Telemedicine is defined by the World Health Organization as “healing at a distance”. It has developed as a result of the application of information and communication technologies during diagnosis, follow-up and treatment, as well as the teaching and transference of medical data when distance and/or time separate participants. The aim of this study is to describe our initial experience with a telemedicine program, connecting with our reference center for the treatment of patients with severe trauma.
We performed a descriptive analysis of a series of patients treated from February 2015 to March 2016, requiring activation of the severe trauma protocol established in our Healthcare Management Area for Campo de Gibraltar, Spain, in 2011. We assessed the number of patients diagnosed who required referrals to medical specialties that do not exist at our hospital, which are classified by the Andalusian Public Healthcare System (Sistema Sanitario Público Andaluz, SSPA) as level 3 trauma, including: vascular, thoracic, cardiac and plastic surgery; interventional radiology; and neurosurgery.
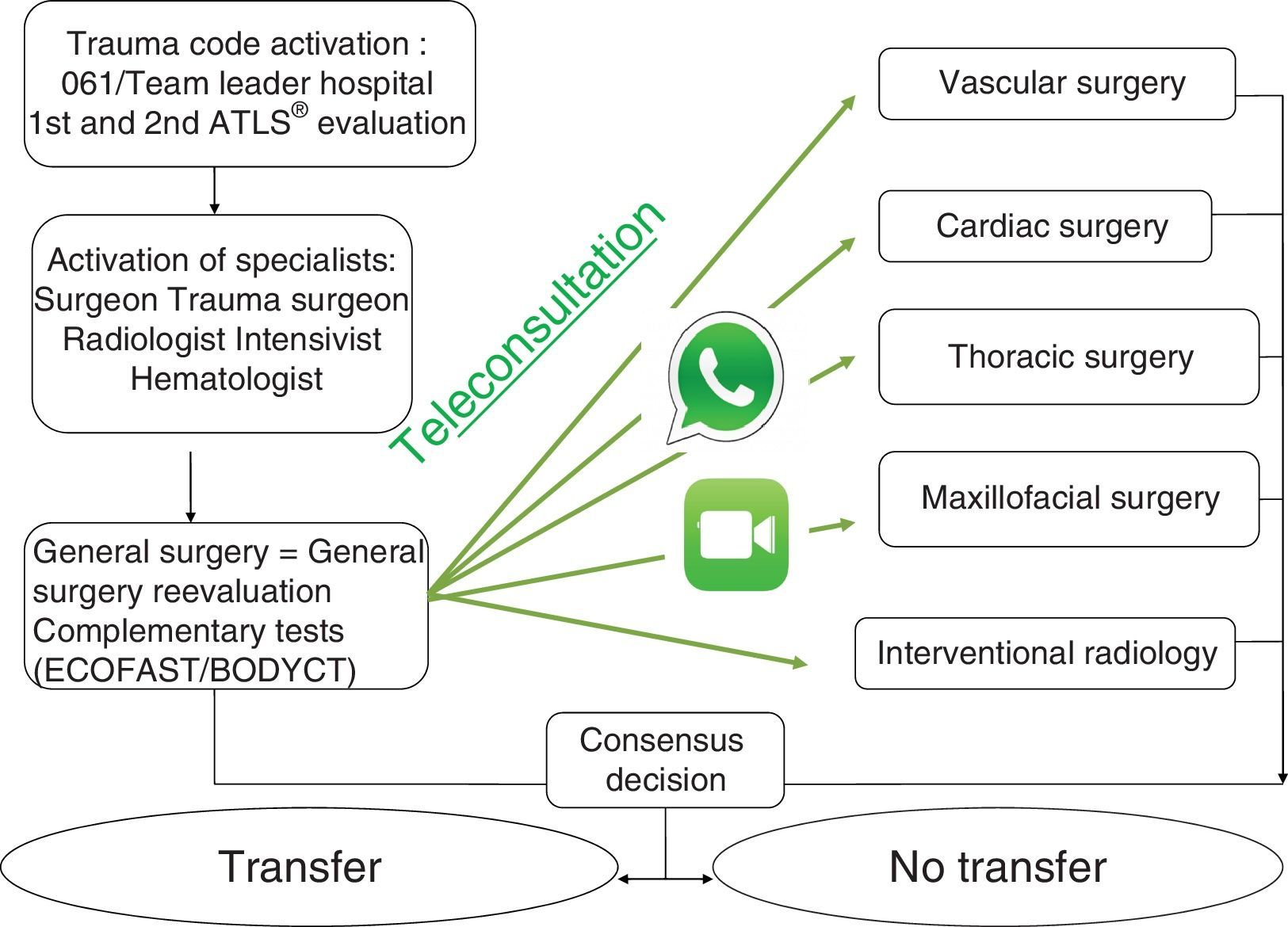
During the study period, the severe trauma care protocol was activated on 159 occasions, which was included on the registry reports approved by the multiple trauma patient care committee and completed at each activation. Teleconsultations with specialists at the reference hospital were used on 16 occasions (Fig. 1).
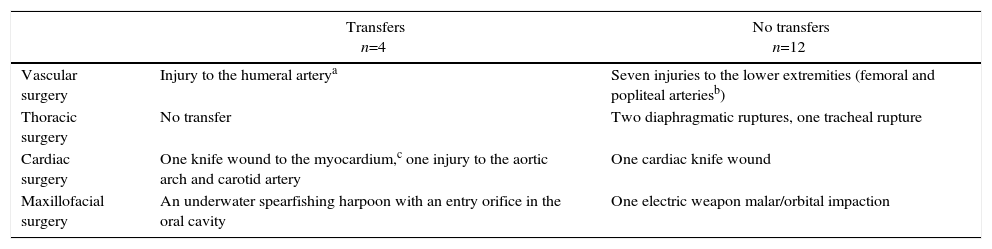
Under the guidance of these specialists, 16 patients were stabilized at our medical center, 4 of whom were transferred to the reference hospital. Therefore, 12 patients remained at our hospital until discharge and transfer was avoided. Table 1 shows details of the 16 telemedicine cases. At the bottom of the table, we explain the reasons that led to transfer/no transfer of the patients to another hospital in cases that could cause confusion.
Results.
| Transfers n=4 | No transfers n=12 | |
|---|---|---|
| Vascular surgery | Injury to the humeral arterya | Seven injuries to the lower extremities (femoral and popliteal arteriesb) |
| Thoracic surgery | No transfer | Two diaphragmatic ruptures, one tracheal rupture |
| Cardiac surgery | One knife wound to the myocardium,c one injury to the aortic arch and carotid artery | One cardiac knife wound |
| Maxillofacial surgery | An underwater spearfishing harpoon with an entry orifice in the oral cavity | One electric weapon malar/orbital impaction |
Hemodynamically stable patient with no radial pulse. CT angiography showed evidence of arterial intimal flap. The patient was transferred for endovascular treatment and returned to our hospital the same day. Patient progress was satisfactory.
Three hemodynamically unstable patients could not be transferred and 4 cases with MESS score >7, which, after consultation with vascular surgery, required amputation.
Hemodynamically stable patient with compatible CT angiogram, with injury to the aortic arch contained by hematoma; carotid artery with intimal flap and contusion, causing cerebrovascular accident. The patient was transferred after hemodynamic stabilization and previous consensus with cardiac and vascular surgery.
After a regional meeting and with the agreement of professionals involved in trauma, contact was established with specialists at reference hospitals, heads of trauma units and local coordinators of severe trauma care at each hospital, under the regional direction of EPES/061. The directors of the Accident Plan and the Integrated Healthcare Plan for Severe Trauma were informed at a regional commission meeting. The subdirectors for Information Technologies and Communication of the SSPA confirmed the feasibility of the project. All the professionals at our hospital involved in the management of severe trauma made their private telephone numbers available, with full provision for image-sharing and direct communication.
Patient consent for recording images was obtained verbally during the videotaping itself.
One of the great benefits of the utilization of technology in medicine is to be able to conduct consultations between professionals at a distance in real time. This method is ideal for use in emergency departments because of the speed and synchronous communication between medical professionals.1–4 This statement has held true in our experience with telemedicine, as we have felt supported by specialists at any time of the day or night, even though they are at a distance.
After completing trauma training courses such as ATLS and DSTC, telemedicine assists general surgeons to evolve in their daily practice of severe trauma treatment through tele-tutoring until their learning curve is completed. There are reports in the literature that the learning curve is more vertical with this method compared to more traditional ones,5–8 a fact that we have been able to verify in our limited experience.
The technical limitations of hospitals make it difficult for telemedicine to become a tool to improve severe trauma management. This limitation is theoretical, since sufficient technology is available.9 Smartphones, for instance, are accessible to the majority of the population and are a technical solution in places with no other equipment. In our hospital, as there is no telemedicine system in place, we use our personal phones with the encrypted WhatsApp® messaging app and FaceTime® from Apple®. It is therefore the lack of motivation and knowledge, coupled with legislative/legal concerns that have not been addressed, that cause resistance to the diffusion of telemedicine and is a source of controversy.10
The literature shows the advantages of telemedicine applied in our specialty, with an emphasis on reducing the number of unnecessary patient transfers. Considering the current financial problems of our healthcare system, and in keeping with the principle of equity in medical care, we believe that telemedicine is a great alternative for populations far from reference centers.
These are the preliminary results of a project that was initiated one year ago at our hospital. We feel it is necessary to wait until a larger number of patients have been treated in order to attain a study with sufficient statistical power to obtain conclusions.
Please cite this article as: Salas Díaz AS, Saavedra Chacón MJ, Ramos Durán JM, Romero Gallego JD. Evaluación de un programa de telemedicina en trauma grave. Resultados preliminares. Cir Esp. 2017;95:412–413.