Pancreatic neuroendocrine tumours (PNETs) represent 1%–2% of all pancreatic neoplasms, with an approximate incidence of 1:100000persons/year.1 PNETs are believed to originate in the pluripotent stem cells of the pancreatic ductal epithelium and from mature and differentiated endocrine cells; this heterogeneity of cell types involved is associated with a wide range of clinical syndromes related with hormone hypersecretion and overproduction.2 Functioning tumours usually present prematurely because of an associated clinical syndrome, and they are often small.3 In contrast, non-functioning tumours generally appear later, are larger in size and give rise to symptoms secondary to the neighbouring compression, invasion or metastases.3 However, in recent years, thanks to the generalised use of computed tomography (CT) and magnetic resonance imaging (MRI), there has been a growing number of small, asymptomatic and non-functioning tumours discovered incidentally.2
The classic and most frequent enhancement pattern of PNETs is that of a hyperdense lesion in the arterial and venous phases on CT, and hyperintense during the arterial/pancreatic phase on the MRI dynamic study, which explains the hypervascular nature of these lesions.2,3 A pattern of hypovascular enhancement on CT and MRI, as presented in this article, is very unusual and has been described in only a few reports and studies of clinical case series.4–7
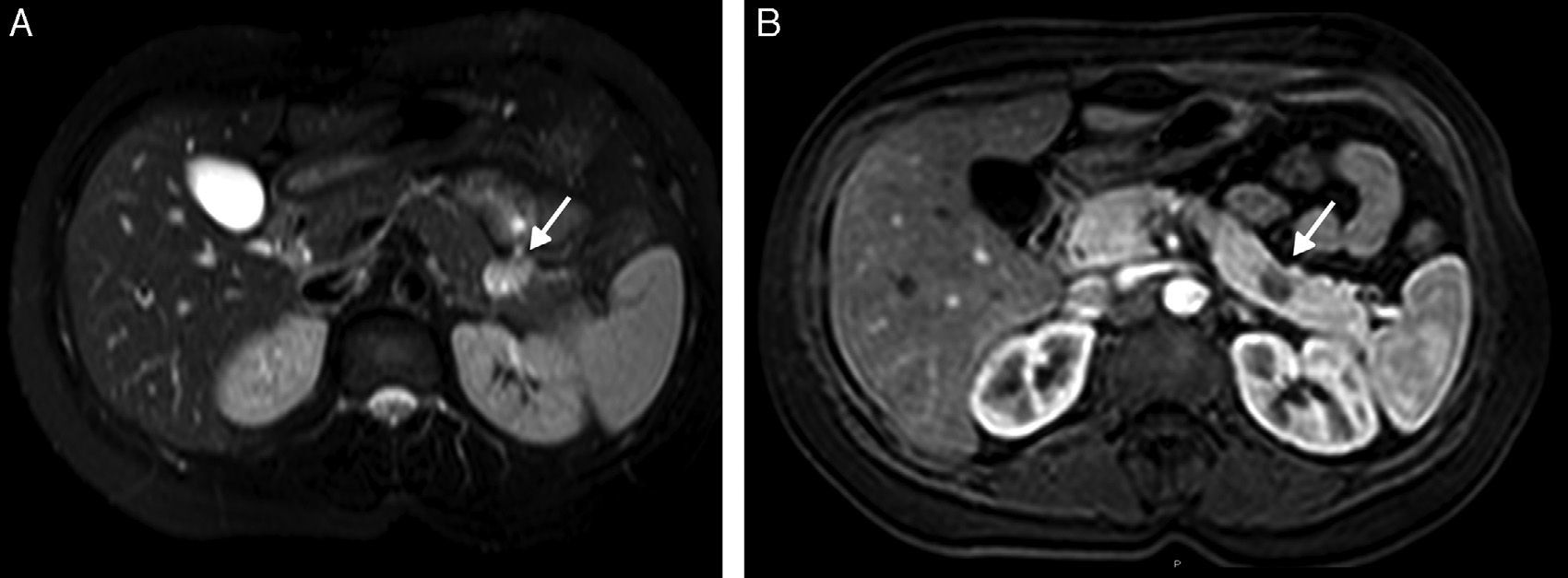
A 34-year-old woman with no prior medical history was referred to the emergency department for clinical suspicion of acute pyelonephritis and to conduct an exploration by CT scan. In this clinical context, the abdominal CT examination was done, and during the portal and equilibrium phases without contrast (in accordance with hospital protocol) a small, well-defined round lesion (1.3cm) was revealed in the junction of the body and tail of the pancreas. It was hypovascular in the portal phase compared with the surrounding parenchyma (Fig. 1). No internal calcifications or defined cystic/necrotic areas were observed, nor were there any signs of dilatation or peripancreatic invasion. The laboratory tests done in the posterior diagnostic study, which included tumour markers and hormone levels in serum, provided no unusual results. Abdominal MRI exploration showed a lesion that appeared hyperintense on T2-weighted images, with a hypovascular enhancement pattern on T1-weighted images done after the administration of gadolinium (Fig. 2). An endoscopic ultrasound (EUS) was performed, which revealed that the lesion was somewhat hypoechoic in the surrounding pancreatic parenchyma. The cytology and immunohistochemistry analyses of samples obtained by EUS-guided fine-needle aspiration were able to establish the diagnosis of well-differentiated neuroendocrine tumour (G1; Ki-67 index≤2%).8 The patient and her doctors chose a non-surgical approach; at the 3-month, 6-month and one-year follow-ups, the mass had remained stable and the patient was asymptomatic. Currently, the guidelines of the European Neuroendocrine Tumours Society (ENETS) accept a conservative approach in certain cases of PNETs<2cm that are non-functioning and incidental findings.8 Although a surgical histopathological diagnosis cannot be established in these select cases, recent studies have demonstrated that EUS-guided fine-needle aspiration is highly sensitive and specific for diagnosing PNETs, without false positive diagnoses, especially when associated with immunocytology techniques and adequate samples.9 Furthermore, high degrees of reproducibility and interobserver agreement have been described between EUS-guided fine-needle aspiration and surgical samples for the classification of the tumours with the Ki-67 index.10
The contrast uptake pattern of PNETs seen on CT and MRI has been the subject of several articles in the literature. On CT with contrast enhancement, PNETs are classically hyperdense compared with the surrounding pancreas.2,3 The characteristic tumour blush provides greater visibility and generally differentiates them from other pancreatic neoplasms, especially adenocarcinomas, which are usually hypodense in contrast enhancement phases.2,3 On MRI, most PNETs show low signal intensity in T1-weighted images with fat suppression and moderately high signal intensity in T2-weighted images with fat suppression.
Various explanations have been proposed about the finding of hypovascular enhancement in PNETs. Iglesias et al. reported a hypovascular insulinoma with important amyloid deposits and poor vascularisation in the histopathologic study.4 Inan et al. reported an atypical insulinoma that was functional and hypointense on T1-weighted images and in T2 with delayed enhancement, which was initially hypovascular; based on pathological correlation, these findings were attributed to an extensive desmoplastic reaction, as if an elevated collagen content in the fibrotic tissue shortened the relaxation time in T2.7 Hong et al.6 referred to these hypovascular tumours as a “delayed enhancement” type because, when an important part of the tumour is composed of hypovascular connective tissue stroma, gradual retention of the contrast medium in the extracellular interstitial tissue could explain the delayed enhancement unlike the background pancreatic parenchyma.6 Although the rich vascular supply is often proposed as the cause of the hypervascular appearance of PNETs in diagnostic imaging tests (and, therefore, a deficient vascular supply in the hypovascular type),2–4,7 a recent study5 has found no correlation between the mean blood vessel density (as observed in pathological samples) and the MRI pattern, which would suggest that other additional factors (like blood flow, blood volume and vascular permeability) could be implicated in this appearance on MRI.5
In short, hypovascular enhancement is an atypical pattern of PNETs and a challenge for diagnostic imaging. However, characteristics like the small size of these lesions that are accidentally discovered in asymptomatic patients and a hyperintense T2-weighted signal, as demonstrated in our case, can be key to establishing a correct diagnosis and the differentiation from other pancreatic lesions, such as adenocarcinomas.
Please cite this article as: Torres US, Nicoletti Cesar D, D’Ippolito G. Tumor neuroendocrino del páncreas hipovascular y no funcionante: una presentación inusual de una neoplasia infrecuente. Cir Esp. 2016;94:182–184.