Streptococcus intermedius is a commensal bacterium. However, with the improved sensitivity of laboratory techniques, it has been identified as an important pathogenic germ in humans. It has been isolated in patients with periodontitis or with fatal purulent infections that metastasise to other organs.1
We present the first case of oral infection and involvement of the mammary gland in a healthy 60-year-old woman with poor dental hygiene. This case of invasive, rapidly developing empyema affecting the neck, chest wall and breast encouraged us to examine the need for systematic testing to identify the oral aetiology.
A 60-year-old woman was admitted to the emergency department due to fever that had progressed over the previous 3 weeks as well as a right infraclavicular mass, enlarged right mammary gland and pain that radiated towards the right arm and neck. The patient had experienced weight loss (of an unspecified amount) and had taken antipyretics (diclofenac and dexketoprofen), with good response.
At the time of hospitalisation, the patient presented syncope and haematemesis. That night, she was diagnosed with a peptic ulcer (probably related with the use of antipyretics during the previous weeks) and was treated endoscopically.
Blood work showed a leucocyte count of 21830×109/L and haemoglobin 114g/L.
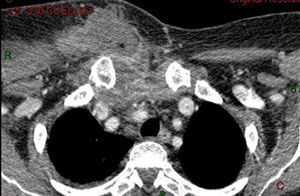
Once the ulcer had been treated, the patient continued to have fever and pain in the neck and right arm for the following 5 days, at which time a computed tomography (CT) study was ordered due to her deteriorating condition. The CT scan revealed multiple interconnected abscesses affecting the right side of the neck (Fig. 1) and the anterior chest wall, sternoclavicular joint, superior mediastinum and right breast (Fig. 2).
At this time, the patient had a leucocyte count of 16200×109/L and haemoglobin 85g/L.
Given these results, surgical intervention was indicated.
A multidisciplinary approach was used, and several contiguous abscesses were found going down the neck to the chest wall and right breast. Various incisions were made to drain the purulent content (Fig. 3). Integrity of the fascia was inspected, and the possibility of descending necrotising mediastinitis was ruled out.2
Five days after surgery, Streptococcus intermedius was isolated from the cultures. The administered empirical antibiotic treatment had already been effective.
Blood work levels had normalised and symptoms disappeared, so the patient was discharged 14 days after surgery.
To date, the patient remains asymptomatic, with the exception of her dental problems, which still have not been resolved.
Odontogenic infections (OI) originate in the teeth and periodontal tissue. Although OI are often localised and self-limiting, in certain rare cases these may spread and endanger the patient's life.
In the literature, many serious complications of OI have been described,3 including cavernous sinus thrombosis, Ludwig's angina, thoracic empyema, cerebral abscess,4 meningitis and septicaemia, maxillary sinusitis and osteomyelitis, mediastinitis, necrotising fasciitis, abscess causing airway compression,5 orbital abscess, carotid sheath abscess and jugular thrombophlebitis, pleurisy and other processes related with bacteraemia, toxaemia caused by pathogens and the induced autoimmune response.6
The few case reports of OI with abdominal involvement are normally related with bacteraemia derived from dental foci and include liver, suprarenal and retroperitoneal abscesses and even abscesses due to continuity along anatomic planes through the diaphragm.5
Until now, this is the first case report describing a breast infection originating in the oral cavity of a previously healthy patient.
There are 3 possible fascial pathways that can comprise a means for abscessification from the neck to the thorax: retropharyngeal and retro-oesophageal, perivascular, and pretracheal (the anatomic plane involved in our case).5 Furthermore, there are also other mechanisms, such as lymphatic or hematogenous dissemination, which have been described in the extension of Streptococcus intermedius.7 In any event, we cannot rule out the possibility that the abscess could have originated from an isolated implantation and later abscessification of isolated septic foci. The connection in a descending manner and the patient history of poor oral hygiene support the theory of a fascial mechanism instead of bacteraemia causing abscesses after an initial single focal origin.
The history of tooth pain, lack of dental hygiene and the isolation of Streptococcus intermedius indicate an oral origin. OI complications have a low incidence but should always be considered especially because, as in the case we report, the patient's life may be at risk. A multidisciplinary team is necessary to debride and drain the different abscesses in these cases. The mouth should be considered a possible origin in the differential diagnosis of fever of unknown aetiology, tumours and abscesses of the neck, thorax and breasts, even in previously healthy patients.
Please cite this article as: Segura-Sampedro JJ, Jiménez-Rodríguez R, Camacho-Marente V, Pareja-Ciuró F, Padillo-Ruiz J. Absceso mamario y sepsis con origen en infección oral. Cir Esp. 2016;94:308–309.