Abdominal wall involvement in colon cancer is a surgical challenge requiring extensive en bloc resection of all elements affected by the tumor. It is a rare complication of these tumors that requires proper planning and multidisciplinary assessment.
We present the case of a 76-year-old male with a history of stenosing sigmoid adenocarcinoma who presented an abdominal wall fistula on imaging tests (T4). An endoluminal stent was inserted as a bridge to surgery in order to facilitate the possibility of anastomosis. Subsequently, complete cytoreduction was performed with complete peritonectomy of the left iliac fossa and flank, dissection of the left gonadal vessels and vas deferens due to tumor involvement, appendectomy, cholecystectomy and complete omentectomy, as well as mitomycin C-based HIPEC as part of a trial for advanced colon tumors1.
During surgery, there was no evidence of peritoneal dissemination of the disease (PCI 0). Wall involvement was limited to contact with the internal inguinal orifice, where it trapped the left spermatic vessels and vas deferens. We resected the structures of the inguinal canal and the peritoneum of the left iliac fossa (including that of the left inguinal orifice).
Cytology of the peritoneal fluid was negative for malignant disease. The pathological study identified a moderately differentiated adenocarcinoma of the sigmoid measuring 9 × 8 cm with a stent perforating the colon wall, T4b, free resection margins, lymph node involvement 0/23. The excised peritoneum (20 × 6 cm) was free of tumor invasion. After surgery, the patient was administered adjuvant chemotherapy with capecitabine.
In the initial outpatient follow-up visits, no complications were observed. Six months after surgery, however, a left inguinal mass appeared with signs of inflammation. The mass was drained under local anesthesia, finding a purulent collection. Intravenous antibiotic therapy was administered to control the septic focus.
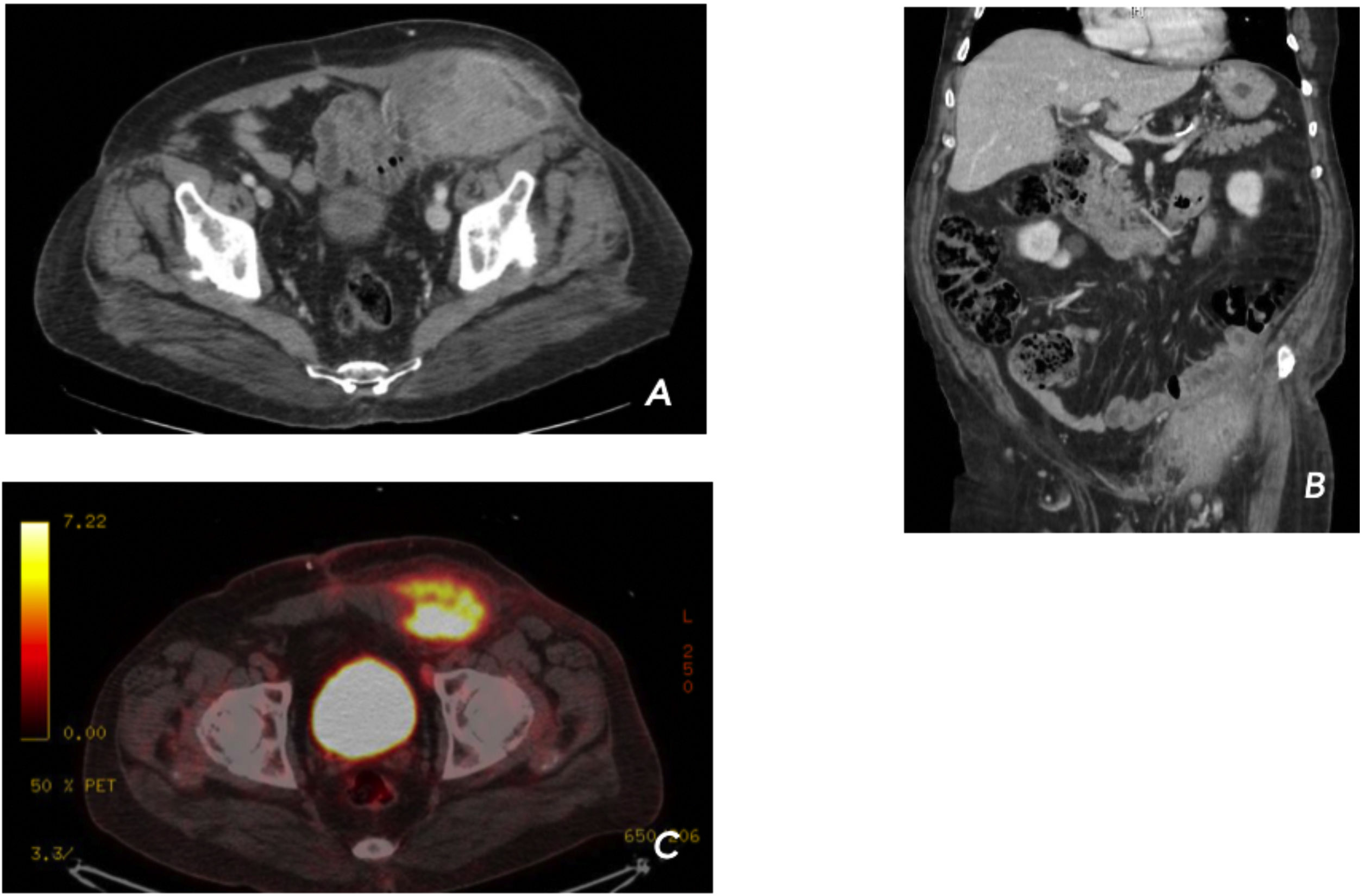
Abdominopelvic CT scan (Fig. 1) revealed a lesion associated with the left rectus abdominis muscle, coinciding with the area of the wall where the lesion initially fistulized. A PET/CT scan described increased metabolism of the inguinal tumor, compatible with neoplastic recurrence. Finally, FNA biopsy was taken from the lesion, which was positive for intestinal-type adenocarcinoma.
Given the results of the complementary tests and the recurrent infections that prevented the administration of neoadjuvant therapy, we decided to reoperate, remove the affected area, and completely reconstruct the area at the same time. We performed en bloc excision of the affected abdominal wall from the left anterosuperior iliac crest to the root of the penis, including the left external oblique, anterior rectus, and transverse muscles, resulting in a defect of about 40 × 50 cm.
Visceral resections included left orchiectomy, resection of a jejunal loop in contact with the mass, and mechanical side-to-side isoperistaltic anastomosis. The wall closure was performed with bicomponent mesh (Proceed® 40 × 40 cm) in a bridge-type repair, sutured to the aponeurosis of the rectus and oblique external muscles medially and to the anterior superior iliac spine laterally, making small perforations in the latter with a drill. Coverage of the skin defect was performed with a pedicled anterolateral thigh (ALT) flap, and the area from which the flap was harvested was covered with partial skin grafts (Fig. 2).
The pathological study of the piece identified an intestinal adenocarcinoma measuring 18 × 16 × 10 cm with an abscessed component at the cutaneous level, no involvement of the intestine or testicle, and free margins. The postoperative period was correct and complication-free. After 20 months of follow-up, the patient remains free of disease and only presents a moderate loss of function in the left lower extremity (34 points on the lower extremity functional scale, or LEFS).
For the staging of the wall defect, we used the Anderson abdominal wall reconstruction classification system for oncological pathology. According to this, the defect would be type I-II-IV (left mesogastric, hypogastric and abdominal wall) subtype C (involvement of the wall in its entire thickness)7.
Abdominal wall involvement in colon cancer occurs in approximately 7.5% of cases, requiring en bloc resections of the colon and affected areas, which entail multivisceral resections in up to 12%2–6.
When performing abdominal wall reconstruction due to oncological lesions, adequate planning is essential to fully recover the functionality of the structure while also ensuring complete resection. However, the extent of the disease at the time of surgery must also be considered. In the event that curative surgery cannot be performed, the indication of a large wall resection with reconstruction should be reconsidered when the expected benefit for the patient would be limited2–6.
During dissection, care should be taken to spare soft tissues and vessels to the greatest extent possible for proper subsequent anchoring of grafts or flaps. In patients with infraumbilical abdominal defects, like ours, the most recommended flap is the ALT type because of its mobilization capacity, as it can be used as a pedicle or free flap1,5,8,9.
Cytoreductive surgery and HIPEC associated with complex wall reconstructions provide for complete cytoreductions (CC-0) but also entail risks. According to the literature, the associated morbidity is 5%-35% and includes incisional hernias, dehiscence of the surgical wound and local infections.
To achieve optimal results in these patients, it is advisable to refer them to specialized medical centers with a greater volume of these pathologies as well as multidisciplinary management to provide optimal surgical treatment.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Gil-Catalán A, Segura-Sampedro JJ, Jerí-McFarlane S, Estrada-Cuxart J, Morales-Soriano R. Recidiva local de adenocarcinoma de sigma sobre pared abdominal. Resección oncológica y reconstrucción de pared compleja. Cir Esp. 2022;100:180–182.