The shortage of available beds and the increase in Emergency Department pressure can cause some patients to be admitted in wards with available beds assigned to other services (outlying patients). The aim of this study is to assess the frequency, types of complications and costs of outlying patients.
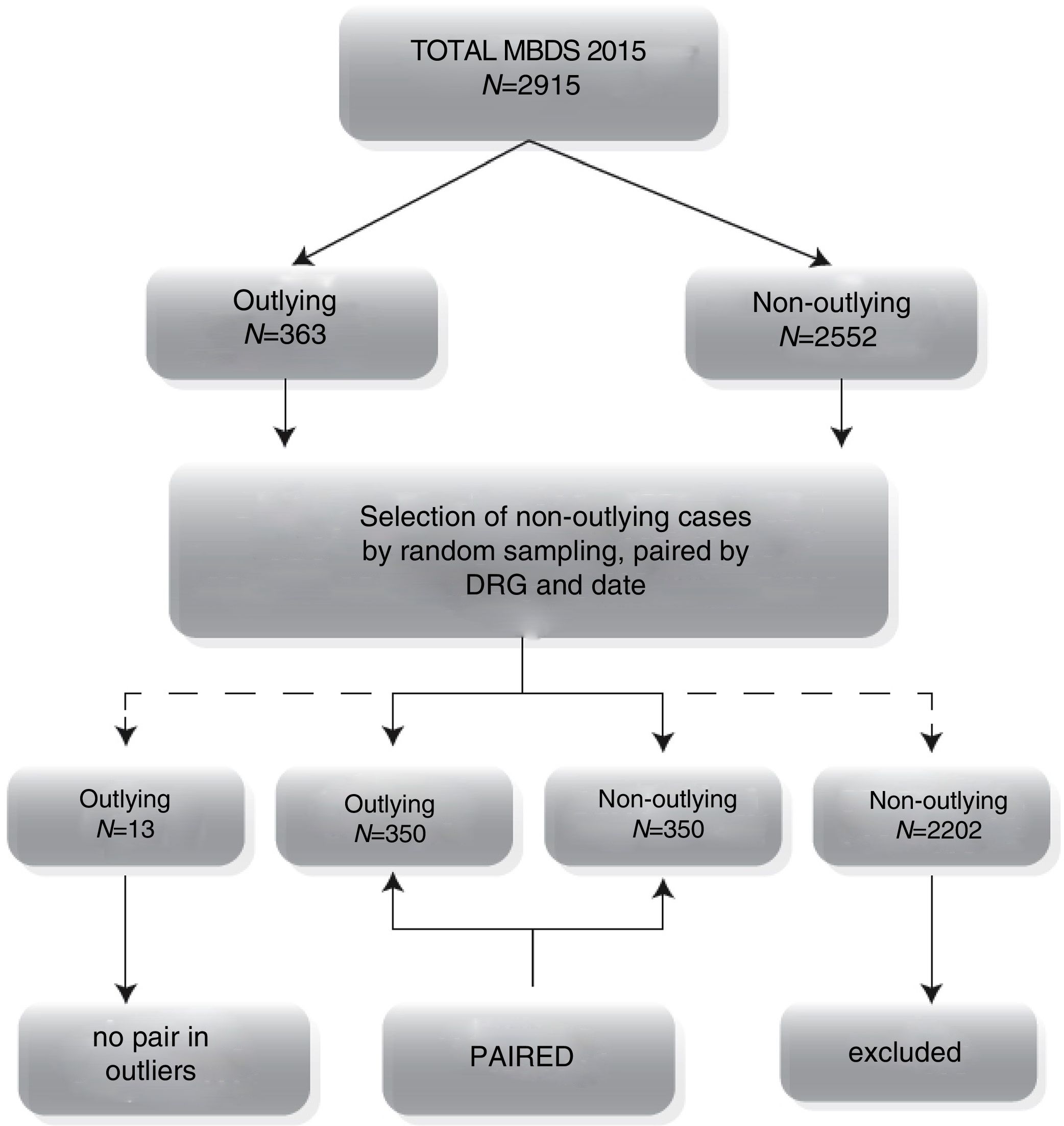
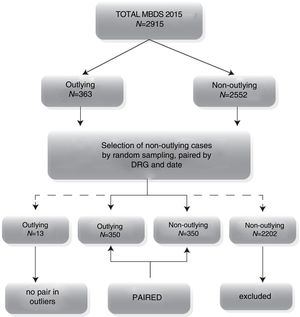
MethodsUsing a retrospective cohort model, we analyzed the 2015 general and digestive surgery records (source: Minimum Basic Data Set and economic database). After selecting all outlying patients, we compared the complications, length of stay, costs and consequences of complications against a randomized sample of non-outlying patients with the same DRG and date of episode for every outlying patient, obtaining one non-outlying patient for each selected outlying patient. Thirteen outlying patients with no non-outlying patient pair were excluded from the study.
ResultsFrom a total of 2915 patients, 363 (12.45%) were outlying patients. A total of 350 outlying patients were analyzed versus 350 non-outlying patients. There were no significant differences in complications (9.4% vs 8.3%), length of stay (4.33 vs 4.65 days) or costs (€3034.12 vs €3223.27). Outlying patients men presented a significantly higher risk of complications compared to women (RR=2.10). Outlying patients presented complications after 2.5 or more days.
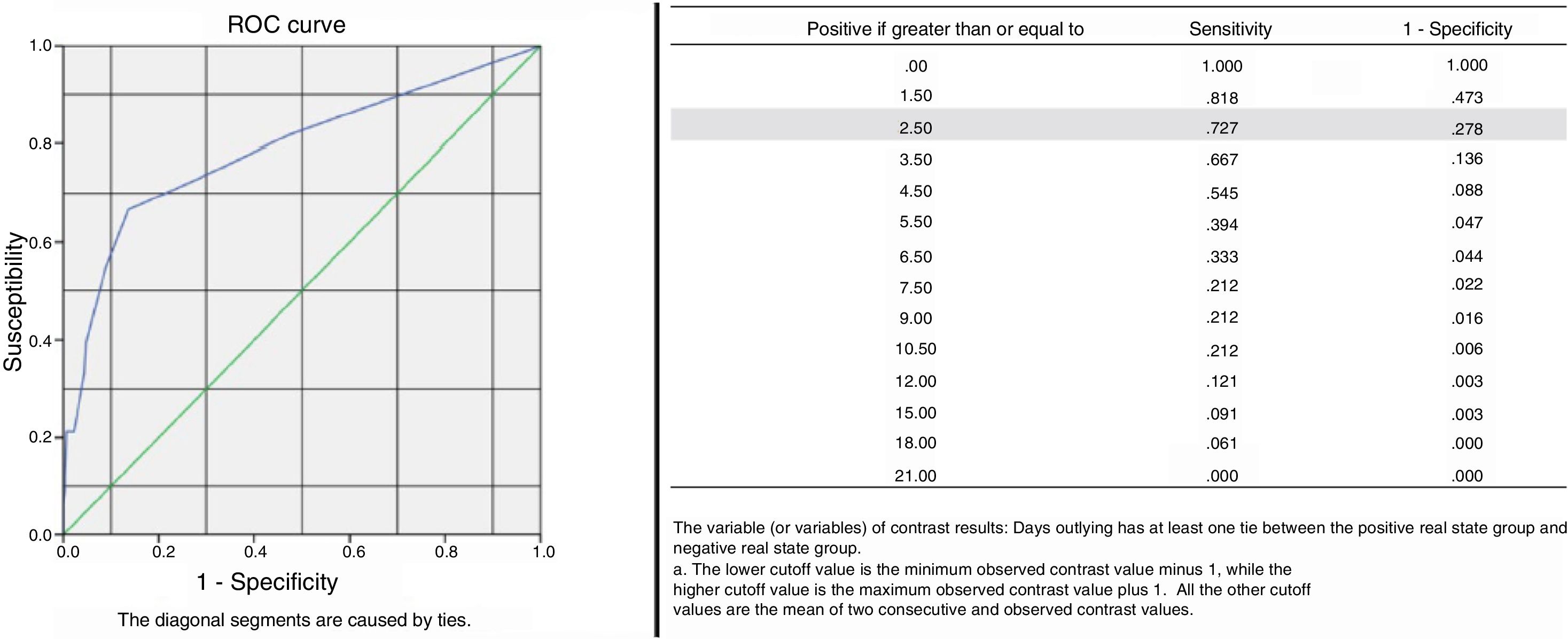
ConclusionsWhen outlying admissions become necessary, the selection of patients with less complex pathologies does not increase complications or their consequences (ICU admissions, readmissions, reoperations or mortality), hospital stays or costs. Only in cases of prolonged outlying stays of more than 2.5 days, or in males, may more complications appear. Therefore, male outliers should be avoided in general, and patients should be transferred to the proper ward if a length of stay beyond 2.5 days is foreseen.
El descenso de camas disponibles y el aumento de la presión de Urgencias provocan que algunos pacientes sean ingresados en salas con camas libres pertenecientes a otros servicios (llamados pacientes ectópicos). El objetivo de este artículo es analizar la frecuencia, los tipos de complicación y los costes en los pacientes ectópicos.
MétodosEstudio retrospectivo de cohortes de pacientes ingresados a cargo de cirugía general y digestiva durante 2015 (fuente: Conjunto Mínimo Básico de Datos y contabilidad analítica). Comparamos las complicaciones, las estancias, los costes y las consecuencias de las complicaciones en todos los ectópicos, frente a un muestreo aleatorio de tantos pacientes no ectópicos como ectópicos ingresados en la misma fecha y con igual GRD. Se excluyen los 13 ectópicos sin par en los no ectópicos.
ResultadosDe un total de 2.915 pacientes, 363 (12,45%) fueron ectópicos. Se analizan un total de 350 ectópicos frente a 350 no ectópicos. No hubo diferencias significativas en las complicaciones (9,4 vs 8,3%), las estancias (4,33 vs 4,65 días) ni el coste (3.034,12 vs 3.223,27€). Los hombres ectópicos presentan un riesgo significativamente mayor de complicaciones respecto a las mujeres (RR=2,10). Los ectópicos presentaron complicaciones a partir de 2,5 o más días como ectópicos.
ConclusionesAl necesitar ingresos ectópicos, seleccionando pacientes de baja complejidad, no aumentamos las complicaciones ni sus consecuencias (ingresos en la UCI, reingresos, reintervenciones o mortalidad), estancias o costes. Solo en caso de prolongar la estancia ectópica más de 2,5 días, o en varones, pueden aparecer más complicaciones, por lo que deberían evitarse ectópicos varones, en general, y plantearse su traslado si se prevé una estancia más allá de 2,5 días.
In recent years, due to the decrease in the number of available hospital beds1 and the increase in the frequency of visits and pressure in the Emergency Room (rate of emergency admissions), certain hospitalization units are forced to occupy more hospital beds than they are allocated. This overload means that some patients have to be admitted to free beds in other units.2 Thus, “outlying patients” (OP) are defined as patients who are admitted to beds in wards that are not specifically assigned for this type of hospitalization.3
The dispersion of these patients in the hospital generates organizational problems in the department as well as a decrease in the quality of care, fundamentally associated with the differences in the level of specialization, which would not have been an issue if the patient had been hospitalized in the correct ward. Theoretically, the outlying patient situation leads to delays in treatment, hospital discharge, complementary studies or interconsultations with other specialists.4 An increase in the average time spent by the medical team with each patient5 and an increased risk of readmissions has also been reported.6 Furthermore, if attempts are made to relocate patients with intrahospital transfers, the number of OP would decrease at the expense of increasing transfers, which would slow down admissions.
The selection of “healthier” patients for outlying hospital admission, expecting that their management will be less problematic,7–9 may suggest that they will be given less priority.10 Moreover, there are presumably greater difficulties in the care provided by nursing staff less trained for diseases that are less common in their ward. Studies in trauma patients11 have found significant differences in the treatment of patients who were admitted to the trauma ward and treated by specialized nursing staff versus those who were not, while also identifying the existence of dangerous situations. In addition, the OP were discharged later.
Long hospital stays involve higher costs and a higher probability of complications,6,12 which is in conflict with the intention of decreasing hospital stays and the number of beds in use, as well as improving quality.
Suggestions have been made regarding the decision-making process for admitting patients, and it seems reasonable to think that the decision to admit OP, even though it is a solution to the limited number of hospital beds, entails additional problems. These include increased complications, readmissions, costs and psychological pressure for patients and relatives, which should be studied in greater depth.13
Our objective is to compare the frequency and types of complications in patients admitted to the General and Digestive Surgery Service (GDS) in terms of their outlying admission or not, as well as their influence on hospital stays and costs.
MethodsA retrospective cohort study including patients admitted to the GDS of a regional public hospital, comparing OP versus non-outlying patients (non-OP).
In a specifically developed database, records from the Minimum Basic Data Set from 2015 were collected and correlated with economic data obtained from the InforCOAN HyD analytical accounting source.14
We defined OP as patients who were admitted to a functional nursing area other than those assigned to GDS. In the case of transfer to GDS beds, patients were considered OP when the ectopic stay was at least half of the total.
Patient selection was done by sampling consecutive OP cases, and a random sampling. Thus, for each OP, a non-OP was randomly included from among all patients who were admitted in the same period, with the same DRG as the corresponding OP. When there were no simultaneous pairs, the OP was excluded from the analysis.
We defined “complication” as any deviation from the normal, symptomatic or asymptomatic postoperative course; “sequela” as an effect inherent to the surgery itself that appears afterwards; and “failure” when the ultimate purpose of the surgery was not achieved.15 Therefore, only complications, and not sequelae or failures, were the object of this study.
The costs were calculated according to the methodology of aggregate costs per DRG and corrected according to the room usage rate, as previously described by Gómez-Rosado et al.16 The project was approved by the Ethics Committee.
Statistical AnalysisAfter the descriptive analysis of the demographic variables, we evaluated the measures of frequency (incidence, cumulative incidence, relative risk [RR]) for the qualitative variables as well as measures of central tendency and dispersion for the quantitative variables, for both groups, comparing the presence and/or absence of complications. For the qualitative variables, we used the Chi-squared test, and the analysis of variance for unpaired samples was used for the quantitative variables, both with a 95% confidence interval. The Kolmogorov–Smirnov normality test was applied, and nonparametric tests were applied in cases of non-normal distribution. The homogeneity of both distributions was evaluated using the Chi-squared test and the Levene test or the Mann–Whitney U test, depending on the normality. The ROC curve was also performed to calculate the number of days as OP associated with the presence of complications. All this was carried out with the IBM-SPSS Statistics 20.0.0 software.
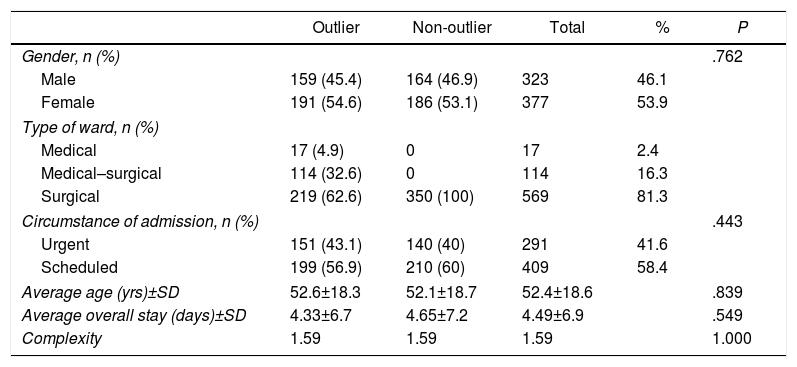
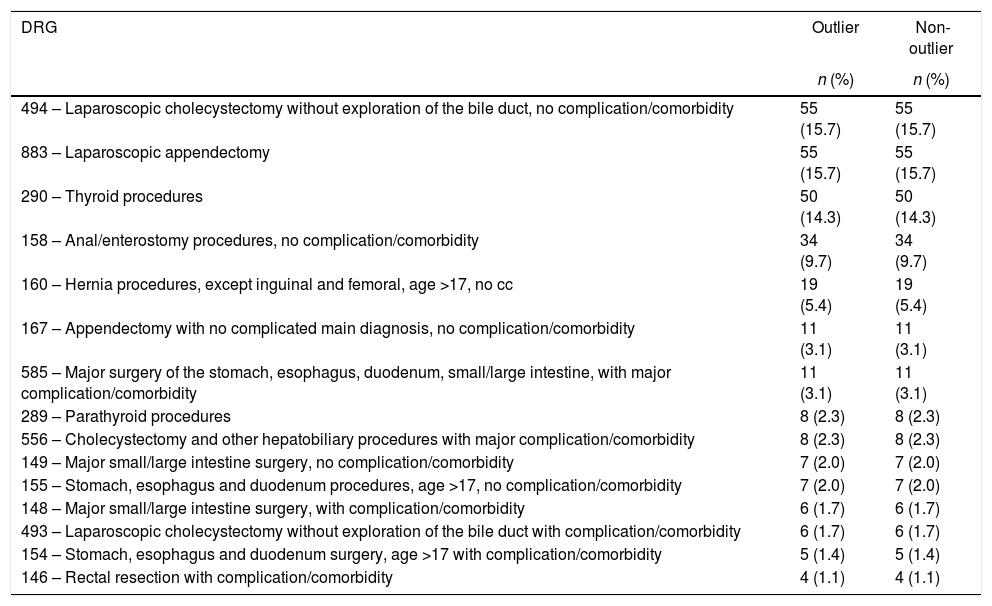
ResultsThe Minimum Basic Data Set for 2015 included 2915 discharges, 363 (12.4%) of which were OP and 2552 (87.6%) non-OP. Out of the total, 13 OP were discarded as they did not have a comparable non-OP pair, leaving a total of 350 in each group, in accordance with the methodology. Fig. 1 shows the distribution of patients and Table 1 their basic characteristics. Table 2 lists the 15 most frequent DRG included in the study (out of a total of 52).
Basic Characteristics of All Patients.
| Outlier | Non-outlier | Total | % | P | |
|---|---|---|---|---|---|
| Gender, n (%) | .762 | ||||
| Male | 159 (45.4) | 164 (46.9) | 323 | 46.1 | |
| Female | 191 (54.6) | 186 (53.1) | 377 | 53.9 | |
| Type of ward, n (%) | |||||
| Medical | 17 (4.9) | 0 | 17 | 2.4 | |
| Medical–surgical | 114 (32.6) | 0 | 114 | 16.3 | |
| Surgical | 219 (62.6) | 350 (100) | 569 | 81.3 | |
| Circumstance of admission, n (%) | .443 | ||||
| Urgent | 151 (43.1) | 140 (40) | 291 | 41.6 | |
| Scheduled | 199 (56.9) | 210 (60) | 409 | 58.4 | |
| Average age (yrs)±SD | 52.6±18.3 | 52.1±18.7 | 52.4±18.6 | .839 | |
| Average overall stay (days)±SD | 4.33±6.7 | 4.65±7.2 | 4.49±6.9 | .549 | |
| Complexity | 1.59 | 1.59 | 1.59 | 1.000 | |
Correlation and Frequency of the 15 Most Frequent DRG Included in Each Cohort.
| DRG | Outlier | Non-outlier |
|---|---|---|
| n (%) | n (%) | |
| 494 – Laparoscopic cholecystectomy without exploration of the bile duct, no complication/comorbidity | 55 (15.7) | 55 (15.7) |
| 883 – Laparoscopic appendectomy | 55 (15.7) | 55 (15.7) |
| 290 – Thyroid procedures | 50 (14.3) | 50 (14.3) |
| 158 – Anal/enterostomy procedures, no complication/comorbidity | 34 (9.7) | 34 (9.7) |
| 160 – Hernia procedures, except inguinal and femoral, age >17, no cc | 19 (5.4) | 19 (5.4) |
| 167 – Appendectomy with no complicated main diagnosis, no complication/comorbidity | 11 (3.1) | 11 (3.1) |
| 585 – Major surgery of the stomach, esophagus, duodenum, small/large intestine, with major complication/comorbidity | 11 (3.1) | 11 (3.1) |
| 289 – Parathyroid procedures | 8 (2.3) | 8 (2.3) |
| 556 – Cholecystectomy and other hepatobiliary procedures with major complication/comorbidity | 8 (2.3) | 8 (2.3) |
| 149 – Major small/large intestine surgery, no complication/comorbidity | 7 (2.0) | 7 (2.0) |
| 155 – Stomach, esophagus and duodenum procedures, age >17, no complication/comorbidity | 7 (2.0) | 7 (2.0) |
| 148 – Major small/large intestine surgery, with complication/comorbidity | 6 (1.7) | 6 (1.7) |
| 493 – Laparoscopic cholecystectomy without exploration of the bile duct with complication/comorbidity | 6 (1.7) | 6 (1.7) |
| 154 – Stomach, esophagus and duodenum surgery, age >17 with complication/comorbidity | 5 (1.4) | 5 (1.4) |
| 146 – Rectal resection with complication/comorbidity | 4 (1.1) | 4 (1.1) |
Of the total number of OP, 17 (4.9%) were admitted to medical wards, 114 (32.6%) to medical-surgical wards and 219 (62.6%) to other surgical wards. OP were urgent in 151 patients (43.1%) and scheduled in 199 (56.9%), while 140 (40%) non-OP were urgent and 210 (60%) scheduled. All the variables (gender, age and admission circumstances) complied with the rules of homogeneity. Of course, the complexity was exactly the same because of the sampling method, with a value of 1.59.
There was no difference (P=.549) in the mean hospital stay between the two groups (4.33±6.7 vs 4.65±7.2 days for non-OP and OP, respectively).
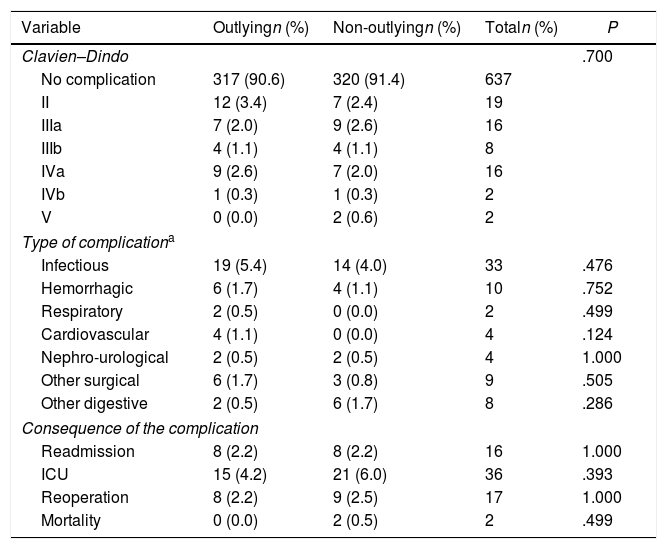
The majority did not present complications (91.0%), and the distribution in both groups did not show statistically significant differences, both for the presence of complications and well as its degree according to the Clavien–Dindo classification, as observed in Table 3. When we subclassified the complications into the 7 types described, we found that all (except “other digestive”) were more frequent in OP, but this difference was not statistically significant. This also occurred with the consequences resulting from complications (readmission, admission to the ICU, reoperation and mortality): no statistically significant differences were found (P>.05).
Distribution of Types and Consequences of Complications According to the Outlying/Non-outlying Location.
| Variable | Outlyingn (%) | Non-outlyingn (%) | Totaln (%) | P |
|---|---|---|---|---|
| Clavien–Dindo | .700 | |||
| No complication | 317 (90.6) | 320 (91.4) | 637 | |
| II | 12 (3.4) | 7 (2.4) | 19 | |
| IIIa | 7 (2.0) | 9 (2.6) | 16 | |
| IIIb | 4 (1.1) | 4 (1.1) | 8 | |
| IVa | 9 (2.6) | 7 (2.0) | 16 | |
| IVb | 1 (0.3) | 1 (0.3) | 2 | |
| V | 0 (0.0) | 2 (0.6) | 2 | |
| Type of complicationa | ||||
| Infectious | 19 (5.4) | 14 (4.0) | 33 | .476 |
| Hemorrhagic | 6 (1.7) | 4 (1.1) | 10 | .752 |
| Respiratory | 2 (0.5) | 0 (0.0) | 2 | .499 |
| Cardiovascular | 4 (1.1) | 0 (0.0) | 4 | .124 |
| Nephro-urological | 2 (0.5) | 2 (0.5) | 4 | 1.000 |
| Other surgical | 6 (1.7) | 3 (0.8) | 9 | .505 |
| Other digestive | 2 (0.5) | 6 (1.7) | 8 | .286 |
| Consequence of the complication | ||||
| Readmission | 8 (2.2) | 8 (2.2) | 16 | 1.000 |
| ICU | 15 (4.2) | 21 (6.0) | 36 | .393 |
| Reoperation | 8 (2.2) | 9 (2.5) | 17 | 1.000 |
| Mortality | 0 (0.0) | 2 (0.5) | 2 | .499 |
The percentages are calculated from the total number of patients in each group.
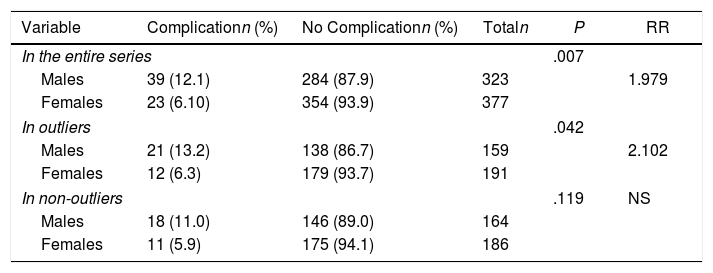
When we analyzed all the patients, we found that a higher percentage of complications appeared in men, with an RR of 1.979 (P=.007). When this analysis was performed separately, the same phenomenon occurred in OP (P=.042), with a significantly higher risk of complications in men (RR=2.102). However, in the non-OP group, there were no statistically significant differences in the percentage of complications between men and women (P=.19). All these data are shown in Table 4.
Complications According to Gender; Evaluation of Risks.
| Variable | Complicationn (%) | No Complicationn (%) | Totaln | P | RR |
|---|---|---|---|---|---|
| In the entire series | .007 | ||||
| Males | 39 (12.1) | 284 (87.9) | 323 | 1.979 | |
| Females | 23 (6.10) | 354 (93.9) | 377 | ||
| In outliers | .042 | ||||
| Males | 21 (13.2) | 138 (86.7) | 159 | 2.102 | |
| Females | 12 (6.3) | 179 (93.7) | 191 | ||
| In non-outliers | .119 | NS | |||
| Males | 18 (11.0) | 146 (89.0) | 164 | ||
| Females | 11 (5.9) | 175 (94.1) | 186 | ||
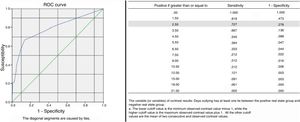
When we studied the correlation between the number of days as OP and the presence of complications by means of an ROC curve, statistical significance was reached, and the optimal cut-off point after which OP began to have complications was 2.5 or more days (Fig. 2).
Regarding the costs, we observed that there were no significant differences between the two groups (P=.573).
DiscussionOP rates can be a quality indicator of hospital bed management and, in a way, the rationality of a hospital's bed allocation is an efficiency indicator.17–19 Our OP rate was 12.45%. We have not found other articles that report this datum in the GDS setting. Goulding3 reported an OP rate of 5.65%, and the Cabrera Torres et al. study20 reached 8.4%. One reason to explain this difference may be that both excluded the summer period, while we included the entire year. In addition, they included patients from all specialties.
Alameda and Suárez21 argue that holidays and weekends may be risk factors to prolong hospitalization stay and delay diagnosis for OP. In fact, our data16 confirm that hospital stays and costs during vacation periods are higher than at other times of the year. However, when only the complications are compared, they are neither more expensive nor generate more hospital stays than during the rest of the year.
During the summer, some hospitalizations wings are usually closed for maintenance, regularization of activity, etc., and in the winter there is a peak demand for hospital beds due to worsening respiratory or heart disease because of bad weather,22 in addition to population aging, as Goulding indicates.3 Although we do not specifically focus on the frequency of OP admitted during vacation, we have observed that it does not significantly increase the number of OP in our specialty. This is probably due to the adequate management of the discharges in addition to the drop in scheduled surgical activity. Furthermore, greater prioritization is given to complex cases in vacation periods, thus decreasing those of less complexity, which are the biggest candidates for OP.
The complexity of this series was 1.59 in both groups due to the sampling method. Cabrera Torres et al.20 found a statistically significant difference in complexity between OP and non-OP. However, the complexity was greater in non-OP, who had better results in their case. The reason for the lower complexity in the OP may be due to the fact that, in case of increasing pressure in the ER, the admitting service gives priority to patients with greater requirements so that they are admitted to the wards of their specialty, while those requiring less demanding treatment are admitted to outlying rooms.
Most studies4,20,23 consider that OP have a greater risk of presenting adverse events due to their longer hospital stay,6 less training of non-specialized nursing staff,21 inadequate room conditions for the patient's disease,23 poor communication between the ward where the patient is admitted and the admitting doctors,5 etc. However, in our case, we found no statistically significant differences either for the complications or their consequences.
According to related articles, the impact of the quality of nursing care has been one of the most widely discussed factors. Elsayed et al.24 compared the care provided for compartment syndrome by nurses with and without orthopedic training. The results showed that nurses who had not received training were less prepared to care for orthopedic patients. Hommel et al.12 reported that OP with a hip fracture can have more complications during hospitalization. Both studies showed that moving to unspecialized wards increases risk. We believe that the reasons for their opinions are not confirmed in our research, probably because they treat a very specific ailment, with very specific care, while ours is more general, requiring standardized care that is not so specific. In addition, the fact that only 17 patients (4.9%) were treated in medical wards, while the remaining OP were treated in medical-surgical wards (114; 32.6%) or surgical wards (219; 62.6%) of a specialty other than GDS, greatly facilitates the fact that the care, although not overly specialized, was provided mostly by nurses with general surgical knowledge.
Likewise, there have been reports of longer hospital stays for OP6,12,20,21; however, in our study, we found no statistically significant differences. Several causes affect hospital stay, such as delays in rounds, delays in the processing of diagnostic tests, lack of pressure from doctors in other wards to discharge OP, etc. We believe that it is very necessary to have a physician responsible for OP management. Thus, their treatment would be a priority for this doctor, and the OP would not come second after the treatment of the non-OP has finished, thereby preventing delays in non-urgent complementary tests or hospital discharge. However, we have not entered into the analysis of this variable because of its difficulty in both measurement and recording associated with a retrospective study.
The initial idea that OP could have more complications and longer hospital stays seems to imply that the costs of these patients would also be higher. However, the actual costs, adjusted for the hospitalization use rate, vary between the two groups without reaching statistical significance. Therefore, we cannot confirm that OP are more expensive than non-OP. We believe that this is because of the few complications presented and low complexity.
We observed an interesting fact: among OP, there is a predominance of complications in men compared to women, with an RR=1.979. However, we have not found any reason to explain this. According to the study by Ambe and Köhler,25 being male could be an independent risk factor for presenting complications in patients undergoing laparoscopic cholecystectomy, with longer surgical times, longer hospital stays and a higher conversion rate at ages over 65, although these results cannot be extrapolated to our study.
By analyzing the ROC curve, we observed that when the outlying stay exceeded an average of 2.5 days, complications increased. We have not found any other studies that analyze this point and, therefore, we can establish an initial reference. We recommend trying to transfer the OP to the appropriate ward within 2.5 days in order to avoid the complications associated with outlying hospitalization. However, if the expected hospital stay will be less than 2.5 days, it does not make much sense to generate the transfer because of the unnecessary consumption of associated resources (time, cleaning, orderlies, etc.).
Because of its retrospective nature, the main limitation of this study lies in the bias created by the selection of outlying patients due to the dynamics of the admissions department. If a future prospective study were conducted, the option of randomizing the location of the patients, once their admission is decided, would probably resolve this question. Nonetheless, we feel that both the modification of hospital admission dynamics and the absence of beds in the hospital cases in which this occurred limited this design, which a priori was appropriate.
As a final conclusion, we propose that, in cases when outlying admissions are necessary, selecting less complex patients would not increase the complications or their consequences (ICU admissions, re-admissions, reoperations or mortality), hospital stays or costs. More complications seem to arise only in cases of prolonged outlying hospitalization of more than 2.5 days or in men. Therefore, OP men should be avoided in general, and patient transfer should be considered when a hospital stay beyond 2.5 days is foreseen.
Conflict of InterestsThe authors have no conflicts of interests to declare that could modify the results or conclusions.
Please cite this article as: Gomez-Rosado J-C, Li Y-H, Valdés-Hernández J, Oliva-Mompeán F, Capitán-Morales L-C. Análisis de la frecuencia, tipos de complicación y costes económicos en los pacientes ectópicos de cirugía general y digestiva. Cir Esp. 2019;97:282–288.