Video-assisted thoracoscopy is a minimally invasive procedure that is routinely used for the resection of pulmonary nodules in pediatric surgery. However, its use may be limited in the case of small lesions (less than 1cm) or those located deep within the lung parenchyma with no pleural contact. Thoracoscopic instruments do not have the tactile sensation of a surgeon's hand, so preoperative marking of the lesion with radiologic techniques is necessary for proper resection.1,2
We present a case in which the combined use of radiological techniques and marking of the lesion with methylene blue provided direct visualization of a nodule, which resulted in successful resection with video-assisted thoracoscopy.
Case ReportThe patient was a 12-year-old boy with a history of right nephrectomy due to spindle cell sarcoma in 2007. In 2008, a spinal metastasis required arthrodesis of T9. A follow-up PET-CT in 2009 revealed a posterior-basal lesion with high uptake in the right lower lobe suggestive of pulmonary metastasis.
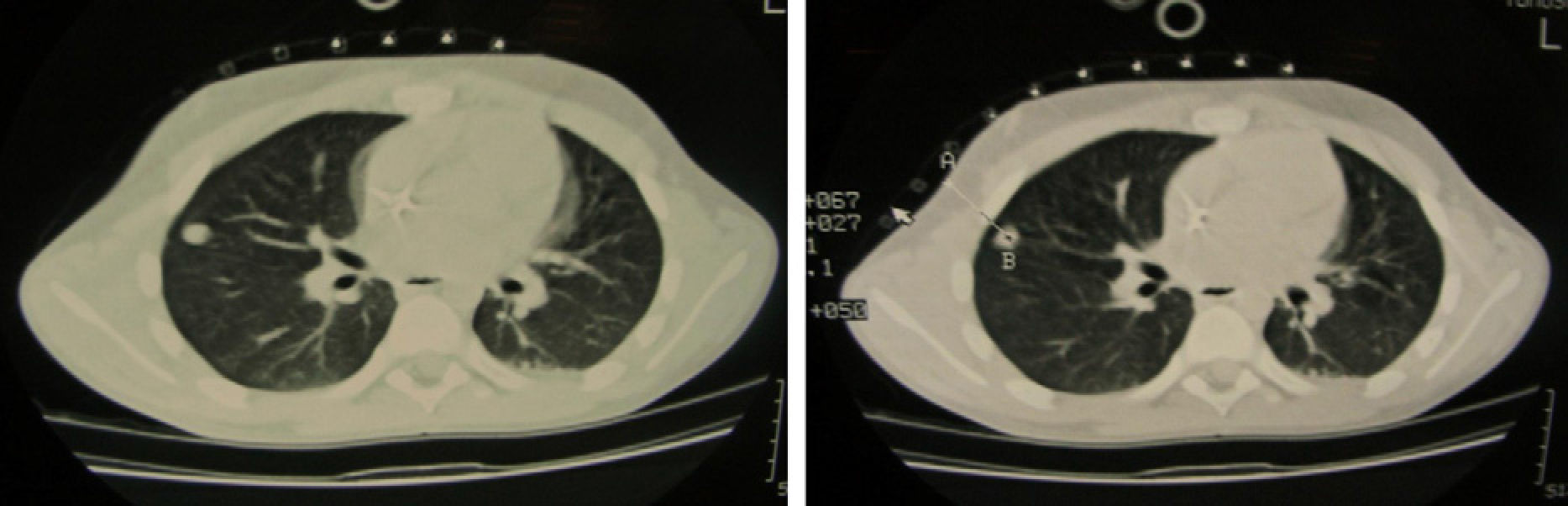
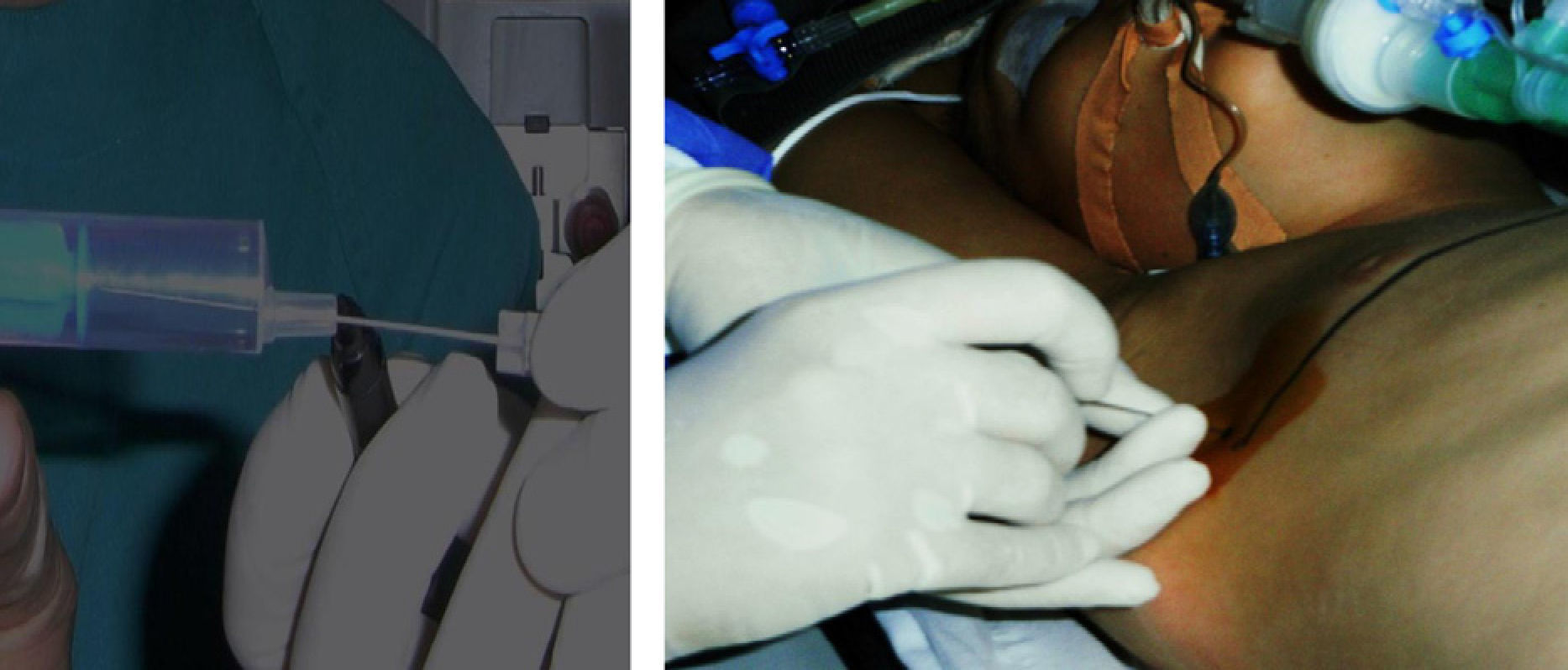
Due to its peripheral location and because it was not in close contact with the pleura (3mm deep), as well as its small diameter (7mm), we decided to mark the nodule using computer tomography (CT) guidance (Fig. 1). In the radiology room, under general anesthesia and using face masks, a needle puncture was performed through the 5th intercostal space, guided by CT, and methylene blue was injected (0.1ml) (Fig. 2).
Afterwards, the patient was transferred to the operating room to begin surgery as soon as possible in order to prevent the diffusion of the injected methylene blue. We proceeded with the selective intubation of the left main bronchus with a flexible bronchoscope, positioning the child in the left lateral decubitus position to start thoracoscopic resection. Three triangulated ports (two 5-mm and one 12-mm) were inserted and, with a 30° camera and ENDOGIA, a wedge measuring 3cm×3cm×3cm was resected, including the nodule with healthy margins. Direct visualization of the punctured area that had been stained blue allowed us to locate the nodule and remove it with safety margins. At the end of the operation, the CO2 was extracted and a chest tube was not required.
During the post-op period, pain was controlled with oral analgesia. Follow-up chest radiography showed no residual pneumothorax, and the patient was discharged 12h after surgery.
The pathology study of the surgical specimen revealed that it was a pulmonary metastasis of the renal spindle cell sarcoma.
ConclusionVideo-assisted thoracoscopic surgery (VATS) is currently the approach of choice for the resection of peripheral single lung nodules for both diagnostic and therapeutic purposes. The combined use of radiological techniques for marking small nodules with no pleural contact allows for adequate visualization of the area to resect, while resolving the limitations of thoracoscopic resection.3,4
The puncture is performed in the intercostal space, close to the upper edge of the rib to avoid injury to the intercostal nerve bundle. With CT guidance, the needle or harpoon is positioned in the exact area of the lesion and a small amount of methylene blue is injected. CT-guided tumor marking is a simple and safe procedure that can be performed in the radiology room, after which the patient is transferred to the operating room. It always requires general anesthesia, and its most common complication is pneumothorax.5,6 The main drawback of this technique is the fast, high rate of diffusion of methylene blue. It may be helpful to dilute it with autologous blood from the patient and inject the minimum amount required; the surgery should be performed immediately within the hour, if possible.7
The advantages of this minimally invasive surgery versus traditional thoracotomy are: less postoperative pain, better recovery of lung function, lower systemic inflammatory response, shorter hospital stay, better esthetic results and less thoracic deformity with the growth of the child. The difficulties and limitations of thoracoscopy can be resolved with the support of radiological localization and marking procedures of small, deep nodules.8–10
During the procedure, the radiologist, anesthetist and pediatric surgeon should work as a perfectly coordinated team.
Please cite this article as: Martínez Criado Y, Pérez Bertólez S, Cabello Laureano R, de Agustín Asensio JC. Instilación de azul de metileno guiado por tomografía axial computarizada para localizar y resecar mediante toracoscopia un nódulo pulmonar. Cir Esp. 2014;92:139–141.