We prospectively evaluated health-related quality of life (HRQoL) through the gastrointestinal quality of life index (GIQLI) as a system to prioritize patients on the waiting list for laparoscopic cholecystectomy (LC) and its correlation with a linear prioritization system developed in the General and Gastrointestinal Surgery Institute of Clínica Quirón in Valencia.
Materials and methodsThere were 100 consecutive patients who underwent elective outpatient LC.
The main outcome measures consisted of: (1) assessment of the impact of the disease, measured through the GIQLI; (2) evaluation of an objective system based on technical scientific criteria; (3) evaluation of the utility of LC in improving HRQoL through the GIQLI by analyzing expected and obtained utility through the change ratio; and (4) analysis of the correlation between the objective linear system, HRQoL and utility.
ResultsThe GIQLI was useful in evaluating the impact of the disease. LC significantly improved HRQoL in both oligosymptomatic and symptomatic patients. The objective or clinical factors did not allow perceptions of the process to be evaluated or the impact on HRQoL to be measured or inferred. A prioritization system based on GIQLI scores allows patients to be selected according to the expected utility (worsening of HRQoL) and obtained utility (improvement in HRQoL) of CL.
ConclusionsPrioritization systems should include utility to guarantee equity. The GIQLI shows the impact of the disease on the patient while the clinical/objective factors are unrelated to the expectation of prioritization. Prioritization systems should include both elements to maintain the balance between impact and appropriate indication.
Evaluación prospectiva de la calidad de vida relacionada con la salud (CVRS) mediante el gastrointestinal quality of life index (GIQLI) como sistema de priorización de pacientes en lista de espera para el proceso colecistectomía laparoscópica (CL) y su correlación con un sistema lineal de priorización (SP) desarrollado en el Instituto de Cirugía General y Aparato Digestivo (ICAD) de la Clínica Quirón de Valencia.
Material y métodosUn total de 100 pacientes consecutivos a los que se les realizó CL electiva ambulatoria.
Principales medidas de resultados (1) repercusión de la enfermedad mediante el GIQLI; (2) evaluación de un sistema objetivo basado en criterios científico-técnicos; (3) evaluación del valor de la CL en términos de CVRS mediante el GIQLI analizando la utilidad esperable y la obtenida en términos de change ratio (CR) y (4) análisis de la correlación entre el sistema objetivo lineal, la CVRS y la utilidad.
ResultadosEl GIQLI es útil en la evaluación de la repercusión. La CL obtiene un beneficio en CVRS significativo en pacientes tanto oligosintomáticos como sintomáticos. Los factores objetivos o clínicos no permiten evaluar la percepción sobre el proceso ni medir o inferir la repercusión en CVRS. Un SP basado en tramos de puntuación del GIQLI permite una selección en función de la utilidad de la CL esperable (deterioro en CVRS) y obtenida (ganancia en CVRS).
ConclusionesUn SP debe incluir la utilidad para garantizar la equidad. El GIQLI objetiva la repercusión sobre el paciente mientras que los factores clínicos-objetivos no tienen relación con las expectativas de priorización. Un SP debe incluir ambos a fin de mantener el equilibrio repercusión/adecuada indicación.
The waiting lists for elective surgery are one of the biggest problems facing our healthcare system.1,2 Although they are necessary for resource management and scheduling, waiting lists are not justifiable when they become excessively long and do not give priority to patients in whom surgery would improve quality of life, even though the benefit of the intervention is supposedly marginal because it does not influence survival. Such is the case of patients with cholelithiasis.
The objective impact of gallstones can be estimated with the use of clinical classifications (McSherry Classification),3,4 frequency of symptoms, complications observed on ultrasound and work-ups, intraoperative findings and difficulties in performing surgery due to chronic inflammatory repercussions. Nonetheless, it is very difficult to correlate the clinical-objective impact with the vision that the patient has of his/her disease and, therefore, the timeframe in which the patient wants to be treated and considers reasonable. This explains why most prioritization systems in general surgery have failed as they are based on clinical and radiological classifications as well as the consensus of experts2 (adequacy or inadequacy) and do not consider patients’ perception of their disease.
The perception of disease is measured with health-related quality of life scales (HRQoL), which are multidimensional parameters that associate subjective and objective variables in order to determine physical, psychological and social state as well as overall satisfaction. The objective of this study is to contemplate the incorporation of HRQoL scales in the process of cholelithiasis treatment using the gastrointestinal quality of life index (GIQLI),5 a reliable and valid tool in the determination of HRQoL in patients undergoing cholecystectomy.
Materials and MethodsThis is a prospective, longitudinal cohort study that analyzed the GIQLI in a population of 100 consecutive patients who underwent elective outpatient laparoscopic cholecystectomy (LC). The patients had a previous history of complicated biliary disease, and the GIQLI was applied at 2 sequential points in time: during the preoperative period (upon being added to the waiting list) and 3 months after the intervention. The maximum time transpired from inclusion until surgery was 2 months and the maximum wait from the diagnosis of gallstones was less than 3.5 months.
In addition to the GIQLI, a questionnaire was included about: current ability to work, whether the patient carried out daily activities independently, associated symptoms of anxiety-depression (Hamilton scale), need for treatment (anxiolytic, hypnotic or depressive, analgesia for abdominal pain), need for emergency medical assistance either at home or at the hospital due to the disease, and other associated gastrointestinal symptoms not included in the traditional GIQLI in order to estimate the degree of impact by areas.
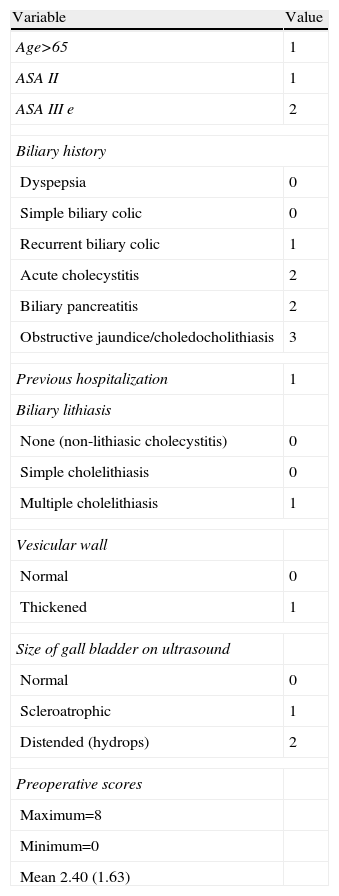
We created an objective preoperative prediction system (Table 1) with clinical and ultrasound data related to the duration of the process, severity or objective clinical intensity,3,4,6–8 as well as the estimated probability of recurrence/complications with the intention to obtain a linear scoring system based on objective, professional or scientific-technical criteria that would correlate with the HRQoL.
Preoperative Linear Scoring System.
| Variable | Value |
| Age>65 | 1 |
| ASA II | 1 |
| ASA III e | 2 |
| Biliary history | |
| Dyspepsia | 0 |
| Simple biliary colic | 0 |
| Recurrent biliary colic | 1 |
| Acute cholecystitis | 2 |
| Biliary pancreatitis | 2 |
| Obstructive jaundice/choledocholithiasis | 3 |
| Previous hospitalization | 1 |
| Biliary lithiasis | |
| None (non-lithiasic cholecystitis) | 0 |
| Simple cholelithiasis | 0 |
| Multiple cholelithiasis | 1 |
| Vesicular wall | |
| Normal | 0 |
| Thickened | 1 |
| Size of gall bladder on ultrasound | |
| Normal | 0 |
| Scleroatrophic | 1 |
| Distended (hydrops) | 2 |
| Preoperative scores | |
| Maximum=8 | |
| Minimum=0 | |
| Mean 2.40 (1.63) | |
All patients were treated by outpatient LC,9 and patients with early or delayed postoperative complications or those requiring conversion were excluded from the study.
The data were included in a database (Dbase 5) and processed with SPSS version 11. The relevant clinical, social and work-related variables were dichotomized in order to analyze any variations in the GIQLI. The psychological variables were analyzed individually in order to study the functional aspects of the patients. Related questions were grouped in “impact areas” in order to be able to individually assess disease severity in all the considerable spheres for each patient.
We used general estimation equations to compare the longitudinal changes in the GIQLI scores, both at baseline as well as 3 months after the LC, in order to calculate the sensitivity of GIQLI since it follows a normal distribution.10 The sensitivity was calculated by determining the change ratio (CR) derived from the coefficient between the mean change score (basal–3 months) and main baseline score multiplied by 100.11
The expected (potential) utility of the therapeutic intervention was defined as the difference between the reference GIQLI of the healthy population and the baseline GIQLI. The objective utility was calculated by using the difference between the post-op and baseline GIQLI and was expressed both in absolute units as well as in percent increase in HRQoL vs baseline scores, this being the CR.
A clinically relevant result was defined as an increase ≥10% over the baseline score12; relevant clinical utility (CU) was considered an increase in 20 absolute units over the baseline score.
The maximum GIQLI on the international score is 144, and the lowest score is 0, obtaining results of 121 (15.0) in healthy control subjects (mean age 48, range 18–74) and 125.8 (13.0) in 168 cases analyzed, respectively.13
The results of the GIQLI are expressed as means (standard deviation) and were compared with the paired student's t test; a P<.05 was considered statistically significant. The CR values are expressed as percentages.
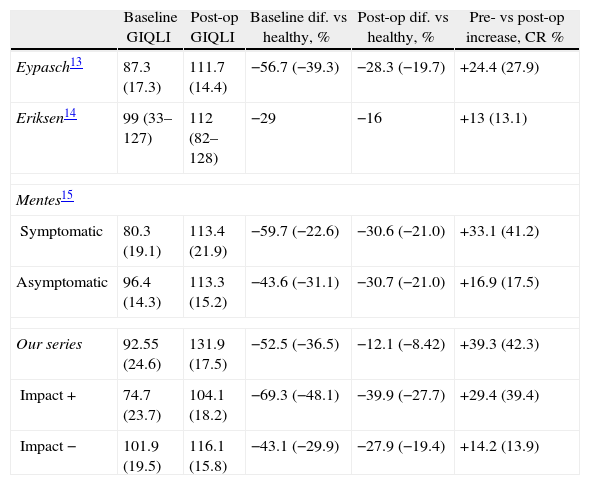
ResultsTable 2 shows the values obtained in our series, the absolute and percentage increase and the CR compared with other series13–15 in order to compare and validate the results obtained in our patient group. The decrease compared with healthy patients (maximum value), or percentage of expected utility, in the preoperative score are similar in all the series, varying according to the “objective” impact of the disease and symptomatic or asymptomatic patients, which validates both the quantitative and percentage results of our series.
Validation of the GIQLI With Regard to Previous Laparoscopic Cholecystectomy Series Based on the Calculation of Percentage Improvements in the Quality of Life Expressed.
| Baseline GIQLI | Post-op GIQLI | Baseline dif. vs healthy, % | Post-op dif. vs healthy, % | Pre- vs post-op increase, CR % | |
| Eypasch13 | 87.3 (17.3) | 111.7 (14.4) | −56.7 (−39.3) | −28.3 (−19.7) | +24.4 (27.9) |
| Eriksen14 | 99 (33–127) | 112 (82–128) | −29 | −16 | +13 (13.1) |
| Mentes15 | |||||
| Symptomatic | 80.3 (19.1) | 113.4 (21.9) | −59.7 (−22.6) | −30.6 (−21.0) | +33.1 (41.2) |
| Asymptomatic | 96.4 (14.3) | 113.3 (15.2) | −43.6 (−31.1) | −30.7 (−21.0) | +16.9 (17.5) |
| Our series | 92.55 (24.6) | 131.9 (17.5) | −52.5 (−36.5) | −12.1 (−8.42) | +39.3 (42.3) |
| Impact + | 74.7 (23.7) | 104.1 (18.2) | −69.3 (−48.1) | −39.9 (−27.7) | +29.4 (39.4) |
| Impact − | 101.9 (19.5) | 116.1 (15.8) | −43.1 (−29.9) | −27.9 (−19.4) | +14.2 (13.9) |
Baseline, pre-operative GIQLI score; CR %, change ratio; Baseline dif. vs healthy, preoperative GIQLI – GIQLI of healthy patients (expected utility); Post-op dif. vs healthy, postoperative GIQLI – GIQLI of healthy patients (utility obtained); Pre- vs post-op increase, absolute value and (percentage); Post-op., postoperative GIQLI score.
The number of patients with oligosymptomatic gallstones was 16/99 (16.2%), with symptomatic gallstones was 83/99 (83.8%) and with complicated cholelithiasis that required prior hospitalization was 9/99 (9.1%). Sixteen patients in the series needed emergency home assistance or emergency hospitalization between the time of diagnosis and inclusion.
The distribution of the series by type of occupation showed a high percentage of patients who were not actively employed (66 homemakers, 28 retirees and 16 unemployed) of 76 cases vs only 21 actively working patients, 14 of whom were civil servants and 7 contracted workers.
Age did not show differences in the pre- and postoperative GIQLI. In patients >65 years of age (No.=29), the preoperative GIQLI was 91.2 (23.2) compared with 91.6 (27.2) in the patients younger than the age of 65 (No.=70). The postoperative score also did not show differences between the 2 age groups: 105.6 (19.1) vs 112.2 (17.9), respectively. The absolute utility and the CR in the patients over the age of 65 were 14.4 (15.8%), respectively, compared with 20.6 (22.5%) in patients younger than 65.
The distribution by sex did show significant difference, although the proportion of males was sensibly lower (11.3% of the series). The pre-operative GIQLI was 106.6 (17.8) in men compared with 89.6 (26.3) in women (P=.012) and the postoperative values were 118.9 (11.4) in males vs 109.3 (18.8); P=.029. The absolute utility and CR were 12.3 (115%) in men compared with 19.7 (22.1%) in women.
In terms of the utility obtained (increment of 10% in GIQLI14) there were no significant differences in: age over 65 years vs under 65 (40.7 vs 45.7%), asymptomatic vs symptomatic cholelithiasis (57.1 vs 44.4%), and a history of previous hospitalization due to complicated cholelithiasis (57.1 vs 43.3%). There was, however, a significant difference between the sexes: 27.2% men vs 46.6% women.
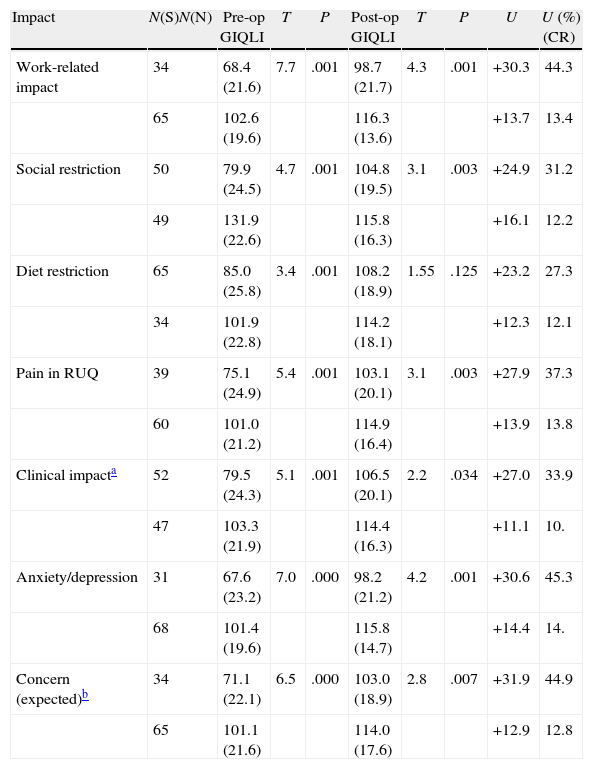
Table 3 shows the variations in the GIQLI, the absolute utility obtained (difference between baseline and post-op GIQLI) and the utility obtained (percentage of CR) depending on the different areas of impact analyzed, demonstrating significant differences in the areas of objective and subjective impact. The prevalence of anxiety-depression symptoms was very high (31/69), as well as the need for hypnotic, anxiolytic or antidepressant medication (42/73), generating very high expected utilities (25%).
Impact Areas and GIQLI.
| Impact | N(S)N(N) | Pre-op GIQLI | T | P | Post-op GIQLI | T | P | U | U (%) (CR) |
| Work-related impact | 34 | 68.4 (21.6) | 7.7 | .001 | 98.7 (21.7) | 4.3 | .001 | +30.3 | 44.3 |
| 65 | 102.6 (19.6) | 116.3 (13.6) | +13.7 | 13.4 | |||||
| Social restriction | 50 | 79.9 (24.5) | 4.7 | .001 | 104.8 (19.5) | 3.1 | .003 | +24.9 | 31.2 |
| 49 | 131.9 (22.6) | 115.8 (16.3) | +16.1 | 12.2 | |||||
| Diet restriction | 65 | 85.0 (25.8) | 3.4 | .001 | 108.2 (18.9) | 1.55 | .125 | +23.2 | 27.3 |
| 34 | 101.9 (22.8) | 114.2 (18.1) | +12.3 | 12.1 | |||||
| Pain in RUQ | 39 | 75.1 (24.9) | 5.4 | .001 | 103.1 (20.1) | 3.1 | .003 | +27.9 | 37.3 |
| 60 | 101.0 (21.2) | 114.9 (16.4) | +13.9 | 13.8 | |||||
| Clinical impacta | 52 | 79.5 (24.3) | 5.1 | .001 | 106.5 (20.1) | 2.2 | .034 | +27.0 | 33.9 |
| 47 | 103.3 (21.9) | 114.4 (16.3) | +11.1 | 10. | |||||
| Anxiety/depression | 31 | 67.6 (23.2) | 7.0 | .000 | 98.2 (21.2) | 4.2 | .001 | +30.6 | 45.3 |
| 68 | 101.4 (19.6) | 115.8 (14.7) | +14.4 | 14. | |||||
| Concern (expected)b | 34 | 71.1 (22.1) | 6.5 | .000 | 103.0 (18.9) | 2.8 | .007 | +31.9 | 44.9 |
| 65 | 101.1 (21.6) | 114.0 (17.6) | +12.9 | 12.8 |
RUQ, right upper quadrant pain; N(N), no impact; N(S), presence of impact; U, clinical impact in absolute value (mean increase in GIQLI pre- vs post-GIQLI score); U (%) (CR), percentage utility; Percentage increase over baseline GIQLI.
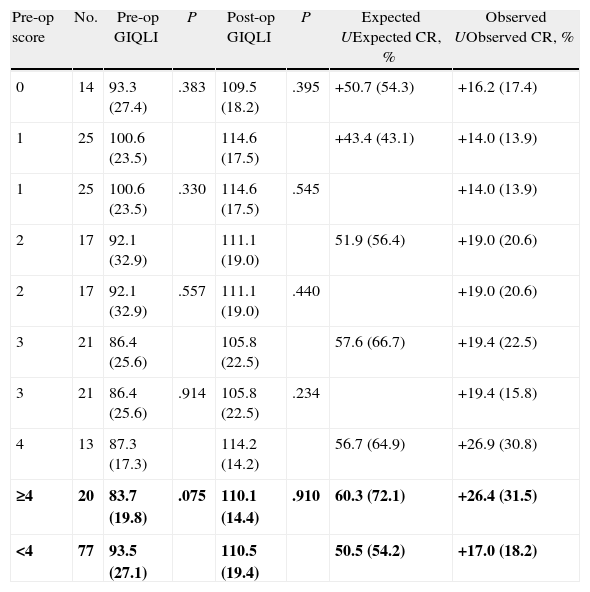
Table 4 shows the correlation between the different values of the objective linear scoring system and the HRQoL, absolute expected utility, expected CR, utility observed and CR obtained. The scores on the objective linear system do not show differences in the pre- and postoperative GIQLI. A discrete correlation was seen between expected and observed utility (CR), except for values of the linear dichotomized system with a cut-off value of 4, although the improvement in HRQoL is similar in patients with high “objective” prioritization (scores≥4) and low prioritization (score<4).
Correlation Between Preoperative Linear System Score and Quality of Life Expressed.
| Pre-op score | No. | Pre-op GIQLI | P | Post-op GIQLI | P | Expected UExpected CR, % | Observed UObserved CR, % |
| 0 | 14 | 93.3 (27.4) | .383 | 109.5 (18.2) | .395 | +50.7 (54.3) | +16.2 (17.4) |
| 1 | 25 | 100.6 (23.5) | 114.6 (17.5) | +43.4 (43.1) | +14.0 (13.9) | ||
| 1 | 25 | 100.6 (23.5) | .330 | 114.6 (17.5) | .545 | +14.0 (13.9) | |
| 2 | 17 | 92.1 (32.9) | 111.1 (19.0) | 51.9 (56.4) | +19.0 (20.6) | ||
| 2 | 17 | 92.1 (32.9) | .557 | 111.1 (19.0) | .440 | +19.0 (20.6) | |
| 3 | 21 | 86.4 (25.6) | 105.8 (22.5) | 57.6 (66.7) | +19.4 (22.5) | ||
| 3 | 21 | 86.4 (25.6) | .914 | 105.8 (22.5) | .234 | +19.4 (15.8) | |
| 4 | 13 | 87.3 (17.3) | 114.2 (14.2) | 56.7 (64.9) | +26.9 (30.8) | ||
| ≥4 | 20 | 83.7 (19.8) | .075 | 110.1 (14.4) | .910 | 60.3 (72.1) | +26.4 (31.5) |
| <4 | 77 | 93.5 (27.1) | 110.5 (19.4) | 50.5 (54.2) | +17.0 (18.2) |
Pre-op score, score on the pre-operative linear system of prioritization; Expected U, expected increase in QoL=healthy GIQLI – pre-op GIQLI; expected CR, expected percentage of utility; Observed U, observed utility (post/pre GIQLI); U % (CR), change ratio: percentage of utility.
In bold, analysis of the cut-off value; the remainder is the ordinal analysis.
The pre-operative values of the objective linear system generate excessive expected utility and, therefore, more false positives (meaning patients prioritized with marginal benefit from the therapeutic intervention) as high-priority patients. Moreover, these cut-off values generate a high percentage of false negatives (patients who are not prioritized even though they should be according to the utility obtained). Thus, the objective linear scale does not correlate with the impact of the disease estimated by the HRQoL or with either the expected or obtained utility.
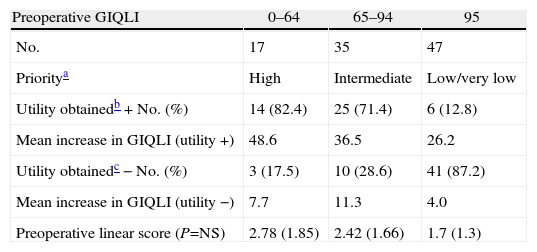
A division was made by arbitrary cut-off values, considering 3 levels of priority according to the pre-operative GIQLI score (estimation of the degree of pre-operative QoL deterioration or expected clinical utility) and the clinically relevant utility (increase in QoL≥20) (Table 5) in which evidence is given that the utility in the high, intermediate and low levels of priority were 82.4, 71.4 and 12.8%, respectively, with a low percentage of false positives (17.5, 28.6 and 12.8). The mean values of the objective linear system derived from the GIQLI scale scores for prioritization do not show statistical differences. They do show, however, considerable overlapping between the values, which confirms the lack of correlation between the objective linear system and utility in absolute terms and in observed CR.
Prioritization Scale According to the Giqli, Utility of the Therapeutic Intervention and Preoperative Objective Linear System.
| Preoperative GIQLI | 0–64 | 65–94 | 95 |
| No. | 17 | 35 | 47 |
| Prioritya | High | Intermediate | Low/very low |
| Utility obtainedb+No. (%) | 14 (82.4) | 25 (71.4) | 6 (12.8) |
| Mean increase in GIQLI (utility +) | 48.6 | 36.5 | 26.2 |
| Utility obtainedc−No. (%) | 3 (17.5) | 10 (28.6) | 41 (87.2) |
| Mean increase in GIQLI (utility −) | 7.7 | 11.3 | 4.0 |
| Preoperative linear score (P=NS) | 2.78 (1.85) | 2.42 (1.66) | 1.7 (1.3) |
Surgical waiting lists and their management continue to be a challenge16 for health-care institutions and the directors of hospital units. Lists longer than 6 months result in approximately 25% of cancelations17 due to clinical, legal, socio-family and work-related factors.
The heterogeneity of waiting lists is secondary to the variability of the clinical indication among specialists (even surgeons from the same unit), generating different uses for the therapeutic intervention, as also happens in the indication for remitting patients by gastroenterologists and general physicians. This generates underutilization or excessive indication of surgery, negatively affecting health-care quality and producing inadequate management of waiting lists.18
The adequacy of indications for a procedure19 has led to the development of methods such as the RAND (combination of experts and scientific evidence), which aims to provide directors and clinicians with information to help them determine the appropriateness of a procedure individually.20
Avoiding variability and adjusting the appropriateness for patients (tolerance to wait) and clinicians requires knowing the natural history of the disease, as it orientates the clinician (priority and adequacy) and eliminates the anxiety in patients caused by the uncertainty of the wait, by rationally adjusting the waiting period to the patients’ clinical category. In cholelithiasis, the delay between the diagnosis and intervention is associated with an increase in the development of complications of 1.6, 5.2, 11.5 and 23.7% for a wait list time of 1, 3, 6 and 12 months, respectively. This is even greater in acute cholecystitis, from 28.5% to 58% at 12 months, with 50% of readmittances within 6 weeks4,6,7 vs only 18% in simple hepatic colic.
Oligo- or asymptomatic gallstones become symptomatic in between 1% and 4% and in up to 20% annually after 20 years21 with a mean between 10% and 25% and an accumulated 15-year probability of 18%.22 Severe complications occur in 0.1%–0.3% and are more frequent in patients with solitary gallstones >3cm or with multiple small gallstones.23
Finally, in patients with uncomplicated symptomatic cholelithiasis, the probability of recurring symptoms after hepatic colic is 50% in the following 12 months, with an accumulative 9-year probability of 24.5%.24
Published reports about patient prioritization22,25–27 have shown evidence that, due to the complexity of interacting factors, the dissociation of an objective evaluation and real needs together with the perception of the disease make it necessary to consider the options and preferences of the users with regards to waiting list times.2 Thus, the ideal prioritization system should include clinical or objective factors as well as social factors, such as: (1) need, expected benefit or utility expressed by the patient; (2) effectiveness; (3) maximum possible benefit; (4) clinical utility from the physician's standpoint; (5) social, family and work situation of the patient; and (6) order of inclusion.16 This entails a multidimensional system that requires considering the HRQoL and expected utility.
Patients on waiting lists watch their HRQoL dwindle,28 as does their tolerance to worsening symptoms, although the acceptance of waiting times has not correlated with the objective measurements for disease impact or with socio-demographic aspects.29
Measuring HRQoL monitors health-care quality, is able to compare therapeutic modalities and quantifies the effect of the intervention with the calculation of the utility obtained.30 The GIQLI is the only HRQoL measurement that has been validated in patients with cholelithiasis13; nevertheless, it may show important differences in score among patients with the same diagnosis13,31 by including sections that reflect the perception of the disease and its treatment.13,31,32
Given the fact that the results of cholecystectomy include symptoms, emotions, and physical and social function as result indicators,33 it is not clear to what degree the changes in these should be considered clinically relevant.34 Statistically significant differences in the HRQoL may not be clinically relevant,35 which makes it essential to define these differences in absolute quantitative terms or percentages of variation in the HRQoL.36
In fact, the GIQLI shows greater sensitivity in the emotional and psychological scales compared with the SF36, although the correlation between the two is good.37
In this direction, in the paper by Mentes et al.15 the gain in HRQoL was significant in symptomatic and asymptomatic patients, although not to the same degree. These results are similar to ours, even though the CR was 50% lower in asymptomatic patients, with an increase in QoL of 10% in most patients.
The increased HRQoL in LC is related to demographic data34,38,39 as it is lower in older female patients (with poor baseline HRQoL). In our study, age did not influence HRQoL score. In women, however, similar to the Quintana et al. study,5 the decline in pre-operative QoL was greater and associated with a greater increase in QoL (CR) compared with men.
The fundamental limitation in the clinical interpretation and applicability of the GIQLI is that the minimum clinically relevant/significant difference is unknown; its definition would enable us to verify the utility of the treatment in terms of the HRQoL.37 The estimation with the CR calculation shows evidence of the gain in HRQoL (utility) of a procedure. In our study, the CR as a main measurement for outcome obtained results in the different QoL subscales that were similar to those of Shy et al.38: symptoms area 23.4 (19.1–30.8) and 22.8, respectively; emotional area 29.5 (19.7–38.8) and 43.7, respectively; physical area 23.4 (20.4–36.9) and 35.7; social areas 21.5 and 20.3; and overall score 19.4 (14.2–29.4) and 28.1. Thus, although they are very different populations (males in 45.3% in the Shy study), it can be estimated that the results are similar in both studies.
The exclusion of patients with postoperative complications eliminates the negative load (subjective and objective) on the HRQoL generated by such complications, which maximizes the objectivity of the expected and obtained utility. In this regard, the GIQLI and the SF36 have not demonstrated differences when considering the laparoscopic or conventional procedure 3 months after the intervention.33 Nonetheless, the utility in terms of CR was 15.5% for LC and 10.6% for small incision cholecystectomy (SIC); the SF36 obtained variations in favor of LC in the perceived change in health, which was not detected by the GIQLI.33 Even so, both the SF36 as well as the GIQLI obtained significant differences that highlight minimally invasive surgery as a decisive factor in improved QoL, which therefore explains why conversion (complications) entails a smaller improvement in HRQoL.
In the study by Quintana et al.5 the GIQLI showed differences for adequacy (RAND method) although the percentage of inadequacy was very low (1.1% and only 9.9% with doubtful indication). In both, there was an increase in the post-operative scores that was significantly greater when asymptomatic and symptomatic patients were compared, which shows a good correlation between the cholecystectomy adequacy evaluation system (objective selection criteria) and greater increase in HRQoL in the patients classified as appropriate.
In contrast, our study does not offer a correlation of the objective linear scoring system with the GIQLI and the 3 levels of priority established in accordance with the expected utility. There is considerable overlapping of the values of the objective system with regard to the utility obtained and, although the utility observed in the high and intermediate prioritization groups is greater than 70%, the linear system cannot define these groups.
Although the objective system does not include chronic acalculous cholecystitis as a relevant clinical factor, our previous paper40 demonstrated a higher CR in this subgroup of patients (20.2%) compared with patients with chronic lithiasic cholecystitis (13.9%), so we therefore believe that it should be included in the linear systems.
The limitations of our study include a small proportion of males, a small patient sample and a low proportion of patients with complicated cholelithiasis.
In conclusion, the lack of correlation between the HRQoL and expected and observed utility with an objective linear scoring system indicates that, in order to develop a system of prioritization, both balanced measurements should be included in a multidimensional system. It is necessary to carry out a longer study and correlate its results for “patients’ tolerance to waiting for surgery” in order to validate the results. The priority level gradation based on the GIQLI is able to guarantee a significant percentage of patients with marked impact of the disease and with a significant improvement in HRQoL.
Conflict of InterestsThe authors declare having no conflict of interests.
Please cite this article as: Planells Roig M, Cervera Delgado M, Garcia Espinosa R, Navarro Vicente F, Sanahuja Santafé Á. Evaluación del gastrointestinal quality of life index como sistema de selección para la priorización de pacientes en lista de espera de colecistectomía laparoscópica. Cir Esp. 2013;91:308–315.