Although the Nuss technique revolutionised the surgical treatment of pectus excavatum, its use has not become widespread in our country. The aim of this study was to analyse the current use of this technique in a sample of Thoracic Surgery Departments in Spain.
MethodsObservational rectrospective multicentric study analyzing the main epidemiological aspects and clinical results of ten years experience using the Nuss technique.
ResultsBetween 2001 and 2010 a total of 149 patients were operated on (mean age 21.2 years), 74% male. Initial aesthetic results were excellent or good in 93.2%, mild in 4.1% and bad in 2.7%. After initial surgery there were complications in 45 patients (30.6%). The most frequent were wound seroma, bar displacement, stabiliser break, pneumothorax, haemothorax, wound infection, pneumonia, pericarditis and cardiac tamponade that required urgent bar removal. Postoperative pain appeared in all patients. In 3 cases (2%) it was so intense that it required bar removal. After a mean follow-up of 39.2 months, bar removal had been performed in 72 patients (49%), being difficult in 5 cases (7%). After a 1.6 year follow-up period good results persisted in 145 patients (98.7%).
ConclusionNuss technique in adults has had good results in Spanish Thoracic Surgery Departments, however its use has not been generalised. The risk of complications must be taken into account and its indication must be properly evaluated. The possibility of previous conservative treatment is being analysed in several departments at present.
Aunque la introducción de la técnica de Nuss revolucionó el tratamiento quirúrgico del pectus excavatum, no se ha generalizado su uso en nuestro medio. El objetivo de este estudio es conocer la situacion actual del uso de esta técnica en una selección de Servicios de Cirugía Torácica de España.
MétodosEstudio observacional retrospectivo multicéntrico que analiza los principales aspectos epidemiológicos y resultados clínicos tras 10 años de experiencia empleando técnica de Nuss.
ResultadosEntre 2001 y 2010 se intervino a 149 pacientes (media de edad 21,2 años), 74% varones. Los resultados estéticos iniciales fueron excelentes o buenos en el 93,2%, regulares en el 4,1% y malos en el 2,7% de los casos. Un total de 45 pacientes (30,6%) presentaron complicaciones tras la primera intervención. Las más frecuentes fueron la presencia de seroma en las heridas quirúrgicas, desplazamiento de la barra, rotura del estabilizador, neumotórax, hemotórax, infección de la herida, neumonía, pericarditis y un taponamiento pericárdico que requirió la extracción de la barra de urgencia. El dolor postoperatorio fue referido por todos los pacientes y 3 de ellos (2%) requirieron la extracción precoz de la barra por dolor intratable. Tras una media de 39,2 meses, se había retirado la barra a 72 pacientes (49%), con dificultades en la extracción en 5 (7%). Tras un seguimiento medio de 1,6 años se constató buen resultado en 145 pacientes (98,7%).
ConclusionesLa técnica de Nuss en adultos ha tenido buenos resultados en los Servicios de Cirugía Torácica españoles aunque no se ha generalizado su utilización. Las posibles complicaciones se han de tener en cuenta, por lo que la indicación debe ser muy bien valorada. La posibilidad de un tratamiento conservador previo es valorado por alguno de los servicios en la actualidad.
Pectus excavatum (PE) or excavated, sunken or funnel chest is a malformation of the anterior wall of the thorax. It is characterised by a deep depression of the sternum and alteration of the lower sternochondral joints.1
Patients affected by this deformity suffer cosmetic, psychological and social effects, although functional ones are usually mild. Thoracic organ compression with clinical repercussion2 only occurs in the most severe cases. The treatment of PE is fundamentally surgical, and it has evolved over time. The traditional surgical technique is the Ravitch procedure, which involves an approach through anterior thoracic incisions, the resection of 3 or 4 rib cartilages on each side plus complete or partial flattening of the sternum.3
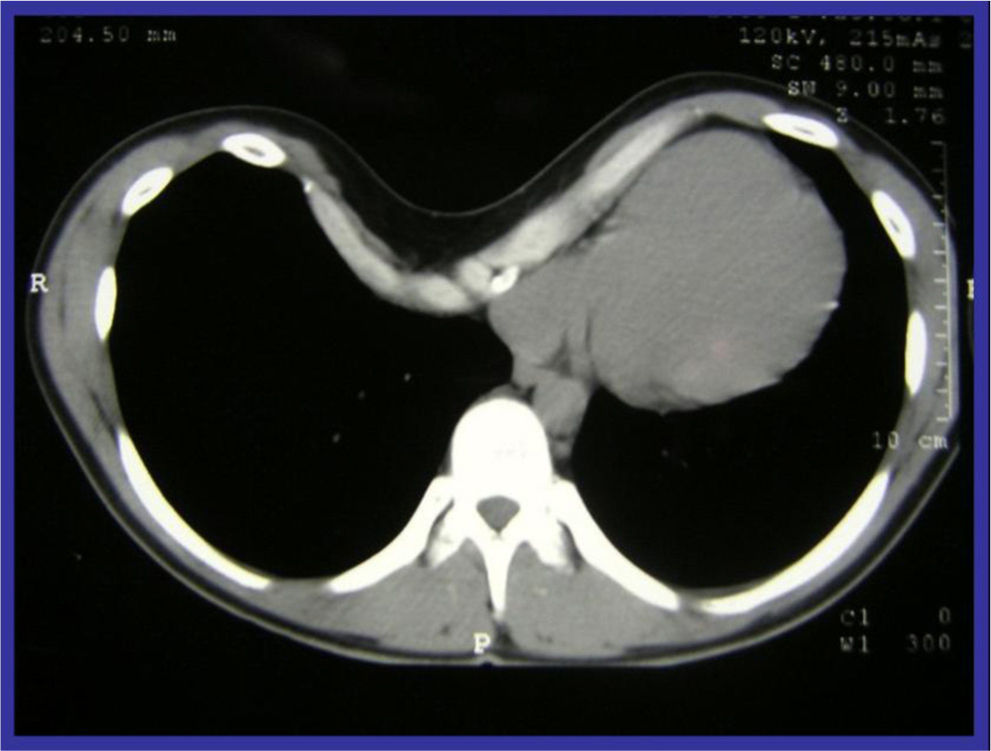
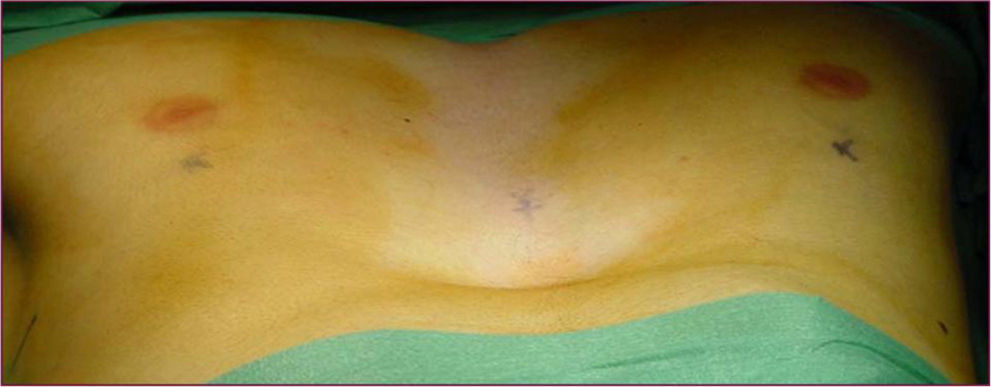
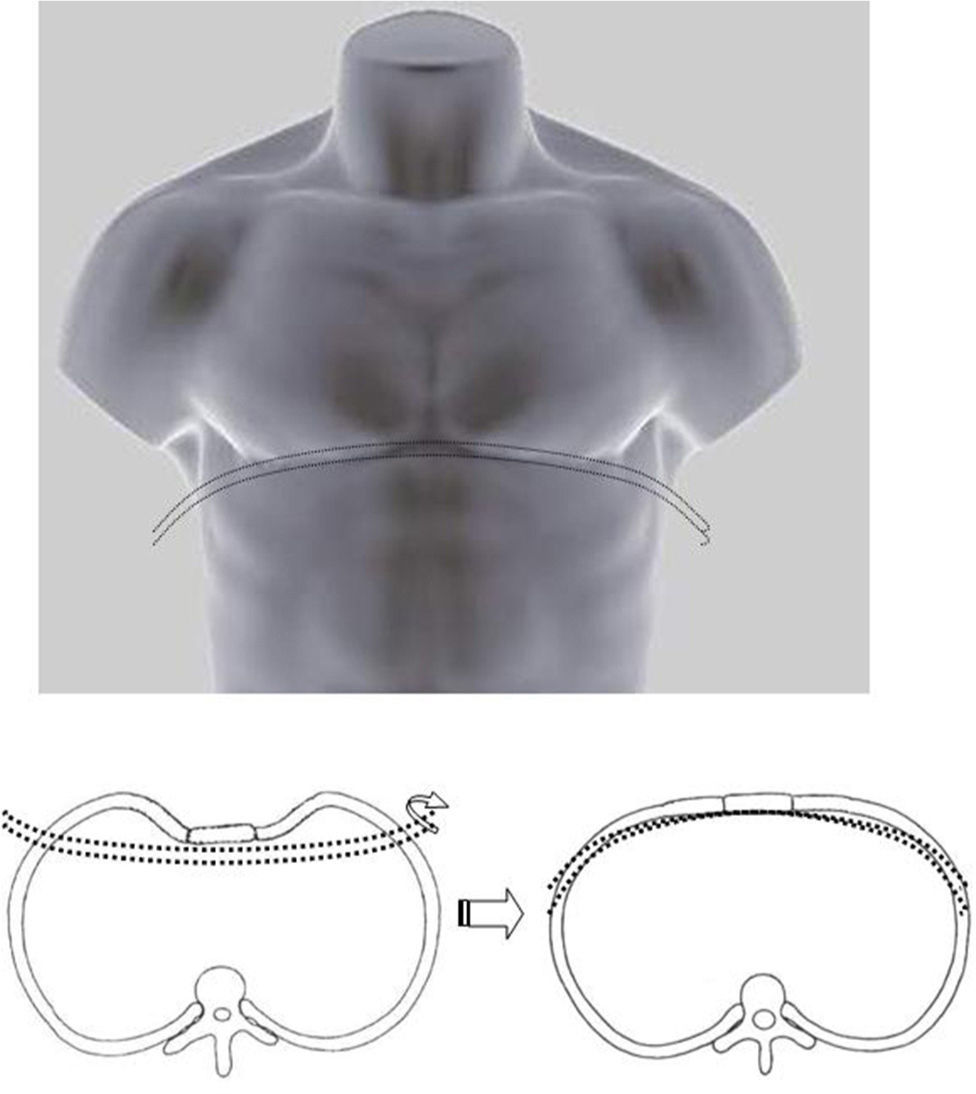
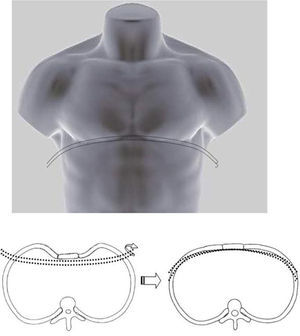
Classical surgical treatment of PE underwent a revolution in the 1990s with the introduction of the procedure of Donald Nuss. This consists of raising the deformity by inserting a bar below the sternum through 2 lateral incisions, which leads to a better appearance than the classic Ravitch procedure4 (Figs. 1–5). This procedure requires no other incisions, rib resections or sternotomy. The most frequent complications described in the bibliography are postoperative pain, seromas in the surgical wounds and displacement of the bar.5
This new procedure has given rise to great enthusiasm since its introduction, although it is still not in widespread use. The aim of this study is to examine the current status of Nuss procedure usage in a representative selection of Thoracic Surgery Departments in Spain.
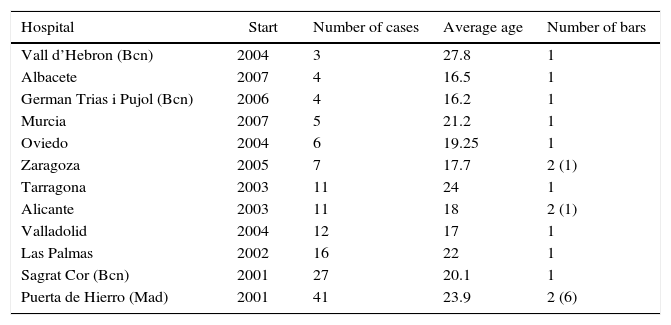
MethodsThis retrospective observational multicentre study commenced with the collection of clinical variables from the hospitals shown in Table 1, in response to the request to fill in a questionnaire. Patient demographic variables were recorded, together with immediate surgical results, the number of bars used, the need for carbon dioxide insufflation, complications and postoperative pain, incidents during follow-up and results, together with satisfaction. Data were analysed descriptively and compared with other previously published series. Each one of the Ethics Committees of the hospitals taking part authorised the study according to the regulations stipulated by the Patient Data and Autonomy Protection Law 41/2002.
Hospitals That Took Part.
| Hospital | Start | Number of cases | Average age | Number of bars |
|---|---|---|---|---|
| Vall d’Hebron (Bcn) | 2004 | 3 | 27.8 | 1 |
| Albacete | 2007 | 4 | 16.5 | 1 |
| German Trias i Pujol (Bcn) | 2006 | 4 | 16.2 | 1 |
| Murcia | 2007 | 5 | 21.2 | 1 |
| Oviedo | 2004 | 6 | 19.25 | 1 |
| Zaragoza | 2005 | 7 | 17.7 | 2 (1) |
| Tarragona | 2003 | 11 | 24 | 1 |
| Alicante | 2003 | 11 | 18 | 2 (1) |
| Valladolid | 2004 | 12 | 17 | 1 |
| Las Palmas | 2002 | 16 | 22 | 1 |
| Sagrat Cor (Bcn) | 2001 | 27 | 20.1 | 1 |
| Puerta de Hierro (Mad) | 2001 | 41 | 23.9 | 2 (6) |
We present the experience of 12 Spanish Thoracic Surgery Departments with the Nuss procedure, from its introduction in October 2001 until November 2010 (Table 1). This retrospective observational study revised the clinical histories of operated patients, including epidemiological data, surgical incidents, postoperative complications and results. The Ethics Committees of all the hospitals taking part authorised this study.
Results20 Spanish Thoracic Surgery Departments were asked whether or not they performed the Nuss procedure in the treatment of PE. Of these, 12 (60%) stated that they had used it. In total, these 12 hospitals had operated on 149 patients aged from 10 to 47 years of age (average age 21.2 years old), of whom 74% were male. In 2 patients (aged 32 and 37 years old) the operation could not be concluded due to the impossibility of raising the sternum. Two departments had operated on 68 patients (46.3%) while the other 10 departments had operated an average of 7.9 patients (range 3–16). A single bar was usually inserted, except in 8 cases when 2 were used (5.4%). Intrathoracic insufflation of CO2 was used in 2 hospitals to increase pulmonary collapse and facilitate the procedure. The initial cosmetic results, as described by the patients themselves, were excellent or good in 137 cases (93.2%), fair in 6 cases (4.1%) and poor in 4 (2.7%). A total of 45 patients (30.6%) presented complications after the first operation, the most frequent of which was seroma in the surgical wounds (17 patients), displacement of the bar (8 patients), in 5 of which another operation was necessary, breakage of the absorbable stabiliser (3 patients), pneumothorax requiring drainage (3 patients), haemothorax in 2 patients that required a repeat operation in one case and drainage in the other, infection of the wound (4 patients), pneumonia one month after the operation (one patient), pericarditis (one patient); another patient suffered pericardiac blockage and respiratory failure one month after the operation which made the emergency removal of the bar necessary. The visual-analogue scale (VAS) was used to evaluate postoperative pain. All of the patients mentioned postoperative pain (100%) in differing degrees, and in 3 of them (3/147: 2%) the bar had to be extracted early due to untreatable pain.
The bar was removed from 72 patients (49%) after an average of 39.2 months. Difficulties in extracting it were found due to erosion of the ribs in 3 patients, and intercostal bleeding occurred in one patient that required enlargement of the incision for suture. Haemothorax occurred in one case, requiring thoracoscopy and drainage. After an average follow-up of 1.6 years a good result was found in 145 patients (98.7%). The result was not considered to be satisfactory in 2 patients, and they had to be operated again using the Ravitch procedure.
DiscussionPE is the most common congenital malformation of the thoracic wall. It appears in one of every 300 to 400 newly-born live infants and is at its most severe during adolescence.
30% of patients have a family history of cases.6 This disease is associated with other abnormalities of the musculoskeletal system, the most frequent of which are scoliosis and Marfan's and Ehlers Danlos syndrome. Spontaneous regression or any other partial improvement in this defect is very rare.7 The pathogenesis of PE is unclear. The resulting defect is an alteration in the development of the costochondral regions of the anterior thoracic wall that leads to symmetrical as well as asymmetrical abnormalities.8
The optimum age for surgical correction is at the start of puberty: from 11 to 13 years old.9 Surgery in adults gives good cosmetic results, especially in patients with symmetrical PE and a not very rigid thorax; however, a higher incidence of complications has been described for adult patients than with paediatric ones.10,11
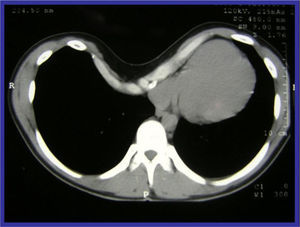
The surgical indication is cosmetic in 90% of cases, although if the Haller index–the result of dividing the horizontal diameter of the thorax in CT by the vertical diameter–is greater than 3.25 this is considered to be an objective criteria for surgery.12
For many years the classic surgery to correct PE was the Ravitch procedure. Although this solved the problem in the majority of cases, the need for a long incision, the resection of the deformed cartilages and the subsequent osteotomies, during surgery that lasts a considerable time to correct a defect which in the majority of cases is cosmetic, led many thoracic surgeons to be reluctant to operate on these patients.13
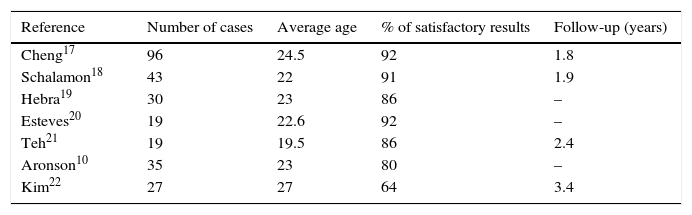
This minimally invasive technique to correct PE was introduced in 1997. It is based on the principle that if the bar is kept in place for 3 years, this leads to a remodelling of the thoracic malformation (in a similar way to the process in orthodontic procedures), which is definitively consolidated.14 In cases with major deformation and in patients with Marfan's syndrome it is sometimes advisable to use 2 bars.15 The metal implant is removed after 3 years in an out-patient procedure.16 The Nuss procedure has gained increasing acceptance since it was introduced, among paediatric surgeons above all but also to a lesser degree among thoracic surgeons. Analysis of the published studies shows that its use in adults has led to similar results to those of the classic procedure10,17–22 (Table 2).
The surgical treatment of PE has also been controversial. The new Nuss procedure aroused great initial enthusiasm, and in fact the number of operations for PE tripled. The reason for this growth was not that there were more operable cases, but rather due to the appeal of the words “minimally invasive”. Individuals who in the past had refused classic open surgery accepted treatment using the Nuss bar.23
Nevertheless, there is no general consensus among thoracic surgeons on this procedure: while some consider it to be the “gold standard”,24,25 others disagree.26
In November 1999 Dr. Leoncio Bento (a paediatric surgeon in the Virgen del Camino Hospital [Pamplona]) introduced the Nuss procedure in Spain, training paediatric surgeons to operate on PE patients younger than 14 years old. Thoracic Surgery departments started to use this technique in adult patients in 2001.27
According to a recent revision, neither procedure (Ravitch and Nuss) has been proven to be better than the other in terms of complications and results in adults.11 The personal preference of each surgeon and their experience determines whether they will use one or the other.
When the results of this study are analysed, and following more than 10 years experience, we are able to conclude that the Nuss procedure to correct PE in Spain has very high success rates (above 90%), with complications similar to those described in the literature (30%). However, in spite of the initial enthusiasm and its good cosmetic results, this procedure is not in widespread use by Spanish Thoracic Surgery Departments. This may be due to several factors: (a) the complication rate–at around 30%–is high; (b) severe postoperative pain is very frequent, so epidural analgesia has to be maintained for as long as is necessary, and the bar may even have to be removed because of intolerable pain; (c) although the risk of serious complications is low, it does exist,28–30; (d) in many hospitals few adults consult due to PE, so that it would be hard to commence and maintain a learning curve using this procedure.
New procedures have emerged recently, such as Taulinoplasty,31 in which a plate affixed to the sternum applies traction to it and corrects its sinking without the need to enter the thoracic cavity. Some departments including ours are now also evaluating the previous use of conservative treatment such as the vacuum bell. The vacuum bell consists of a suction bell that creates a vacuum when it is applied to the sternochondral depression. This vacuum is created manually by the patient using a bulb, and it immediately raises the sternum and ribs. This apparatus has to be used for at least 30min twice a day. Its side-effects associated with excessive use include the appearance of a subcutaneous haematoma, petechiae and dorsalgia. It is especially useful in patients with slight to moderate symmetrical PE. In a study of 34 patients, after 3 months usage it was shown to bring about the permanent raising of the sternum of at least 1.5cm in 79% of cases. It has also been shown to be of use in operations, as it aids the passage of the Nuss bar under the sternum.31,32
To conclude, the Nuss procedure to correct PE gives good cosmetic results, although it is not widely used by Spanish Thoracic Surgery Departments. As the operation takes place in “healthy patients”, complications in one third of them have to be taken into account, so that the patient himself has to consider this indication highly positive. PE repair is still evolving and new techniques are appearing which make it unnecessary to enter the thoracic cavity, thereby reducing the complications that this may involve.
Conflict of InterestsThe authors have no conflict of interests to declare in this paper.
Please cite this article as: Fibla JJ, Molins L, Moradiellos J, Rodríguez P, Heras F, Canalis E, et al. Experiencia de los Servicios de Cirugía Torácica españoles en el tratamiento del pectus excavatum mediante la técnica de Nuss. Cir Esp. 2016;94:38–43.