Four-dimensional computerized tomography (4D-CT) offers a good sensitivity for the localization of the pathological gland responsible of primary hyperparathyroidism. The aim was to evaluate its results as a second line preoperative localization test after inconclusive or discordant results of usual preoperative studies.
Material and methodsObservational retrospective study that included all patients intervened for primary hyperparathyroidism with 4D-CT scan as preoperative study, from 1st October 2016 to 1st October 2021, in a tertiary referral centre.
The results of 4D-CT, cervical ultrasound, and Nuclear Medicine explorations (scintigraphy, SPECT and SPECT-CT) were compared with the gold standard of the surgical exploration and the pathological result. The correct lateralization and the approximate localization rates of the pathological gland were evaluated.
ResultsA total of 64 patients were analysed, with a 93,8% (60/64) remission rate. 4DCT showed a correct lateralization in 57,8% (37/64) of the cases and revealed the approximate localization of the gland in 48,4% (31/64) of the cases. The cervical ultrasound had a rate of 31,1% (19/61) and 18% (11/61) for the correct lateralization and approximate localization, respectively, compared to 34,9% (22/63) and 28,6% (18/63) in Nuclear Medicine explorations, and 32,7% (16/49) and 24,5% (12/49) in SPECT-CT. These differences were statistically significant.
Conclusion4D-CT demonstrated acceptable results for the localization of the lesions responsible of primary hyperparathyroidism, thus its use should be considered with the absence of localization in routinely studies.
La tomografía computarizada en cuatro dimensiones (TC-4D) ofrece buena sensibilidad para localizar la glándula patológica responsable del hiperparatiroidismo primario. El objetivo fue evaluar su rendimiento como estudio de segunda línea tras ausencia de localización o resultado no concordante de los estudios habituales.
Material y métodosEstudio observacional retrospectivo que incluyó todos los pacientes intervenidos por hiperparatiroidismo primario con TC-4D como estudio preoperatorio, del 1 de octubre de 2016 al 1 de octubre de 2021, en un centro hospitalario de tercer nivel.
Se compararon los resultados del TC-4D, la ecografía y las exploraciones de Medicina Nuclear (gammagrafía, SPECT y SPECT-TC) con el gold standard de la exploración quirúrgica y el resultado anatomopatológico, analizando los porcentajes de lateralización correcta y localización aproximada de la glándula patológica.
ResultadosEl análisis incluyó 64 pacientes, con una curación del 93,8% (60/64). El TC-4D mostró una lateralización correcta del 57,8% (37/64) y reveló la localización aproximada de la glándula en el 48,4% (31/64). La ecografía tuvo unos porcentajes del 31,1% (19/61) y del 18% (11/61) para la lateralización correcta y la localización aproximada, respectivamente, frente a un 34,9% (22/63) y un 28,6% (18/63) de los estudios de Medicina Nuclear y un 32,7% (16/49) y un 24,5% (12/49) del SPECT-TC. Estas diferencias fueron estadísticamente significativas.
ConclusionesEl TC-4D ofrece un rendimiento aceptable para localizar las lesiones responsables del hiperparatiroidismo primario, por lo que debería considerarse su uso ante la ausencia de localización en los estudios habituales.
Primary hyperparathyroidism is a common calcium metabolism pathology caused by excessive or inadequate secretion of parathormone (PTH)1. This disease is mainly caused by parathyroid adenoma (85%), while the presence of multiglandular disease is less frequent (15%)2. Surgical treatment is indicated in symptomatic hyperparathyroidism and in asymptomatic hyperparathyroidism in patients under 50 years of age, with serum calcium 1 mg/dL above the normal limit, bone densitometry diagnostic for osteoporosis (T-score < −2.5) in the lumbar spine, hip or distal third of the radius, in the presence of vertebral fractures on imaging tests, with creatinine clearance <60 mL/min, calciuria >400 mg/day in 24-h urine in patients with increased risk of lithiasis, or in the presence of nephrolithiasis or nephrocalcinosis on imaging tests3.
Preoperative localization tests are recommended to locate the pathological gland and enable the surgeon to conduct selective parathyroidectomy, which is associated with high cure rates4. Cervical ultrasound and cervical scintigraphy with [99mTc]Tc sestaMIBI are usually the initial tests. Used in combination, they provide adequate accuracy and sensitivity4, even allowing for intraoperative monitoring of PTH to be eliminated in cases of complete concordance5, although their sensitivity may be lower in multiglandular disease6. Currently, the test that offers the greatest sensitivity is positron emission tomography/computed tomography (PET/CT) with [18F]fluorocholine7, although its use is limited by the high cost8 and limited availability.
In this context, 4-dimensional computed tomography (4D-CT) is a preoperative localization study that consists of acquiring three vascular phases (basal, arterial, and venous), assessing the behavior of the lesions according to time after the administration of intravenous contrast8. In this test, rapid uptake and washout of contrast are diagnostic of parathyroid adenoma8, which is combined with the high spatial resolution of CT to locate the pathologic gland9. This localization test offers good sensitivity for the lateralization of the lesion at nearly 81% (95% CI: 75–87), while the sensitivity for localization in the appropriate quadrant is 73% (95% CI: 69–78)10.
The objective of this study was to evaluate the performance of 4D-CT as a second-line localization study in primary hyperparathyroidism surgery, comparing its results with cervical ultrasound and nuclear medicine studies: parathyroid scintigraphy, single-photon emission computed tomography (SPECT) and SPECT/CT.
MethodsThis article follows the STROBE (Strengthening the Reporting of Observational Studies in Epidemiology) recommendations for the preparation of observational studies11.
Study design and participantsOurs is a single-center retrospective observational study that included all patients operated on for primary hyperparathyroidism who underwent 4D-CT as a preoperative study after the usual studies provided inconclusive results. The study was conducted at a tertiary hospital from October 1, 2016 to October 1, 2021.
Patients treated surgically for secondary or tertiary hyperparathyroidism, those with a non-protocol CT, or those with no subsequent follow-up were excluded from the study.
The study was accepted by the institution's Research Ethics Committee (code 290/21) and was carried out in accordance with the Declaration of Helsinki on human experiments. Given the retrospective natures of the study, we requested an exemption for obtaining informed consent, which was granted by the Research Ethics Committee.
InterventionThe initial localization studies included ultrasound and planar scintigraphy of the parathyroid with [99mTc]Tc sestaMIBI, with SPECT or SPECT/CT being possible at the discretion of the Nuclear Medicine specialist. The 4D-CT study was indicated as a second-line preoperative study due to either the absence of localization or the discordant results of previous studies. Depending on the results of these preoperative tests, the surgical intervention was performed using either a targeted or bilateral approach. An intraoperative pathological study and intraoperative monitoring of PTH were available; surgery was concluded when PTH decreased to normal ranges and at a percentage greater than 50% compared to previous values12.
The demographic variables analyzed included: sex, age, body mass index (BMI) (kg/m2), history of previous surgery, and presence of multinodular goiter. We evaluated maximum serum calcium levels (mg/dL) at diagnosis and after 6 months, as well as preoperative and postoperative PTH levels (ng/dL). We also analyzed the preoperative localization test results, including: cervical ultrasound, planar parathyroid scintigraphy with [99mTc]Tc-sestaMIBI, SPECT and SPECT/CT, and 4D-CT. The surgical variables analyzed included: the approach, the location of the adenoma, and postoperative complications. The pathological variables collected were: the result of the deferred study, maximum length of the gland (mm), maximum weight (mg), and the sum weight of the glands in the case of multiglandular disease. Cure after surgery was defined as normalized calcium levels 6 months after surgery.
The delayed pathological result, together with the description of the location of the pathological gland in surgery, was considered the ‘gold standard’ and was compared with the results of the preoperative localization studies. The scintigraphy result was added to the SPECT or SPECT/CT since the reading of these tests was performed together. To evaluate the performance of the preoperative localization tests, correct lateralization and approximate localization were analyzed as percentages. We considered the lateralization to be correct when the preoperative localization test coincided with the side (right or left) on which the pathological gland was later identified. We considered the approximate location to be correct when the pathological gland was located in the immediate area of the site predicted by the preoperative localization test.
Statistical analysisIn the descriptive analysis, categorical variables are defined as frequency (n) and percentage (%). Quantitative variables are described as mean and standard deviation (SD) when they followed normal distribution, and as median and interquartile range when they did not. The normality analysis was performed using the Shapiro-Wilk test. The percentages of correct lateralization and approximate location of the preoperative localization tests were evaluated as categorical variables in statistical hypothesis testing using the chi-squared test. The level of significance was set at 0.05. The data analysis was performed with the SPSS Statistics 23 program.
ResultsDuring the study period, 359 patients underwent surgery for hyperparathyroidism, 64 of whom were studied with a 4D-CT scan after inconclusive results of the usual studies and included in the analysis.
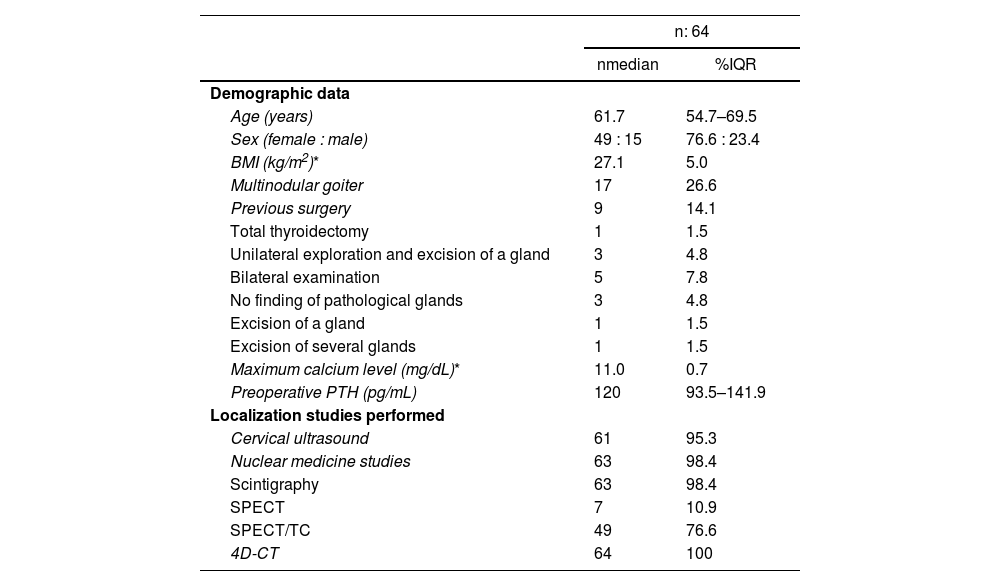
Series descriptionThe median age of the sample was 61.7 years (IQR: 54.7–69.5) with a predominance of women (76.6%; 49/64). Mean BMI was 27.1 kg/m2 (SD: 5.0). Concomitant multinodular goiter was observed in 26.6% (17/64) of patients, and 14.1% (9/64) had a history of previous cervical intervention: total thyroidectomy (1/64), unilateral exploration and excision of a gland (3/64), and bilateral cervical examination (5/64). Maximum preoperative calcium was 11.0 mg/dL (SD: 0.7), with a median preoperative PTH of 120 pg/mL (IQR: 93.5–141.9).
Cervical ultrasound was performed in 95.3% (61/64) of the sample. The 3 patients who did not undergo ultrasound had SPECT/CT performed directly. Nuclear Medicine studies were performed in 98.4% (63/64) of the sample, and the most frequently performed tests were planar scintigraphy (98.4%; 63/64) and SPECT/CT (76.6%; 49/64). In all the cases analyzed, 4D-CT was performed (100%; 64/64). These results are shown in Table 1.
Demographic data and localization tests performed.
| n: 64 | ||
|---|---|---|
| nmedian | %IQR | |
| Demographic data | ||
| Age (years) | 61.7 | 54.7–69.5 |
| Sex (female : male) | 49 : 15 | 76.6 : 23.4 |
| BMI (kg/m2)* | 27.1 | 5.0 |
| Multinodular goiter | 17 | 26.6 |
| Previous surgery | 9 | 14.1 |
| Total thyroidectomy | 1 | 1.5 |
| Unilateral exploration and excision of a gland | 3 | 4.8 |
| Bilateral examination | 5 | 7.8 |
| No finding of pathological glands | 3 | 4.8 |
| Excision of a gland | 1 | 1.5 |
| Excision of several glands | 1 | 1.5 |
| Maximum calcium level (mg/dL)* | 11.0 | 0.7 |
| Preoperative PTH (pg/mL) | 120 | 93.5–141.9 |
| Localization studies performed | ||
| Cervical ultrasound | 61 | 95.3 |
| Nuclear medicine studies | 63 | 98.4 |
| Scintigraphy | 63 | 98.4 |
| SPECT | 7 | 10.9 |
| SPECT/TC | 49 | 76.6 |
| 4D-CT | 64 | 100 |
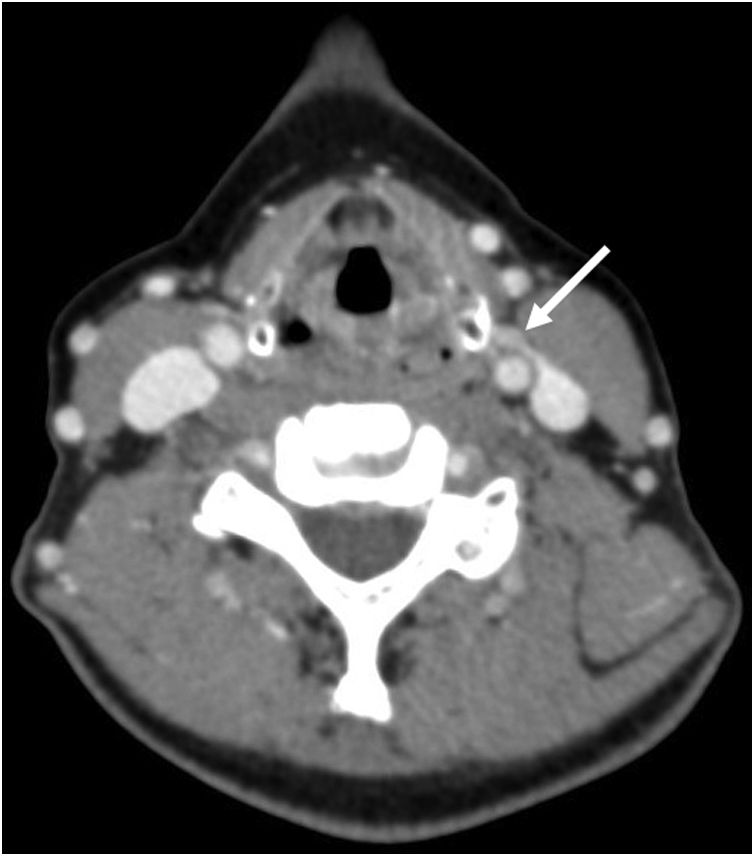
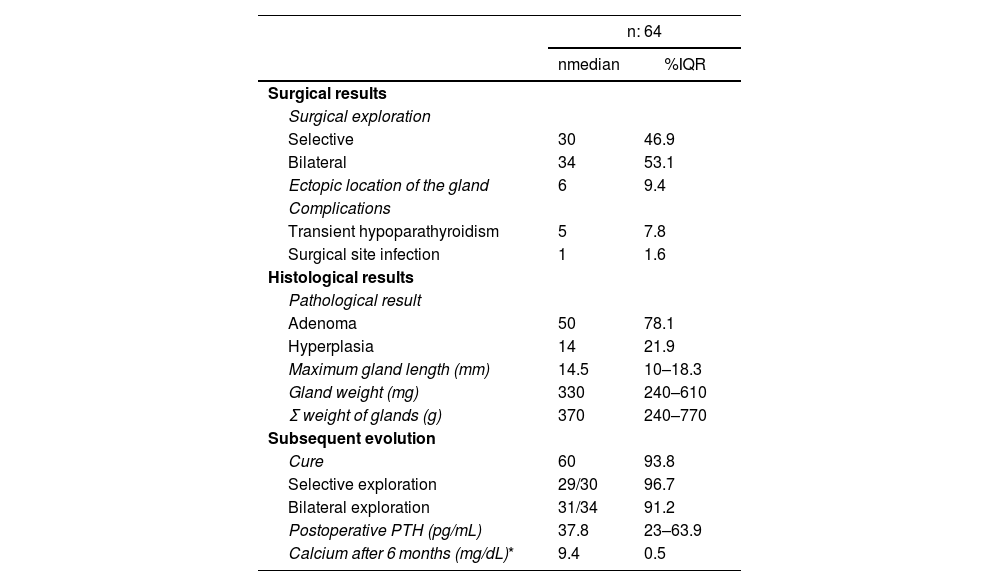
Selective parathyroidectomy was performed in 46.9% (30/64) of the sample and bilateral cervical exploration in the remaining 51.7% (34/64). In 9.4% of the cases (6/64), this was due to an ectopic gland (Fig. 1). Postoperative complications included 5 cases (7.8%) of transient hypoparathyroidism and one case (1.6%) of surgical wound infection. No complications related to the recurrent laryngeal nerve or other definitive complications were observed.
The final pathological result was adenoma in 78.1% of cases (50/64) and hyperplasia in the remaining 21.9% (14/64). The median maximum weight of the pathological gland was 330 mg (IQR: 240–610). Postoperative PTH dropped to 37.8 pg/mL (IQR: 23–63.9), while mean calcium 6 months after the intervention was 9.4 mg/dL (SD: 0.5). The cure rate after surgery was 93.8% (60/64), with a cure rate of 96.7% (29/30) on selective examination and 91.2% (31/34) on bilateral examination. These results are shown in Table 2.
Surgical results, histological results and subsequent evolution.
| n: 64 | ||
|---|---|---|
| nmedian | %IQR | |
| Surgical results | ||
| Surgical exploration | ||
| Selective | 30 | 46.9 |
| Bilateral | 34 | 53.1 |
| Ectopic location of the gland | 6 | 9.4 |
| Complications | ||
| Transient hypoparathyroidism | 5 | 7.8 |
| Surgical site infection | 1 | 1.6 |
| Histological results | ||
| Pathological result | ||
| Adenoma | 50 | 78.1 |
| Hyperplasia | 14 | 21.9 |
| Maximum gland length (mm) | 14.5 | 10–18.3 |
| Gland weight (mg) | 330 | 240–610 |
| Σ weight of glands (g) | 370 | 240–770 |
| Subsequent evolution | ||
| Cure | 60 | 93.8 |
| Selective exploration | 29/30 | 96.7 |
| Bilateral exploration | 31/34 | 91.2 |
| Postoperative PTH (pg/mL) | 37.8 | 23–63.9 |
| Calcium after 6 months (mg/dL)* | 9.4 | 0.5 |
Σ: sum.
Ultrasound achieved correct lateralization in 31.1% (19/61) of cases and correctly indicated the approximate location of the pathological gland in 18% (11/61) of patients. The addition of nuclear medicine studies showed correct lateralization in 34.9% (22/63) and revealed the approximate location in 28.6% (18/63) of the sample. When we exclusively analyzed the patients with SPECT/CT, the percentage of correct lateralization with this test was 32.7% (16/49), and the percentage of approximate localization was 24.5% (12/49). With 4D-CT, the correct lateralization rate was 57.8% (37/64), and the approximate location of the pathological gland was correct in 48.4% (31/64) of the cases. These results are shown in Table 2.
The correct lateralization rate of 4D-CT was statistically superior to cervical ultrasound (P = .001), the nuclear medicine studies (P = .018), and SPECT/CT (P = .010). The correct approximate location rate of 4D-CT was also statistically superior to that indicated by cervical ultrasound (P = .002), nuclear medicine studies (P = .002), and SPECT/CT (P = .001) (Table 3).
Results of preoperative localization studies.
| n: 64 | ||
|---|---|---|
| nmedian | %IQR | |
| Cervical ultrasound | ||
| Correct lateralization | 19/61 | 31.1 |
| Approximate location | 11/61 | 18 |
| Nuclear medicine studies | ||
| Correct lateralization, nuclear med | 22/63 | 34.9 |
| Approximate location, nuclear med | 18/63 | 28.6 |
| Correct lateralization, SPECT/CT | 16/49 | 32.7 |
| Approximate location, SPECT/CT | 12/49 | 24.5 |
| 4D-CT | ||
| Correct lateralization | 37/64 | 57.8 |
| Approximate location | 31/64 | 48.4 |
The location and number of pathological glands localized/not localized by 4D-CT is shown in Fig. 2 (adapted from Powell et al.13). 4D-CT was able to resolve the discrepancy between the results of the cervical ultrasound and the nuclear medicine tests in 16 cases (26.2%). Furthermore, it was decisive for localization in 11 cases (17.2%), in which all previously performed localization tests had been negative. The characteristics of this last subgroup of patients are shown in Table 4.
Analysis of patients with negative results from usual localization studies and decisive 4D-CT for preoperative localization of patients not cured.
| Sex | Age | Previous surgery | Maximum calcium level (mg/dL) | PTH pre-op (pg/mL) | 4D-CT | Approach | Localization of the pathological gland | Histological result | PTH post-op (pg/mL) | Calcium after 6 m (mg/dL) |
|---|---|---|---|---|---|---|---|---|---|---|
| Negative result of usual localization studies and decisive 4D-CT | ||||||||||
| F | 81.1 | No | 12.3 | 141.7 | Left pathological glands | Bilateral | Left superior and inferior | Hyperplasia | 49.9 | 9.7 |
| F | 67.3 | Bilateral exploration, no pathological glands found | 10.5 | 71.0 | Right pathological gland | Bilateral | Right inferior | Adenoma | 21.0 | 9.2 |
| F | 72.3 | Unilateral exploration and excision of a gland | 11.1 | 169.0 | Right pathological and left intrathymic glands | Bilateral | Right superior and inferior and intrathymic | Hyperplasia | 81.0 | 9.7 |
| F | 50.9 | Bilateral exploration with excision of a gland | 11.1 | 187.8 | Adenoma inferior to the left submaxillary gland | Selective | Inferior-posterior to the left submaxillary gland | Adenoma | 23.0 | 8.7 |
| F | 60.4 | No | 10.9 | 165.0 | Left inferior adenoma | Bilateral | Left inferior | Adenoma | 27.0 | 9.2 |
| M | 80.3 | No | 11.6 | 156.0 | Right adenoma | Selective | Right superior | Adenoma | 106.0 | 9.6 |
| F | 74.6 | No | 10.7 | 132.8 | Left superior adenoma | Bilateral | Left superior | Adenoma | 46.7 | 9.5 |
| F | 61.7 | No | 10.3 | 127.5 | Bilateral inferior pathological glands | Bilateral | Left inferior and right inferior | Hyperplasia | 55.0 | 9.7 |
| F | 65.1 | No | 10.6 | 91.0 | Left adenoma | Bilateral | Left superior | Adenoma | 67.0 | 8.7 |
| M | 63.0 | No | 11.3 | 85.1 | Right inferior adenoma | Selective | Right inferior | Adenoma | 38.6 | 10.0 |
| F | 67.9 | No | 11.5 | 81.1 | Right superior adenoma | Selective | Right superior | Adenoma | 19.7 | 8.9 |
| Patients not cured | ||||||||||
| F | 72.3 | No | 10.8 | 193.0 | Pathological glands not located | Bilateral | Right superior and inferior | Hyperplasia | 122.0 | 10.6 |
| F | 69.5 | No | 11.2 | 136.0 | Left inferior adenoma | Bilateral | Superior and inferior right and inferior left | Hyperplasia | 21.4 | 10.7 |
| M | 75.7 | No | 10.5 | 130.0 | Right adenoma | Bilateral | Right superior and inferior | Hyperplasia | 115.0 | 10.2 |
| F | 75.4 | No | 11.3 | 123.0 | Right inferior adenoma | Selective | Right inferior | Adenoma | 105.0 | 10.7 |
Pre-op: preoperative; Post-op: postoperative; F: female; M: male.
The patients not cured despite surgical treatment are also described in detail in Table 4. Three cases were due to multiglandular disease, in which, despite bilateral cervical exploration, normalization of calcium levels was not achieved, nor was PTH normalized in the case of normocalcemic hyperparathyroidism (3rd patient). The last case was a selective approach, in which the gland identified by 4D-CT was located intraoperatively, but it persisted with elevated calcium and PTH, so it could also have been another case of hyperplasia.
DiscussionUtilized as a second-line test after usual test results were inconclusive, 4D-CT indicated the correct lateralization of the pathological gland causing the primary hyperparathyroidism in 57.8% (37/64) of the sample as well as the approximate location of the pathological gland in 48.4% (31/64). In 2006, the first study published by Rodgers et al.14 reported a sensitivity of 4D-CT for lateralization of the pathological gland of 88%, which was higher than cervical ultrasound (57%) and cervical scintigraphy with [99mTc]Tc-sestaMIBI (65%). Sensitivity for exact localization of the lesion was also better with 4D-CT (70%) than cervical ultrasound (29%) and cervical scintigraphy (33%). Our results are more modest than the Rodgers et al. study14, but they are within the range described in the literature when using the technique in patients with difficult preoperative localization in whom the usual studies had not offered favorable results15–17. In these studies, the sensitivity is between 49%16 and 60%17, which is in line with the 57.8% described in our sample. Causes that make localization difficult include the presence of small, ectopic adenomas, or hyperplasia, which reduces the identification of the pathological gland by any preoperative localization method.
Studies using 4D-CT as the initial preoperative localization test show very high sensitivities, ranging from 77% to 79%18–21. Thus, according to the systematic review by Kluijfhout et al.10 the sensitivity of 4D-CT was 81% (95% CI: 75–87) for lateralization of the lesion and 73% (95% CI: 69–78) for localization in the appropriate quadrant. Another more recent meta-analysis by Wan et al.9 from 2021 also concluded that 4D-CT had better sensitivity than SPECT/CT with [99mTc]Tc-sestaMIBI (85% [95% CI: 69–94] vs 68% [95% CI: 51–80]). These results9,10 are much superior to those obtained by 4D-CT in our study as a second-line test. Logically, expanding the indications of 4D-CT to patients with typical localization would probably provide better percentages of correct localization, although it would be difficult to justify given the greater exposure to ionizing radiation of this test compared to other more innocuous techniques like ultrasound.
4D-CT may also be useful in cases of persistent or recurrent hyperparathyroidism, the causes of which include a higher proportion of patients with multiglandular disease (28.4%) or ectopic parathyroid glands (44.3%)22. The surgical indication in these patients must be carefully evaluated, since reoperation may present a higher rate of complications22. In the Mortenson et al. article23, the sensitivity of 4D-CT for lesion lateralization in the operated neck was 98% (95% CI: 86–100), which was higher than ultrasound (46% [95% CI: 31 62]) or [99mTc]Tc-sestaMIBI scintigraphy (54% [95% CI: 38–69]). Similar results were obtained by Hamidi et al.24 in recurrent hyperparathyroidism, where 4D-CT had a sensitivity of 77.4%, better than ultrasound (38.5%) or cervical scintigraphy (46%).
Currently, the diagnostic sensitivity of 4D-CT is only surpassed by PET/CT with [18F]fluorocholine. According to the systematic review by Piccardo et al.7, this test has a sensitivity of 89% compared to a sensitivity of 77% for 4D-CT in this study. In our setting, the study by Ballester Vázquez et al.25 managed to detect hyperfunctioning parathyroid tissue on PET/CT with [18F]fluorocholine in 85.3% of their study sample, achieving cure in 87% of cases. However, given the difficulties for a broader use of PET/CT, 4D-CT may be a useful alternative in hyperparathyroidism that is difficult to locate.
The limitations of our study include the lack of blinding, so the radiologists, nuclear medicine physicians and surgeons had information about the tests performed previously. That is why the results of the nuclear medicine functional tests have been offered jointly with the result of the SPECT/CT anatomical-functional test, since the information provided by these tests was considered jointly. Undoubtedly, the best design to evaluate these localization tests would be a prospective analysis that blindly compared 4D-CT, SPECT/CT and PET/CT with [18F]fluorocholine against the ‘gold standard’ of surgical results and pathological results. Meanwhile, we believe that our study is a good representation of the usual clinical practice of medical centers that use 4D-CT as a second-line test.
Conclusion4D-CT offers acceptable performance for locating the lesions responsible for primary hyperparathyroidism, so its use should be considered as a second-line test in the absence of localization after applying the usual studies.
Compliance with ethical standardsThis study was accepted by the institution's Research Ethics Committee (code 290/21) and conducted in accordance with the Declaration of Helsinki on human experiments. Given the retrospective nature of the study, We requested an exemption for obtaining informed consent, which was granted by the Research Ethics Committee.
FinancingThis research has received no specific aid from public agencies, the commercial sector or non-profit entities.
Conflict of interestNone.