An abdominal pseudohernia is a protrusion of the abdominal wall that resembles a hernia, but differs from a true hernia in that there is no real muscle disruption and all muscle layers remain intact.1 Pseudohernias are rare conditions that are caused by atrophy of the abdominal musculature. They have been described in association with neuropathy sultrasoundndary to medical causes2,3 or post-lumbotomy.4 Pseudohernias resulting from medical causes are resolved partially or totally,2,3 while those sultrasoundndary to a surgical complication do not improve.4 To date, they have not been described after spinal cord injury. The objective of this paper is to reported the cases of 3 patients who developed abdominal pseudohernias after spinal cord injury. These patients were identified in the outpatient clinic of the spinal cord injury unit from 2009 to 2015. At a follow-up visit, each had reported diffuse symptoms, including unilateral abdominal heaviness, lumbar discomfort or imbalance while sitting, but no clear limitations for activities of daily living. Two of these patients had been referred by their family doctor to the general surgery department with the diagnosis of abdominal hernia.
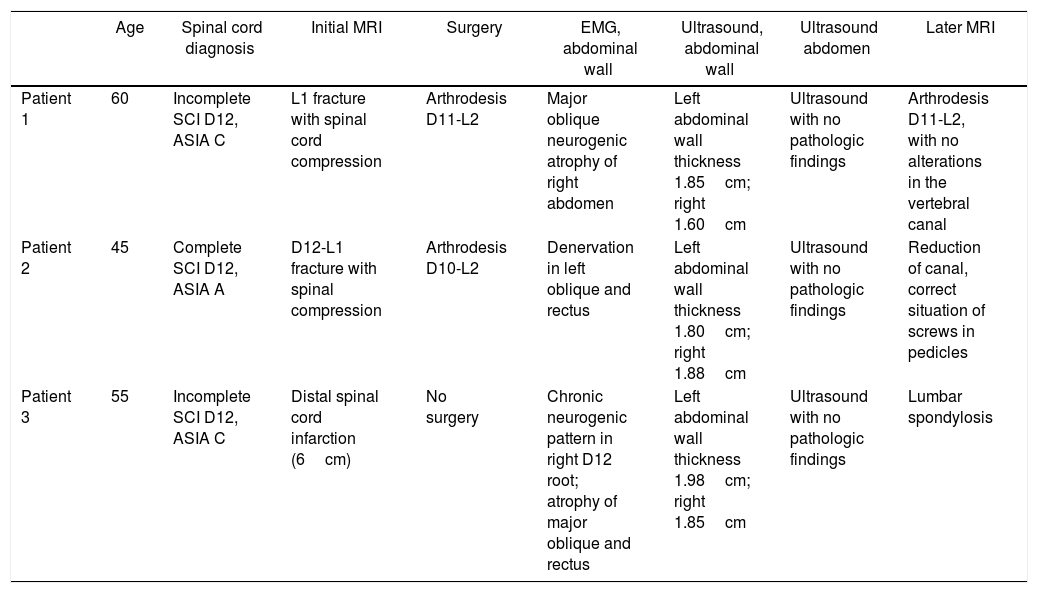
The patients began reporting symptoms 4–6 months after the spinal cord injury. The 3 patients were males between the ages of 45 and 57. In 2 cases, the spinal cord injury was caused by a trauma injury (D12-L1 fractures), and in the third case the origin of the spinal cord injury was medullary ischemia affecting the lumbosacral spinal cord segments and produced an incomplete medullary lesion. Clinical examination revealed abdominal asymmetry (Fig. 1). The cranial magnetic resonance imaging (MRI) study of the vertebral-medullary trauma causing the spinal cord injury was reviewed, and an abdominal ultrasound, electromyogram of the abdominal wall and measurement of the abdominal wall thickness by ultrasound were requested, as well as a new spinal MRI if there had been surgery after the spinal cord injury (Table 1). In the 3 cases, there was unilateral involvement of the L1 root, which caused unilateral thinning of the abdominal wall. The patients, who have continued in follow-up in the outpatient clinic of the ULM, have continued to present the same clinical symptoms and examination results for 2–8 years. Described by Taylor in 1895,5 abdominal pseudohernia has usually been described in various studies as a medical complication of a herpes zoster infection2,6,7 or diabetic radiculopathy.3,8,9 Likewise, it has also been described after surgery,4 invasive diagnostic procedures10 or rib fractures. Unlike the cases described in the literature where the neurological lesion occurred in the peripheral nerve, the cases presented in this study relate the origin of the pseudohernia with a unilateral lesion of the anterior horn of the spinal cord.
Type of Injury and Complementary Tests.
| Age | Spinal cord diagnosis | Initial MRI | Surgery | EMG, abdominal wall | Ultrasound, abdominal wall | Ultrasound abdomen | Later MRI | |
|---|---|---|---|---|---|---|---|---|
| Patient 1 | 60 | Incomplete SCI D12, ASIA C | L1 fracture with spinal cord compression | Arthrodesis D11-L2 | Major oblique neurogenic atrophy of right abdomen | Left abdominal wall thickness 1.85cm; right 1.60cm | Ultrasound with no pathologic findings | Arthrodesis D11-L2, with no alterations in the vertebral canal |
| Patient 2 | 45 | Complete SCI D12, ASIA A | D12-L1 fracture with spinal compression | Arthrodesis D10-L2 | Denervation in left oblique and rectus | Left abdominal wall thickness 1.80cm; right 1.88cm | Ultrasound with no pathologic findings | Reduction of canal, correct situation of screws in pedicles |
| Patient 3 | 55 | Incomplete SCI D12, ASIA C | Distal spinal cord infarction (6cm) | No surgery | Chronic neurogenic pattern in right D12 root; atrophy of major oblique and rectus | Left abdominal wall thickness 1.98cm; right 1.85cm | Ultrasound with no pathologic findings | Lumbar spondylosis |
ASIA: American Spinal Injury Association; D: dorsal; SCI: spinal cord injury; MRI: magnetic resonance imaging.
On examination, the 3 patients presented better sensory preservation at D12 (residual sensitivity) on one side; 2 were incomplete spinal cord injuries and another was complete. For the differential diagnosis, abdominal hernia was ruled with abdominal ultrasound, which confirmed the integrity of the abdominal wall and the normal visceral location of its contents. Likewise, in the 3 ultrasounds of the abdominal wall, a reduction in the thickness of the abdominal wall was observed, which in the 3 cases has occurred at the expense of the outermost muscular layer (greater oblique dependent on the D12 root), with greater preservation of the thickness of the minor oblique and the transverse muscle (L1). Posterior MRI of the spinal column ruled out any associated injuries. The authors suggest that the 3 patients presented asymmetric medullary lesions that would affect the anterior root to the union of the first and sultrasoundnd motor neurons on one side of the cord, with preservation of the contralateral side at that level, which would result in atrophy of the musculature of the affected hemiabdomen. Although the cases presented correspond to very rare spinal cord injuries (spinal cord injury at D12 on one side, with preservation on the contralateral side), similar cases must have undoubtedly presented previously on numerous occasions. However, according to the authors’ review of the literature, no reports have been published to date. This may possibly be due to the fact that, among other things, this complication scarcely produces remarkable symptomatology within the context of the spinal cord injury itself and does not usually require treatment. Abdominal pseudohernia is a lesion that may appear after asymmetric spinal cord injury at D12. Although the symptoms that it causes are minimal and do not usually require treatment, this pathology should be included in the differential diagnosis of abdominal hernias.
Please cite this article as: Bárbara-Bataller E, Martín del Rosario F, Méndez-Suárez JL, Alemán-Sánchez C, Sosa Henríquez M. Seudohernia abdominal tras lesión medular. A propósito de 3 casos. Cir Esp. 2018;96:587–589.
Part of the content of this study was presented as a scientific poster at the 34th Symposium of the Spanish Paraplegia Society held from October 18 to 20 in Maspalomas, Gran Canaria, Spain.