Endovascular radiofrequency with first generation catheters was not successful due to its technical difficulty and restrictions in veins with diameters larger than 12mm. However, using the new catheter there is not enough scientific evidence to affirm that the diameter represents a technical limitation. The aim of this study was to evaluate and compare pre and post-operative venous trunks diameter, aiming at the reduction of size after 6 months with last generation catheters.
MethodsRetrospective observational and descriptive study on a cohort of patients with insufficiency of the great saphenous vein, small saphenous vein and anterior accessory vein operated on with last generation radiofrequency catheters. The diameters were evaluated in the pre and post-operative period with ultrasound.
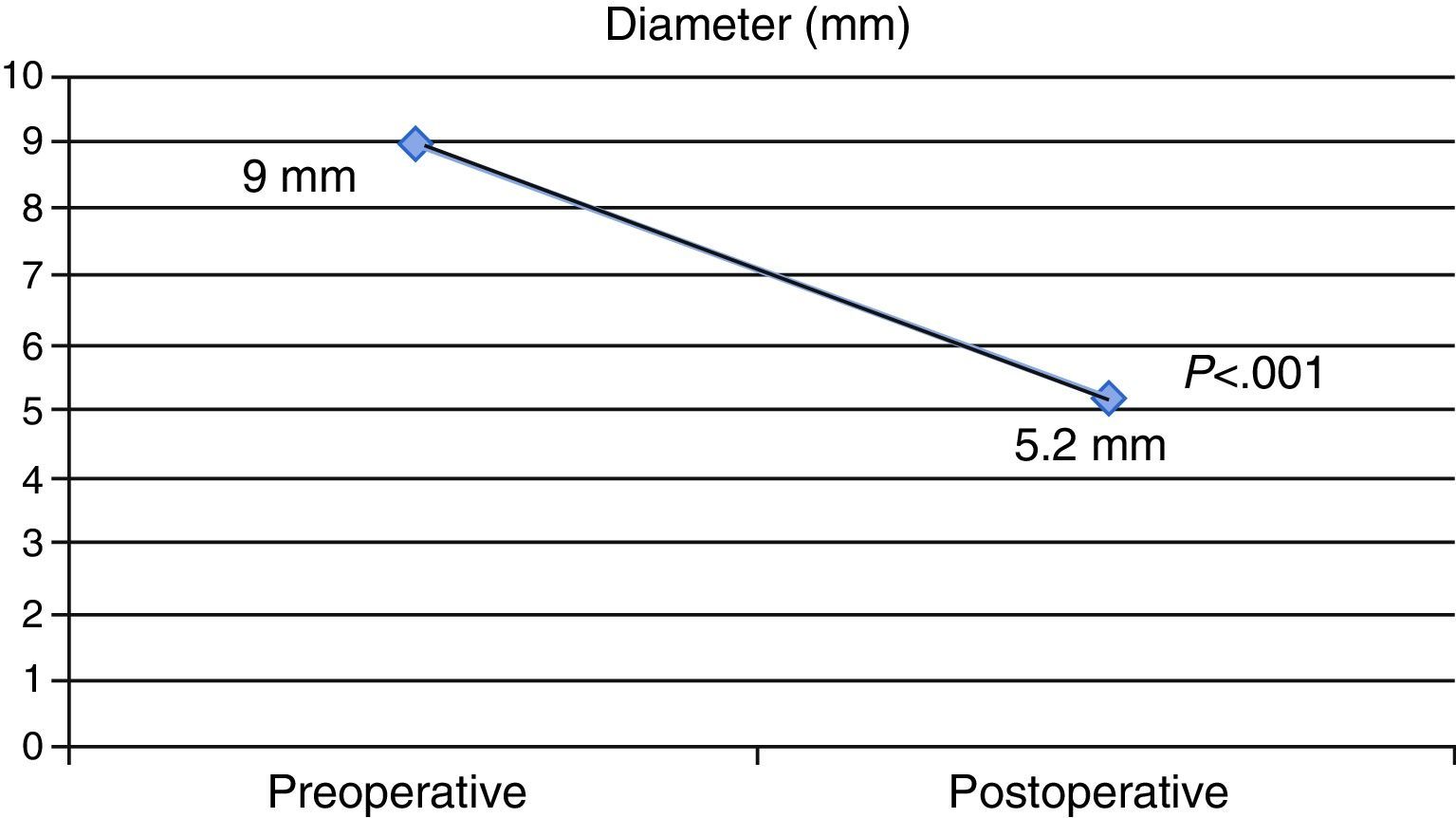
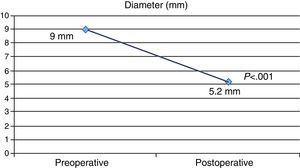
ResultsBetween 2007 and 2014 a total of 365 ablations were performed in veins with an average diameter of 9±3.1mm showing a reduction of it after 6 months with a mean value of 5.2±0.8mm (P<.0001). Total occlusion was also observed in 100% of cases and complications such as deep vein thrombosis in 0.5% and heat-induced thrombosis in 1.1%.
ConclusionsA significant reduction in venous diameter after endovascular treatment with the new ClosureFast® catheters was checked, even in veins with diameters greater than 12mm.
La radiofrecuencia endovascular con los catéteres de primera generación no obtuvo buenos resultados debido a su difícil manipulación y a las restricciones en venas con diámetros mayores de 12mm. Sin embargo, utilizando los nuevos catéteres no existe evidencia científica suficiente para afirmar que el diámetro represente una limitación técnica. El objetivo del presente estudio fue evaluar y comparar el diámetro pre y postoperatorio de grandes troncos venosos de miembros inferiores para determinar la reducción del caliber que se produce a los 6 meses de la ablación con catéteres de última generación.
MétodosEstudio retrospectivo observacional y descriptivo sobre una cohorte de pacientes con insuficiencia de la vena safena magna, vena safena parva y vena accesoria anterior de la safena magna, operados con catéteres de última generación de radiofrecuencia. Los diámetros fueron evaluados en el pre y en el postoperatorio mediante ecografía.
ResultadosEntre el año 2007 y el 2014 se realizaron un total de 365 ablaciones en vasos con un diámetro medio de 9±3,1mm, observándose una reducción de este a los 6 meses con un valor medio de 5,2±0,8mm (p<0,0001). Se observó además oclusión total en el 100% de los casos y complicaciones como trombosis venosa profunda en el 0,5% y trombosis inducida por calor en el 1,1%.
ConclusionesSe comprobó una significativa disminución del diámetro venoso tras el tratamiento endovascular con los nuevos catéteres ClosureFast® incluso en vasos con dilataciones superiores a 12mm.
Endovenous radiofrequency ablation (RFA) was the first procedure to use physical energy to treat large vessel insufficiency.1 At its inception in 1998 in Europe and after its approval by the US Food and Drug Administration (FDA) in 1999,2 the equipment included the first-generation catheters called ClosurePlus® and the generator RFAG Plus® (VNUS® Medical Technologies, San Jose, CA, USA).
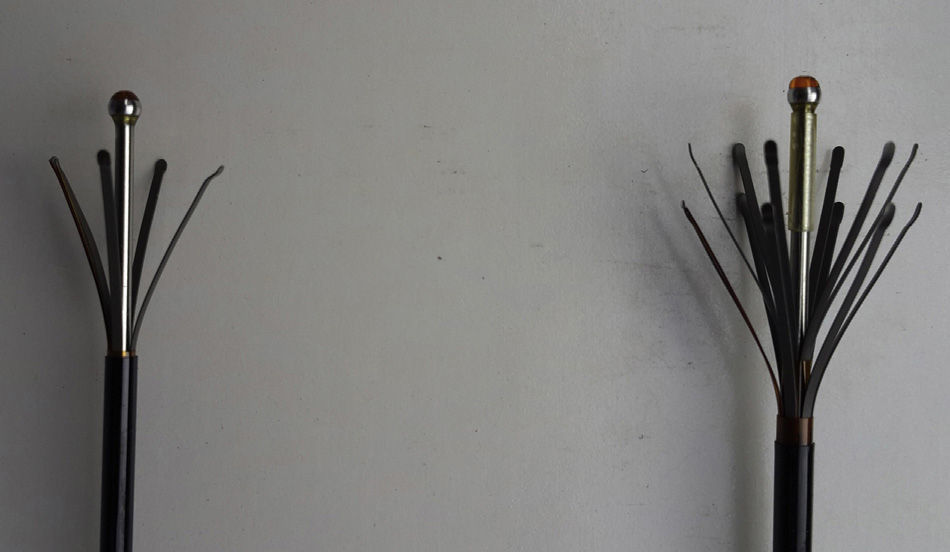
ClosurePlus® catheters were characterized by being complex to manage with a very slow pullback, which made the procedure very long. Furthermore, there were 2 catheter measurements (Fig. 1), 6 and 8F, for veins of up to 8 and 12mm in diameter, respectively,3 which was the maximum diameter treatable allowed by the FDA until that time.
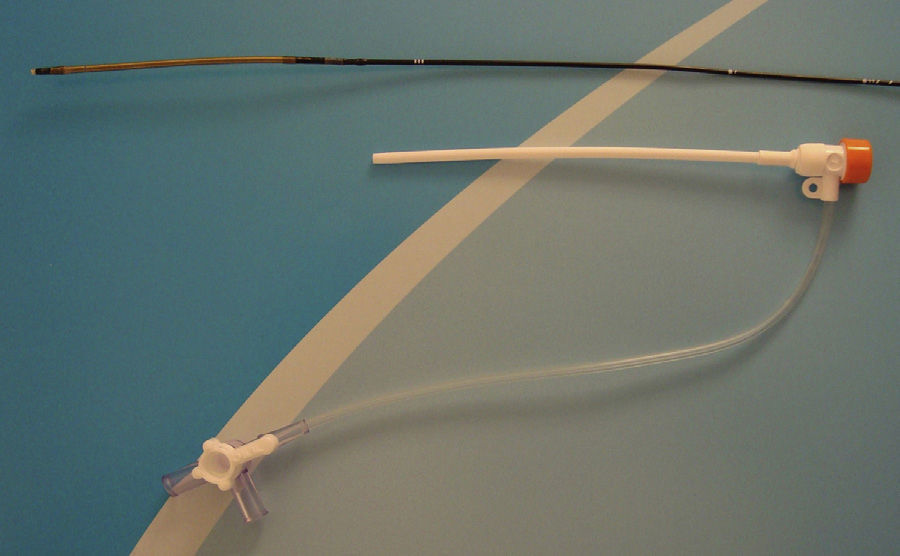
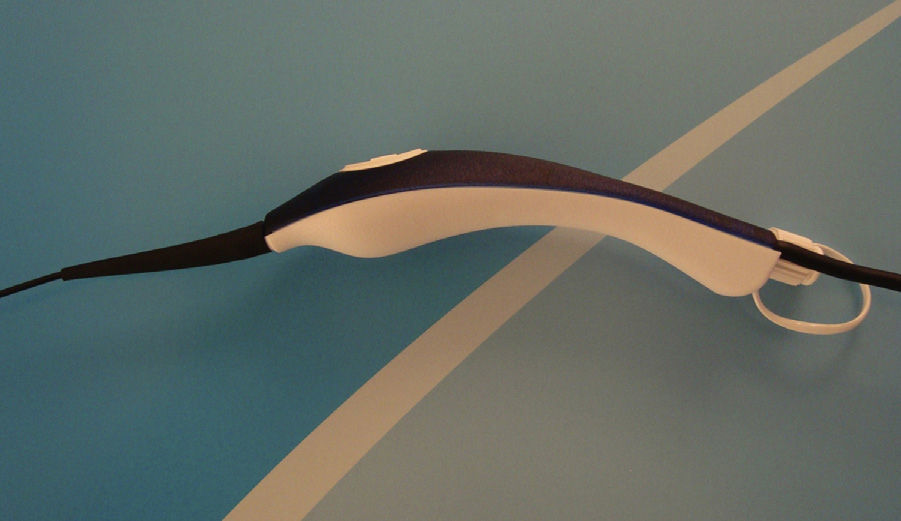
Given these limitations, in 2007 a new generation of catheters known as ClosureFast® was marketed by Medtronic (Minneapolis, Minnesota, USA). These devices have a heating coil element at their distal end measuring 7 or 3cm in length (Fig. 2) and markings along the length of the catheter every 6.5 or 2.5cm, respectively, providing for segmental ablation with an overlap of half a centimeter between segment and segment. The proximal segment has a sterile handle with a push-button (Fig. 3) to initiate or interrupt the emission of RFA manually. Each 20s cycle reaches a temperature of 120°C4 (registered by a thermocouple), and at the end of the cycle the generator interrupts the emission automatically.
Above 60°C, there is a rupture of the bonds of collagen triple-helix, thus increasing its contractile molecular strength.5 The temperature reached by the new ClosureFast® catheter is sufficient to induce endothelial destruction, denaturalization and collagen contraction in the venous wall, with shortening and reduction of the vessel lumen, plus an inflammatory reaction with posterior fibrosis, achieving venous occlusion. In this manner, with the introduction of this new catheter, large venous trunks with diameters larger than 12mm were able to be treated, although the treatment of these patients is still controversial. Furthermore, there is little evidence on the objective reduction of the diameter before and after treatment with these new catheters.
The objective of this present study is to evaluate and compare the pre- and postoperative diameters of the great saphenous vein (GSV), small saphenous vein (SSV) and anterior accessory saphenous vein (AASV) by observing their reduction in size, regardless of the initial measurement, 6 months after ablation with new-generation catheters. The secondary objective is to describe the presence of thromboembolic complications or endovenous heat-induced thrombosis (EHIT)6 within the first 72h post-op and to determine the rate of venous occlusion both one month and 6 months after ablation.
MethodsOurs is an observational and descriptive, retrospective study on a patient cohort with GSV, SSV and AASV insufficiency (based on symptoms and ultrasound studies) who were treated with RFA using ClosureFast® catheters between January 2007 and December 2014 in the Outpatient Surgery Unit at the Hospital Italiano of Buenos Aires.
All patients were operated on with the same surgical technique: 146 under general anesthesia, 127 under intravenous sedation, and 9 with local anesthesia alone. Venous access was performed with ultrasound-guided percutaneous puncture using Abbocath® 16G (Hospira Venisystem, Lake Forest, IL, USA) at the last reflux point, respecting approximately 15cm of the distal leg. After the catheter had been inserted, perivenous tumescent infiltration (saline solution, lidocaine, adrenalin and sodium bicarbonate) was administered by a peristaltic pump (Nouvag® DP20, Nouvag AG, Rorschach, Switzerland) through a 50/8 intramuscular needle, creating a distance of more than 1cm between the vein to be treated and the surrounding tissue to avoid thermal damage.
The protocol of use for the ClosureFast® catheter is well defined and standardized. Its tip should be positioned 2cm from the saphenofemoral junction, saphenopopliteal junction, or at the outlet of the GSV, depending on whether the vessel to treat is the GSV, SSV or AASV, respectively. Once the perivenous tumescence has been completed, at least two 20s cycles should be done in either the first segment or the segment that is most proximal to the deep venous system. Afterwards, one 20s cycle should be used in each of the remaining segments along the entire length of the vessel being treated.
The procedure is completed with phlebectomy of the dilated tributary veins, and the procedure is finished with a triple-layer bandage that is removed after 24h, which is later followed by an elastic stocking (20–30mmHg) or an elastic bandage for 5–7 days. Prophylaxis for thromboembolic disease is administered, specifically 40mg/day of low molecular weight heparin for one week in patients at risk (over the age of 50, use of oral contraception, smokers, those with a history of thromboembolic disease and/or a BMI over 30).
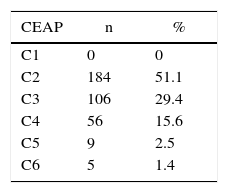
We collected demographic data and “C” component data from the CEAP clinical classification.7 The diameters of the GSV, SSV and AASV were evaluated in millimeters (mm) by means of ultrasound with the patient standing during pre-op, using as a measuring point the area that is 3cm distal to the saphenofemoral junction, saphenopopliteal junction or near the end of the GSV, depending on a GSV, SSV or AASV, respectively. The post-procedure diameter was evaluated by ultrasound at the same measuring point as the preoperative baseline measurement, with the patient standing and also expressed in mm, 6 months after endovascular ablation.
We also recorded whether deep vein thrombosis (DVT) and/or pulmonary embolism (PE) and EHIT were detected.
DVT is defined as the presence of a thrombus in any sector of the deep venous system (iliofemoral, femoropopliteal, tibioperoneal or soleal sinuses), evaluated clinically and by venous Doppler ultrasound 24–72h after the procedure. PE was defined as the impaction of a clot in any region of the pulmonary veins, evaluated by the clinical presentation of the patient during follow-up. EHIT was defined as the formation of a heat-induced thrombus, evaluated by venous Doppler 24–72h after the procedure. According to its location, this was classified into 4 grades: grade 1, the thrombus reaches the ostium of the junction of the ablated superficial system with the deep system, without overpassing it; grade 2, the thrombus surpasses the ostium, compromising less than 50% of the deep venous system; grade 3, the thrombus compromises more than 50% of the deep venous system; grade 4, the thrombus compromises the entire deep venous system.
The evaluation of the venous occlusion was determined by the percentage of veins without flow over the total of ablated veins in patients who had complied with follow-up, as evaluated by venous Doppler ultrasound in the first months and 6 months post-op. Occlusion was defined as the total absence of flow along the venous trunk treated.
Statistical AnalysisFor the descriptive analysis of the continuous variables, mean and standard deviation or median and range were used according to the distribution of the variable. Categorical variables were expressed in absolute frequency and proportion. To compare the pre- and post-treatment diameter, Student's t test for paired samples was used. Probabilities lower than 0.05 were considered statistically significant. The statistical analysis was calculated with Stata version 13.0 software (College Station, TX, USA).
Ethical ConsiderationsThe present study was conducted in complete accordance with the current national and international legal regulations: the Helsinki Declaration of the World Medical Association, Regulation 6677/10 of the National Administration for Medicine, Food and Medical Technology, the Rules for Proper Clinical Practices ICH E6m and the Personal Data Protection Law 25.326 (Habeas Law for data). All patients gave their signed consent for the procedure.
ResultsBetween January 2007 and December 2014, a total of 339 patients with clinical and ultrasound insufficiency of large blood vessels were treated with RFA, 57 of which (16.8%) did not complete the follow-up and were therefore excluded from this study.
Out of the 282 patients included, 203 were women (71.9%) and 79 were men (28.1%); mean age was 57±13 years. As for the C component of the CEAP classification, 184 patients (51.1%) were distributed as C2 and 106 patients (29.4%) as C3 (Table 1). A total of 365 segmental RFA ablations were done in 360 lower extremities, 305 of which were in the GSV, 51 in the SSV and 9 in the AASV. With regards to laterality, 168 cases involved the right lower limbs and 197 the left lower limbs; 78 presented bilateral involvement, and 5 patients had insufficiency of more than one venous trunk in one lower extremity, which were treated during the same surgical intervention. In all cases, the procedure was completed with phlebectomy of the dilated tributary veins with the Müller technique.
The preoperative venous diameter showed a mean of 9±3mm. Six months after ablation, the diameter showed a mean value of 5.2±0.8mm, which was a statistically significant difference (P<.0001) (Fig. 4). Meanwhile, the preoperative diameters of the treated veins had a range of 4–25mm, and the postoperative diameters were 2–11mm.
The Doppler ultrasound evaluation in the first 72h showed DVT of the soleal sinuses in only 2 cases (0.5%), one of which was asymptomatic; both were resolved with oral anticoagulant therapy during the first 6 months of evolution. In 4 cases (1.1%), we also observed the presence of grade 2 EHIT, all asymptomatic, which were treated for 15 days with low-molecular weight heparin; the treatment was completed in all cases within this time period, and none required hospitalization. Furthermore, no cases demonstrated symptoms of PE.
Doppler ultrasound evaluation one and 6 months after RFA ablation showed a percentage of venous occlusion of 100% in all the cases treated, even in those vessels with diameters greater than 12mm.
DiscussionEndovascular thermal ablation has been shown to be a safe and effective procedure recommended by the American Venous Forum and the Society for Vascular Surgery, with a degree of evidence of 1B according to the most recent clinical guidelines.8
Although the FDA did not recommend the use of first-generation ClosurePlus® catheters in veins with diameters larger than 12mm, with the appearance of the new generation ClosureFast® catheters there are already reports of their use to treat veins of up to 18mm in diameter.9
Our study demonstrates that the reduction in diameter 6 months after the procedure is statistically significant; the maximum treated diameter was 25mm, which had been reduced by 56% (11mm) 6 months after treatment.
It should be mentioned that, when administered correctly and favored by the pressure exerted by the peristaltic pump, ultrasound-guided perivenous tumescent infiltration contributes toward reducing the vein diameter10 to a bare minimum, whatever its caliber. This provides for better contact of the vascular endothelium with the thermal emission element, which in turn favors better action of the RFA on the vein wall.
As for thromboembolic complications, we can affirm that the results obtained in the present study are similar or lower to those currently found in the international literature. For example, while Marsh et al. reported post-RT DVT rates of 0.7%,11 in our retrospective analysis we have found a DVT incidence of 0.5%. Furthermore, although there are studies such as the Rosales-Velderrain et al. article that report a very low incidence of PE (0.03%),12 in our review we have found no complications of this type. Regarding EHIT, in our series we observed the presence of heat-induced thrombosis in only 4 cases (0.9%), all of which were Kabnik classification grade 2; meanwhile, recent studies such as that by Sufian et al. report an overall incidence of EHIT of 2.99%13 in a series of 6707 large venous trunks treated by RFA.
Last of all, the occlusion rates of the present report are 100%, both in the first month as well as 6 months post-segmental RFA ablation. These values are similar to those found by Proebstle et al. in the presentation of their first study about this subject, with results after one year of follow-up.14
It should be mentioned that the limitation of this paper is that it is a retrospective and observational study.
We can conclude that endovenous radiofrequency ablation is a safe and effective procedure. With the new ClosureFast® catheters, a significant reduction in post-ablation vein diameters is reached, including those veins with diameters greater than 12mm, which is the maximum measurement recommended by the US FDA. Nevertheless, this does not represent an impossibility or contraindication and it avoids the need for open ligation, with an observed optimal occlusion rate and no major complications.
AuthorshipHBM helped in study design. HBM, MD, RK, CMF, SR, CP contributed in data collection. HBM, HM helped in analysis and interpretation of the results. HBM contributed in composition of the article. HBM, MD, RK, CMF, SR, CP, HM helped in critical review and approval of the final version.
Conflict of InterestsThe authors have no conflicts of interests regarding the research, authorship or publication of this study.
The authors would like to thank Dr. Victoria Ardiles for her time and dedication toward the statistical evaluation of this study.
Please cite this article as: Bauzá Moreno H, Dotta M, Katsini R, Marquez Fosser C, Rochet S, Pared C, et al. Ablación endovascular por radiofrecuencia. Efecto sobre el diámetro venoso con el uso del catéter ClosureFast®. Cir Esp. 2016;94:353–357.