechanisms triggered after infection by M. tuberculosis associated with the host's genetic susceptibility. Amongst the immune pathways which have been postulated to explain the association between rheumatic diseases, the genetic markers of the major histocompatibility complex and infectious diseases include: (1) the deposition of immune complexes (antigen-antibody) which promote an inflammatory response; (2) the production of toxins by mycobacteria, which function as superantigens; (3) the deposition of the antigen and retention of flogistic bacterial components inside the joint; and (4) molecular mimicry of M. tuberculosis and the proteoglycans of the articular cartilage matrix.15,16
In accordance with the review by Rueda et al.17 no more than 200 cases of Poncet's disease have been reported in the literature; the countries with the most published cases are India with 70, Brazil with 26 and Mexico with 20. The joints that are most frequently affected are: ankles 63.3%, knees 58.8%, carpal 29.1% and elbows (23.1%); all of these were affected in our case,3,8 joints such as the proximal interphalangeals are less frequently affected, the metacarpophalangeal joints are also compromised and the morning stiffness is associated in some cases.15
The focus of tuberculous infection in the cases reported in the literature is 56.8% extrapulmonary and 42% compromise the lymphatic system. In our case, lymph node biopsy demonstrated the presence of a tuberculous granuloma, the specific stains did not prove positive to identify the tubercle bacillus. Cases similar to ours have been reported in literature, where a diagnosis is made by exclusion, and is supported by the response to anti-tuberculous therapy, which delays the diagnosis of tuberculous rheumatism “Poncet's disease” from 19 months to 12 years according to Rueda et al.17 and Walter.18 An important element in consolidating a diagnosis, is that by eliminating the focus of infection the pain and joint inflammation subside without leaving damage to the joints; this is borne out by this case. This element is part of the diagnostic criteria proposed by Rueda et al.17 for Poncet's disease, which include: (1) evidence of active extra-articular tuberculosis; (2) involvement of more than one joint, including knees and ankles; (3) no axial or vertebral compromise, or sacro-iliac involvement; (4) non-specific laboratory results; (5) complete remission after anti-tuberculous therapy; (6) no chronic joint compromise; and (7) the exclusion of other rheumatological diseases.17
Poncet's disease is a rare form of tuberculosis, and therefore clinicians must carefully monitor patients with inflammatory joint diseases of autoimmune origin.
ConclusionsTuberculosis is a worldwide public health problem, and has been nicknamed “the great mimicker” due to its clinical and serological expression. As in the case presented with Poncet's disease, this is an under-recognised form of expression of tuberculosis as reflected in the few published cases. In light of this, we consider it important to disseminate knowledge on this clinical case and contribute data which could result in a consensus of clinical criteria, in order to enable early diagnosis of the disease and its treatment. The diagnosis and treatment of these types of patients is important towards helping to control a health problem which is endemic in several regions of the world.
Conflict of interestsThe authors have no conflict of interest to declare.
Please cite this article as: Lugo-Zamudio GE, Barbosa-Cobos RE, González-Ramírez LV, Delgado-Ochoa D. Reumatismo tuberculoso «enfermedad de Poncet». Reporte de caso. Cir Cir. 2016;84:167–170.