Age has been classically considered as a determining factor for the development of postoperative complications related to lung resection for bronchogenic carcinoma. The Postoperative Complications Study Group of the Spanish Society of Thoracic Surgery has promoted a registry to analyze this factor.
MethodsA total of 3307 patients who underwent any type of surgical resection for bronchogenic carcinoma have been systematically and prospectively recorded in any of the 24units that are part of the group. Several variables related to comorbidity and age, as well as postoperative complications, were analyzed.
ResultsThe mean age of patients was 65.44. Men were significantly more common than female. The most frequent complication was prolonged air leak, which was observed in more than one third of patients. In a univariant analysis, air leak presence and postsurgical atelectasis showed statistical association with patient age, when stratified in age groups. In a multivariate analysis, age was recognized as an independent prognostic factor in relation to air leak onset. However, this could not be confirmed for postoperative atelectasis.
ConclusionAge is a predisposing factor for the development of postoperative complications after lung resection. Other associated factors also influence the occurrence of these complications.
La edad del paciente ha sido clásicamente interpretada como un factor condicionante de la aparición de complicaciones postoperatorias en cirugía de resección pulmonar por carcinoma broncogénico. El Grupo de Estudio de Complicaciones Postoperatorias de la Sociedad Española de Cirugía Torácica promovió un registro que permitiera analizar este hecho.
MétodosSe recogieron de forma consecutiva, sistemática y prospectiva los datos de un total de 3.307 pacientes tratados con algún tipo de resección quirúrgica por carcinoma broncogénico en las 24 unidades que forman parte del grupo. Fueron analizadas variables relativas a la comorbilidad y la edad del paciente, así como a las complicaciones postoperatorias acaecidas.
ResultadosLa edad media de los pacientes intervenidos fue de 65,44 años. La población masculina en la serie era significativamente mayor que la femenina. La complicación más frecuente fue la fuga aérea prolongada, que ocurrió en más de un tercio de los pacientes. En el estudio univariante, la aparición de fugas aéreas y de atelectasias posquirúrgicas mostraron asociación estadística con la edad de los enfermos, analizada por grupos etarios. En el análisis multivariante, la edad se presentó como un factor pronóstico independiente en relación con la aparición de fugas aéreas posquirúrgicas, no así en cuanto a las atelectasias posresección.
ConclusiónLa edad es un factor predisponente para el desarrollo de complicaciones postoperatorias tras resección pulmonar en nuestro medio, si bien otros factores asociados condicionan también la aparición de estas complicaciones.
Although bronchogenic carcinoma surgery (and for that matter, lung resections in general) has experienced remarkable development in recent years, it has been the progression of video-assisted surgery that has provided probably the greatest revolution in the field of thoracic surgery since the end of the last century.1 This, along with other technical advances, has meant that we are now able to surgically treat patients who previously would have been ruled out for surgery because of their comorbidities. For instance, age was classically interpreted as a determining factor in the expected morbidity after lung resection and, therefore, in the selection of patients who were candidates for lung surgery. Whereas in the early 1990s it was common practice to dismiss surgical treatment in patients over the age of 70,2,3 today patients between the sixth and eighth decades of life represent the vast majority of the population considered candidate for surgery at our hospitals.4
Given this situation, the Postoperative Complications Group of the Spanish Society of Thoracic Surgery (Group de Complicaciones Postoperatorias de la Sociedad Española de Cirugía Torácica, GCP-SECT) has promoted a study to analyze the current impact of age as a predisposing factor for postoperative complications in the context of lung cancer resections.
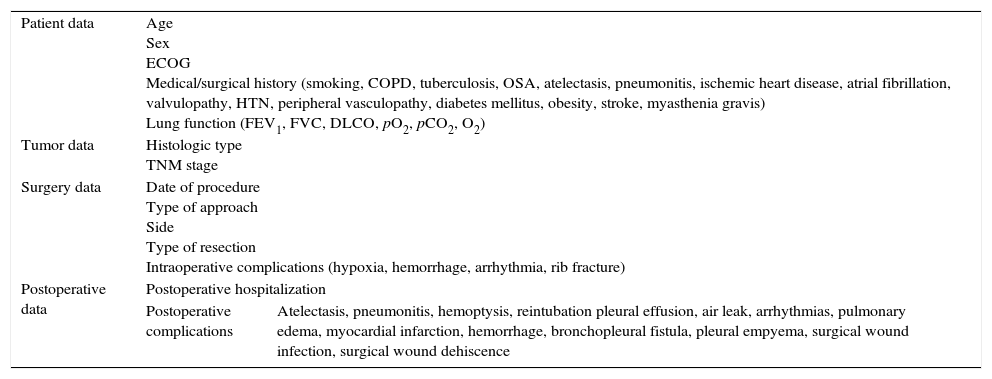
MethodsFrom the period of time between June 1, 2012 and November 30, 2014, the GCP-SECT systematically and prospectively collected data from a total of 3307 patients treated with some type of pulmonary resection due to bronchogenic carcinoma. In this multicenter project, a total of 24 thoracic surgery departments participated, each belonging to a different hospital throughout Spain. The participating hospitals are listed in Addendum A. Data were obtained for the following variables: related with age, sex, patient medical history, surgery conducted and postoperative complications (Table 1). These data were compiled consecutively and anonymously in a computerized database with online internet access, and the information was stored in a Excel file stored by the GCP-SECT. All the participating hospitals have followed the guidelines of the Patient Personal Data Protection Law. These data were stratified according to 3 age groups: 70 years of age or younger (group A), between 70 and 80 years of age (group B) and 80 years of age or older (group C).
Collected Variables.
| Patient data | Age Sex ECOG Medical/surgical history (smoking, COPD, tuberculosis, OSA, atelectasis, pneumonitis, ischemic heart disease, atrial fibrillation, valvulopathy, HTN, peripheral vasculopathy, diabetes mellitus, obesity, stroke, myasthenia gravis) Lung function (FEV1, FVC, DLCO, pO2, pCO2, O2) | |
| Tumor data | Histologic type TNM stage | |
| Surgery data | Date of procedure Type of approach Side Type of resection Intraoperative complications (hypoxia, hemorrhage, arrhythmia, rib fracture) | |
| Postoperative data | Postoperative hospitalization | |
| Postoperative complications | Atelectasis, pneumonitis, hemoptysis, reintubation pleural effusion, air leak, arrhythmias, pulmonary edema, myocardial infarction, hemorrhage, bronchopleural fistula, pleural empyema, surgical wound infection, surgical wound dehiscence | |
The inclusion criteria of this registry were: patients with a histological diagnosis of bronchogenic carcinoma who had undergone surgery with curative intent at the Thoracic Surgery Departments within Spain, including atypical lung resection, segmentectomy, lobectomy, bilobectomy or pneumonectomy. In order to provide the study with homogeneity, exclusion criteria were: exploratory video-assisted thoracoscopies or thoracotomies, life-saving emergency surgeries and cases with synchronous tumors.
The statistical study was carried out with SPSS 21.0 for Windows. The Student's t test was used for the comparison of numerical variables with other dichotomic categories. The comparison of numerical variables with other categorical variables of more than 2 categories was performed with the single-factor ANOVA test. The comparison of qualitative variables was done with the chi-squared test and the multivariate study with a logistic regression test. A P value <.05 was considered statistically significant.
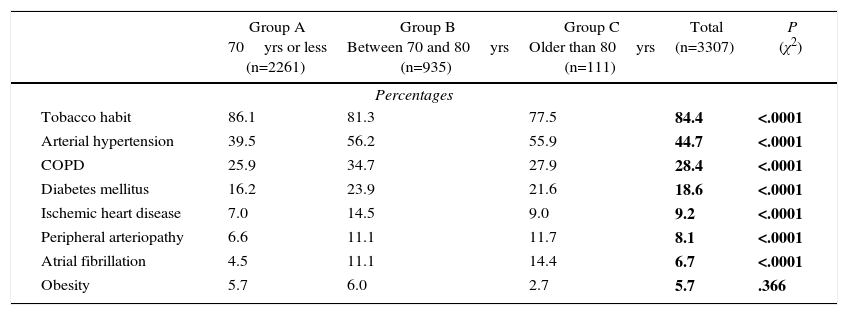
ResultsIncluded in the study were 3307 patients, 2566 (77.6%) of which were men. The preoperative comorbidity data of the series are shown in Table 2. In the analysis of these data, we have found statistically significant differences in the incidence of previous disease, according to different age groups.
Preoperative Comorbidity of the Series (According to Age Groups).
| Group A 70yrs or less (n=2261) | Group B Between 70 and 80yrs (n=935) | Group C Older than 80yrs (n=111) | Total (n=3307) | P (χ2) | |
|---|---|---|---|---|---|
| Percentages | |||||
| Tobacco habit | 86.1 | 81.3 | 77.5 | 84.4 | <.0001 |
| Arterial hypertension | 39.5 | 56.2 | 55.9 | 44.7 | <.0001 |
| COPD | 25.9 | 34.7 | 27.9 | 28.4 | <.0001 |
| Diabetes mellitus | 16.2 | 23.9 | 21.6 | 18.6 | <.0001 |
| Ischemic heart disease | 7.0 | 14.5 | 9.0 | 9.2 | <.0001 |
| Peripheral arteriopathy | 6.6 | 11.1 | 11.7 | 8.1 | <.0001 |
| Atrial fibrillation | 4.5 | 11.1 | 14.4 | 6.7 | <.0001 |
| Obesity | 5.7 | 6.0 | 2.7 | 5.7 | .366 |
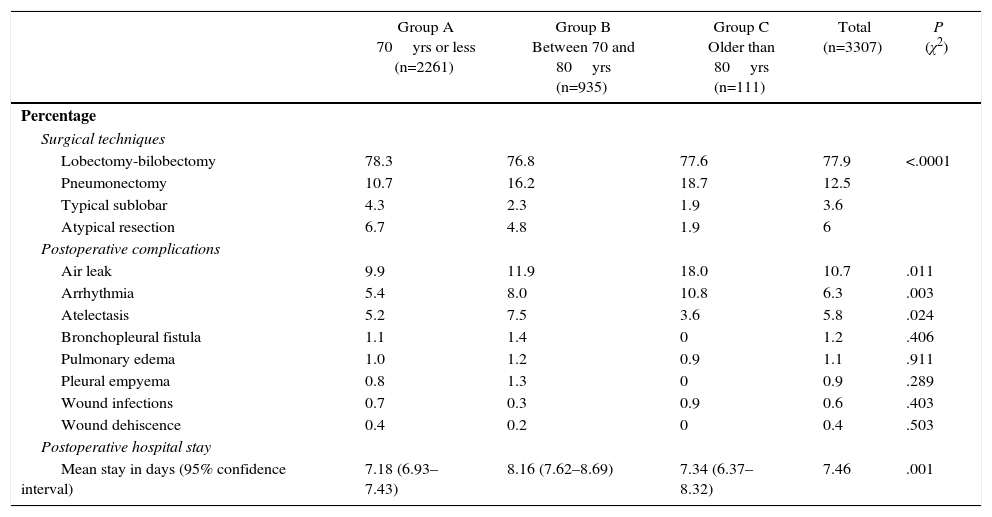
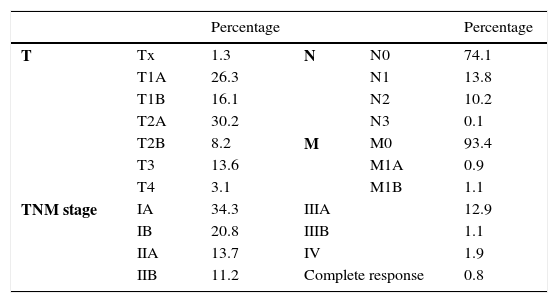
Less than one-third of the patients were treated with video-assisted surgery (n=1028; 31.1%). As for laterality, in 1804 cases (54.6%) the tumor was located in the right hemithorax, versus 1503 (45.4%) in the left. The different surgical techniques are shown in Table 3. Although statistically significant differences were found among the different age groups, there was no observed greater tendency of atypical resections in older age groups that would bias the results obtained. As for the pathological/surgical tumor stage, the classification data according to the 2009 TNM classification (7th Edition) of the different cases can be observed in Table 4.
Surgical Techniques, Postoperative Complications and Postoperative Hospital Stay Recorded for This Analysis (Stratified by Age Groups).
| Group A 70yrs or less (n=2261) | Group B Between 70 and 80yrs (n=935) | Group C Older than 80yrs (n=111) | Total (n=3307) | P (χ2) | |
|---|---|---|---|---|---|
| Percentage | |||||
| Surgical techniques | |||||
| Lobectomy-bilobectomy | 78.3 | 76.8 | 77.6 | 77.9 | <.0001 |
| Pneumonectomy | 10.7 | 16.2 | 18.7 | 12.5 | |
| Typical sublobar | 4.3 | 2.3 | 1.9 | 3.6 | |
| Atypical resection | 6.7 | 4.8 | 1.9 | 6 | |
| Postoperative complications | |||||
| Air leak | 9.9 | 11.9 | 18.0 | 10.7 | .011 |
| Arrhythmia | 5.4 | 8.0 | 10.8 | 6.3 | .003 |
| Atelectasis | 5.2 | 7.5 | 3.6 | 5.8 | .024 |
| Bronchopleural fistula | 1.1 | 1.4 | 0 | 1.2 | .406 |
| Pulmonary edema | 1.0 | 1.2 | 0.9 | 1.1 | .911 |
| Pleural empyema | 0.8 | 1.3 | 0 | 0.9 | .289 |
| Wound infections | 0.7 | 0.3 | 0.9 | 0.6 | .403 |
| Wound dehiscence | 0.4 | 0.2 | 0 | 0.4 | .503 |
| Postoperative hospital stay | |||||
| Mean stay in days (95% confidence interval) | 7.18 (6.93–7.43) | 8.16 (7.62–8.69) | 7.34 (6.37–8.32) | 7.46 | .001 |
TNM Categories and Tumor Stages in the Series According to the 2009 TNM Classification (7th Edition).
| Percentage | Percentage | ||||
|---|---|---|---|---|---|
| T | Tx | 1.3 | N | N0 | 74.1 |
| T1A | 26.3 | N1 | 13.8 | ||
| T1B | 16.1 | N2 | 10.2 | ||
| T2A | 30.2 | N3 | 0.1 | ||
| T2B | 8.2 | M | M0 | 93.4 | |
| T3 | 13.6 | M1A | 0.9 | ||
| T4 | 3.1 | M1B | 1.1 | ||
| TNM stage | IA | 34.3 | IIIA | 12.9 | |
| IB | 20.8 | IIIB | 1.1 | ||
| IIA | 13.7 | IV | 1.9 | ||
| IIB | 11.2 | Complete response | 0.8 | ||
The most frequent histological types in the series were adenocarcinoma and epidermoid carcinoma. 51% of the resected tumors presented histology for adenocarcinoma, versus 36.6% epidermoid carcinomas. Undifferentiated large-cell carcinoma was 2.9%, and undifferentiated small-cell was 0.9%.
Mean age of the surgically treated patients was 65.4 (standard deviation: 9.7), with a median of 66. Stratified by age groups, 68.4% of the patients belonged to group A, 28.3% of the cases to group B and 3.4% to group C. As for the relationship between patient age and sex, the male population was significantly older than the feminine population (mean age 66.5 vs 61.9; P<.0001).
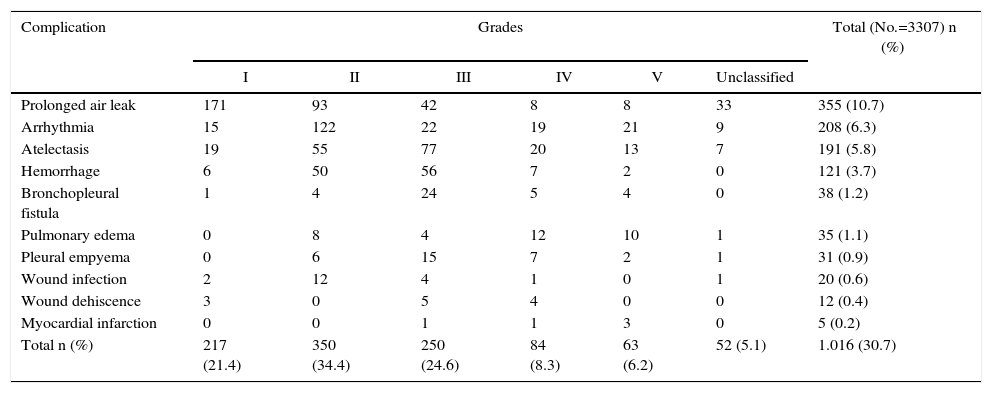
Some type of postoperative complication was observed in 30.7% of the patients after lung resection. Among those recorded in this study, the most frequent complication (10.7%) was prolonged air leak (defined as a leak persisting beyond the 5th day post-op). In 94.9% of cases, these complications were classified according to the Clavien–Dindo severity score (Table 5).
Distribution of Postoperative Complications According to the Clavien–Dindo Classification (in Number of Cases).
| Complication | Grades | Total (No.=3307) n (%) | |||||
|---|---|---|---|---|---|---|---|
| I | II | III | IV | V | Unclassified | ||
| Prolonged air leak | 171 | 93 | 42 | 8 | 8 | 33 | 355 (10.7) |
| Arrhythmia | 15 | 122 | 22 | 19 | 21 | 9 | 208 (6.3) |
| Atelectasis | 19 | 55 | 77 | 20 | 13 | 7 | 191 (5.8) |
| Hemorrhage | 6 | 50 | 56 | 7 | 2 | 0 | 121 (3.7) |
| Bronchopleural fistula | 1 | 4 | 24 | 5 | 4 | 0 | 38 (1.2) |
| Pulmonary edema | 0 | 8 | 4 | 12 | 10 | 1 | 35 (1.1) |
| Pleural empyema | 0 | 6 | 15 | 7 | 2 | 1 | 31 (0.9) |
| Wound infection | 2 | 12 | 4 | 1 | 0 | 1 | 20 (0.6) |
| Wound dehiscence | 3 | 0 | 5 | 4 | 0 | 0 | 12 (0.4) |
| Myocardial infarction | 0 | 0 | 1 | 1 | 3 | 0 | 5 (0.2) |
| Total n (%) | 217 (21.4) | 350 (34.4) | 250 (24.6) | 84 (8.3) | 63 (6.2) | 52 (5.1) | 1.016 (30.7) |
In this manner, we have analyzed the relationship between these age groups and patient complications (Table 3). We found that, in the cases with air leaks, arrhythmias and postoperative atelectasis, the older age groups presented these complications more frequently. Thus, patients who developed postoperative atelectasis were slightly older than those who did not (66.5 vs 65.4; P=.107). As for prolonged air leak, the patients who presented this complication were significantly older than those who did not (67.2 vs 65.2; P<.0001). Likewise, the patients who developed postoperative arrhythmias showed a significantly older age than those who did not (68.7 vs 65.2; P<.0001). In the case of the remaining complications, we found no age differences or incidence rates according to the previously defined age groups.
We have also studied the possible relationship between patient age and postoperative hospital stay. The correlation between the two variables is low (r=0.064; P<.0001). However, when we evaluated the different postoperative stays by age intergroups, we observed statistically significant differences between patients in group A and group B (P=.001) (Table 3). However, no relationship was found between age and readmission rate (P=.732).
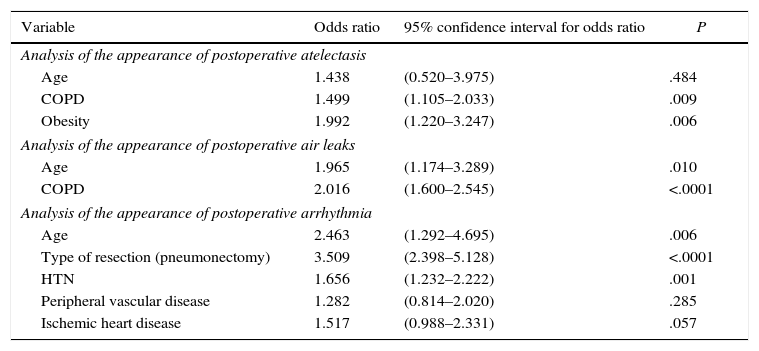
Since the univariate study showed that postoperative atelectasis, arrhythmia and prolonged air leakage were variables related with patient age, we decided to analyze other variables that could be related to these last 3 and could bias the results from a multivariate standpoint. We found that the presence of postoperative atelectasis was associated with the history of COPD, showing statistically significant differences (P=.006), as well as the history of obesity (P=.003). When performing the multivariate analysis, age did not behave as an independent prognostic factor for the development of postoperative atelectasis after lung resection (Table 5).
With regard to prolonged air leakage, the previous existence of COPD (P<.0001) and the type of resection performed (P<.0001) showed a statistical association with this variable. In the multivariate study (Table 6), age and COPD history were shown to be independent prognostic factors for the development of postoperative air leak after resection. Finally, the history of arterial hypertension (P<.0001), peripheral arteriopathy (P=.031), ischemic heart disease (P=.014) and type of lung resection performed (P<.0001) showed an association with the appearance of postoperative arrhythmias. In the multivariate study (Table 6), age, arterial hypertension and type of resection behaved as independent prognostic factors for the development of postoperative arrhythmias.
Multivariate Study of the Appearance of Postoperative Complications According to Patient History.
| Variable | Odds ratio | 95% confidence interval for odds ratio | P |
|---|---|---|---|
| Analysis of the appearance of postoperative atelectasis | |||
| Age | 1.438 | (0.520–3.975) | .484 |
| COPD | 1.499 | (1.105–2.033) | .009 |
| Obesity | 1.992 | (1.220–3.247) | .006 |
| Analysis of the appearance of postoperative air leaks | |||
| Age | 1.965 | (1.174–3.289) | .010 |
| COPD | 2.016 | (1.600–2.545) | <.0001 |
| Analysis of the appearance of postoperative arrhythmia | |||
| Age | 2.463 | (1.292–4.695) | .006 |
| Type of resection (pneumonectomy) | 3.509 | (2.398–5.128) | <.0001 |
| HTN | 1.656 | (1.232–2.222) | .001 |
| Peripheral vascular disease | 1.282 | (0.814–2.020) | .285 |
| Ischemic heart disease | 1.517 | (0.988–2.331) | .057 |
The intraoperative mortality of the series was 0.24% (8 patients). Half of the cases were due to vascular accidents (2 patients with uncontrolled rupture of the left pulmonary artery with an intrapericardial approach, one case of ventricular rupture, and one case with rupture of the ascending aortic aneurysm). The rest were due to hemodynamic or respiratory disorders, with no specified cause. The 30-day mortality rate was 2.15%, most frequently caused by postoperative bleeding and respiratory causes (23.9% and 35.2% of these patients, respectively).
DiscussionThe prediction of complications and morbidity associated with lung resections provides for better patient selection, which in turn improves results.5,6 Several studies7,8 have analyzed the historic relationship between postoperative morbidity/mortality and patient-dependent factors, such as age or type of resection. Although there are data linking mortality after lung excision with the development of postoperative complications, the role of these and its contribution to this mortality has not yet been well defined.7–9
In this context, our study presents the limitations of multicenter studies. Although the patient selection criteria, surgical techniques practiced and, therefore, the results obtained are comparable, the different characteristics of the populations treated at each hospital, as well as the particularities of each of the participating medical centers, introduce a certain factor of uncertainty in the analysis of the data reflected in the study. On the other hand, other limitations associated with the nature of the study design could be intuited. Nonetheless, although this type of studies presents difficulties in analyzing infrequent events, the high sample size partially compensates for this fact.
Watanabe et al. have described that the appearance of postoperative complications was associated in up to 60% of cases resulting in patient death.7 The importance of establishing this analysis lies in the risk stratification of the patients based on these data, which would provide better adaptation of the procedures to the patient characteristics. Varela et al.10 established that the application of adjusted risk calculation models based on different preoperative variables may be useful in the analysis of cardiorespiratory complications, although they lack the necessary sensitivity and specificity.
Patient age continues to be a predictor for morbidity and mortality after pulmonary resection.11 Jean et al.9 identified age as a risk factor associated with morbidity and mortality after lung resection. Other factors that contributed to the development of complications were the American Society of Anesthesiologists (ASA) classification system for the estimation of anesthetic risk, surgical technique or performance status.9 According to the analysis provided by the American Society of Thoracic Surgeons database, patient age has been a predictor of major complications for pulmonary resections due to bronchogenic carcinoma, as well as mortality, in these patients. By stratifying data for patient older and younger than 65 years of age, the significance disappeared in those under 65, while it remained consistent in those over 65.12
However, although the Bernard et al.8 study finds differences in postoperative complications according to the different age groups above 65 years of age, it includes age in the risk analysis model, as it showed no significance in the multivariate study. For these authors, the etiology of the pulmonary lesion, the type of resection performed and the preoperative FEV1 are the main risk factors related with the postoperative development of complications. Along these lines, Rivo et al.13 demonstrated the usefulness of data mining in the development of surgical risk models, with area-under-the-curve values higher than 80%. They found that age over 70 and cardiovascular comorbidity were preoperative risk factors in patients treated with lung resection for bronchogenic carcinoma. Our study has been able to demonstrate an age-independent association with certain postoperative complications (prolonged air leaks, postoperative arrhythmias). However, other factors, such as history of COPD, arterial hypertension, peripheral arterial disease, ischemic heart disease, or type of lung resection, have also influenced the appearance of postoperative complications. A recent study by the European Society of Thoracic Surgeons rated age as an independent prognostic factor related with the development of cardiopulmonary complications following anatomic lung resection.4
Regarding perioperative mortality, figures below 6% are considered acceptable.14 In a series of 6435 patients, Jean9 reported a perioperative mortality of 1.9%. Hence, the data of our series are within the usual standards (2.15% at 30 days).
Over time, thoracic surgeons have increased the patient age for surgical treatment to the point that, currently, there are different authors who advocate surgery in octogenarian patients as a safe practice, although it does seem that the increase in patient age is a risk factor in terms of survival.15 Other authors believe that these patients should have the same selection criteria, since this factor is not associated with postoperative morbidity after resection.16 In addition, the benefit of the development of video-assisted surgery in elderly patients has been noticeable. Wang17 has published data for the frequency and severity of complications in patients over 70 years of age treated with VATS versus open surgery. In spite of everything, correct patient selection continues to be the cornerstone for lung resection surgery results in elderly patients.18
In conclusion, we can affirm that age is a predisposing factor for the development of postoperative complications after lung resection in our setting, although other associated factors also influence the appearance of these complications. In this context, correct patient selection is essential in order to minimize expected morbidity and mortality after these procedures. Future studies on specific aspects, such as video-assisted thoracoscopic resection, may shed more light on the possibility that selected patients could benefit from surgical treatment with improved expectations for short-term outcomes.
Authorship/CollaborationsThe contribution of each of the authors to the study is as follows:
- •
Miguel A. Cañizares Carretero: study design, analysis and interpretation of the results, composition of the article, critical review and approval of the final version
- •
Eva M. García Fontán: study design, data collection, critical review and approval of the final version
- •
Montserrat Blanco Ramos: data collection, critical review and approval of the final version
- •
José Soro García: data collection
- •
Rommel Carrasco Rodríguez: data collection
- •
Emilio Peña González: data collection
- •
Antonio Cueto Ladrón de Guevara: study design and data collection
The authors have no conflict of interests to declare regarding the publication of this article.
- •
Hospital Virgen de las Nieves, Granada
- •
Hospital Carlos Haya, Malaga
- •
Hospital Virgen del Rocío, Seville
- •
Hospital Gregorio Marañón, Madrid
- •
Hospital Puerta de Hierro, Madrid
- •
Hospital La Ribera, Alzira, Valencia
- •
Hospital Sagrado Corazón, Barcelona
- •
Hospital Josep Trueta, Gerona
- •
Hospital General de Asturias, Oviedo
- •
Hospital Clínico de Santiago, Santiago de Compostela
- •
Hospital Son Espases, Palma de Mallorca
- •
Hospital Germans Trías i Pujol, Badalona
- •
Hospital Reina Sofía, Córdoba
- •
Hospital Ciudad de Jaén, Jaén
- •
Hospital General, Albacete
- •
Hospital Clínico, Madrid
- •
Hospital General, Alicante
- •
Hospital General, Valencia
- •
Hospital Clinic, Barcelona
- •
Hospital Universitario, San Sebastián
- •
Hospital Álvaro Cunqueiro, Vigo
- •
Hospital Universitario, La Coruña
- •
Hospital Virgen Candelaria, Tenerife
- •
Hospital La Paz, Madrid
Please cite this article as: Cañizares Carretero M-Á, García Fontán E-M, Blanco Ramos M, Soro García J, Carrasco Rodríguez R, Peña González E, et al. ¿Es la edad un factor predisponente de complicaciones postoperatorias en las resecciones pulmonares por neoplasias pulmonares primarias? Cir Esp. 2017;95:160–166.
Data from this study were partially presented at the 7th National Conference of the Spanish Society of Thoracic Surgery (Sociedad Española de Cirugía Torácica), held in Valencia on May 4–6, 2016.