The number of geriatric patients with lung cancer is expected to increase in the next few years, especially patients over 80, and therefore it is important to know where the therapeutic limits should be drawn. Is surgery a good option in patients over 80?
ObjectiveTo show the results of lung resection in patients over 80 years of age to evaluate the safety and short-term results.
Materials and methodsRetrospective study of 21 patients who underwent lung resection between October 1999 and October 2011.
ResultsThe mean age of the patients was 82±2; 13 lobectomies were performed, 5 transegmental resections, 2 segmentectomies, and 1 pneumonectomy. Postoperative complications (28.6%) were: respiratory 66.6%, cardiological 16.7% and digestive 16.7%. Perioperative mortality was 9.5% (2). There was a significant association between mortality and age (P=.023), or pneumonectomy (P=.002). We studied COPD as a risk factor for mortality and found a statistically significant relation with the need for ICU (P<.007), and the appearance of complications (P<.044).
ConclusionsResective lung surgery is feasible and safe in selected patients over 80 years of age. In our experience, squamous cell carcinoma was the most frequent tumor. The most common procedure was lobectomy which is a safe technique with a low complication rate in elderly patients. Pneumonectomy should be avoided, as we have found a significant association with perioperative mortality.
El número de pacientes geriátricos con cáncer de pulmón se espera que aumente en las próximas décadas, especialmente por encima de los 80 años de edad, por tanto es importante conocer los límites terapéuticos. ¿Es una buena opción terapéutica la cirugía pulmonar en mayores de 80 años?
ObjetivoMostrar nuestros resultados en las resecciones pulmonares realizadas a mayores de 80 años para evaluar la seguridad y el pronóstico a corto plazo en estos pacientes.
Material y métodosEstudio retrospectivo de 21 pacientes sometidos a resección pulmonar entre octubre de 1999 a octubre de 2011.
ResultadosDe 21 pacientes con edad de 82±2 años, en los que se realizó 13 lobectomías, 5 resecciones transegmentarias, 2 segmentectomías regladas y una neumonectomía, las complicaciones postoperatorias (28,6%) fueron: 66,6% respiratorias, 16,7% cardíacas y 16,7% digestivas. La mortalidad perioperatoria fue del 9,5% (2). Observamos significación estadística entre la mortalidad postoperatoria y la edad (p=0,023), o la realización de neumonectomía (p=0,002). Estudiamos la EPOC como factor de riesgo de mortalidad apreciando significación estadística con la necesidad de UCI (p<0,007) y la aparición de complicaciones (p<0,044).
ConclusionesLa cirugía de resección pulmonar en mayores de 80 años es una buena opción terapéutica en pacientes seleccionados. En nuestra experiencia el carcinoma broncogénico epidermoide fue el más frecuente. La cirugía de elección fue la lobectomía, que demuestra ser una técnica segura con una baja tasa de complicaciones postoperatorias en pacientes añosos. La neumonectomía debe evitarse en estos pacientes, ya que hemos observado una asociación significativa con la mortalidad perioperatoria.
The increasing life expectancy in developed countries and the growing prevalence of lung cancer have led to a rise in the percentage of patients over the age of 80. Age is a very important risk factor for morbidity and mortality after lung resection, which is usually accompanied by many chronic diseases. It is for this reason that thoracic surgeons occasionally have to reject the potential benefits of curative surgery in order to avoid a greater risk for postoperative morbidity and a poorer quality of life. The objective of our study is to report the results of lung resections performed in patients over the age of 80 in our hospital and to evaluate the safety and short-term prognosis for patients who underwent radical or limited lung surgery.
Materials and MethodsThis is a retrospective study of the medical histories of 21 patients who underwent lung resection between October 1999 and October 2011.
The data collected included the patients’ medical histories and comorbidities, preoperative studies, size and location of the tumor measured by CT, type of surgery performed, tumor histology, adjuvant treatment, postoperative evolution and postsurgical morbidity and mortality. The descriptive and inferential analyses were done with the Chi-squared and Student's t tests, using SPSS-Statistics 20.0.
Our evaluation of patients for lung surgery included compiling their medical history, physical examination, blood analysis, electrocardiogram, blood gas analysis, spirometry and estimation of the diffusing capacity of the lungs for carbon monoxide (DLCO). If there was a history of heart disease, the patient was assessed by the cardiologist for complementary echocardiography. Scintigraphy was used in those patients with a predicted postoperative FEV1 of less than 40%. To rule out lesions at other levels, cranial CT and PET were used, and in the initial cases abdominal ultrasound was also performed.
The inclusion criteria were: age 80 or older and pulmonary surgery that had involved lung resection in patients with pulmonary lesions suggestive of cancer. A total of 342 patients required lung resection in the study period. Out of the 342, 21 were octogenarians and made up the study population.
ResultsThe 21 patients, including 17 males (81%) and 4 women (19%), with a mean age of 82±2 years (distribution: 80 [6], 81 [8], 82 [2], 83 [2], 84 [2], 88 [1]), presented the following comorbidities: hypertension (7), diabetes mellitus (4), dyslipidemia (3), renal failure (2), smoking (16) with an accumulated consumption of 71.2 pack years, alcoholism (1), COPD (11) and cardiopathy (5). 62% had undergone surgery for neoplasms, most of which were colorectal adenocarcinomas (30.8%).
90.5% of the tumors were unilobar and 9.5% were bilobar, and the most frequently affected lobe was the upper right (33.3%). The distribution of the clinical stages was: cT1a (1), cT1b (8), cT2a (8), cT2b (1), cT3 (3), cN0 (13), cN1 (6), cN2 (2), cM0 (20), cMx 1.
The preoperative study included: cranial CT (12), PET (11), cardiac ultrasound (7), abdominal ultrasound (5), respiratory function tests (21) (mean values: FVC 2,593.6ml, FEV11752ml/s, Tiffeneau 77.8%), bronchoscopy (13, with pathologic findings in one case), bronchial brushing (16), fine-needle aspiration (7) (1 negative, 3 epidermoid carcinoma, 1 adenocarcinoma, 1 large-cell carcinoma, 1 bronchoalveolar carcinoma) and mediastinoscopy (6). The pre-anesthesia study determined: ASA-II (25%), ASA-III (75%), RISK-I (12.5%), RISK-II (25%) and RISK-III (62.5%).
The approach used was thoracotomy in 20 cases and video-assisted surgery in one case, performing 13 lobectomies, 5 transegmental resections, 2 segmentectomies and 1 pneumonectomy. Disease-free safety margins were achieved in all cases. Lymph node dissection was done in 60%: 25% at one lymph node station, 41.7% at 2 lymph node stations and 33.3% at 3 lymph node stations. The results showed that there was lymph node involvement in only one case, which was N2. Hemostatic and aerostatic agents were used in 9.5% of the cases. In 61.9% of the patients, two 28F chest tubes were left in place, while one tube was used in 38.1%. Five patients (23.8%) were hospitalized in the ICU after the intervention: the patient with pneumonectomy, 3 patients with COPD (2 due to respiratory failure and one due to pneumonia) and one non-COPD patient with pneumonia. Postoperative complications (28.6%) were: 66.6% respiratory, 16.7% cardiac and 16.7% digestive. Mean postoperative stay was 9.2±6.4 days. Perioperative mortality was 9.5% (2).
The pathology study determined that 14% were primary lung neoplasms (57.1% epidermoid, 28.6% adenocarcinoma, 14.3% large-cell carcinoma) and 33.3% were metastases of other neoplasms (4 colorectal adenocarcinomas, one renal club cell carcinoma, one prostate adenocarcinoma and one endometrial carcinoma). Postoperative staging of the bronchogenic carcinomas showed: 6.7% pT1a, 33.3% pT1b, 46.6% pT2a, 6.7% pT2b, 6.7% pT3, 95.2% pN0, 0% pN1, 4.8% pN2, 100% pM0. Stages were: ia 30.8%, ib 46.1%, iia 7.7%, iib 0%, iiia 15.4%, iiib 0%. Seven patients received adjuvant chemotherapy and 2 patients had radiotherapy; no cases received neoadjuvant treatment.
In our series, we analyzed the correlation between postoperative mortality and other variables. We have observed a significant relationship between mortality and age (P=.023), cT (P=.015), pneumonectomy (P=.002), histology of large-cell carcinoma (P=.047), need for ICU after the intervention (P=.008) and postoperative respiratory complications (P=.004).
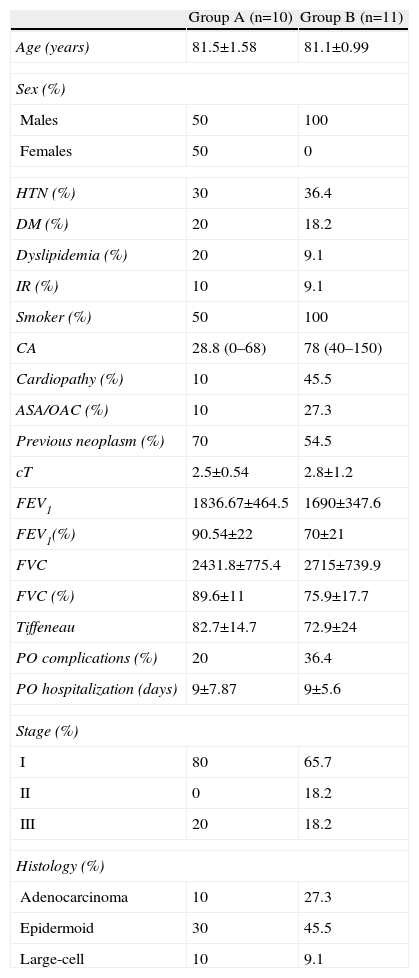
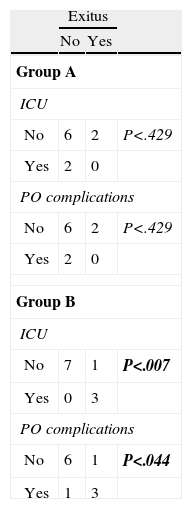
As the 2 perioperative deaths were COPD patients, we have created 2 groups (Table 1) according to this risk factor: group A (non-COPD) and group B (COPD). We have observed a statistically significant correlation in group B between the need for ICU after the procedure and death (P<.007), as well as between the appearance of postoperative complications and death (P<.044) (Table 2).
Demographic, Clinical and Pathological Data of the Study Population in Groups A (Non-COPD) and B (COPD).
| Group A (n=10) | Group B (n=11) | |
| Age (years) | 81.5±1.58 | 81.1±0.99 |
| Sex (%) | ||
| Males | 50 | 100 |
| Females | 50 | 0 |
| HTN (%) | 30 | 36.4 |
| DM (%) | 20 | 18.2 |
| Dyslipidemia (%) | 20 | 9.1 |
| IR (%) | 10 | 9.1 |
| Smoker (%) | 50 | 100 |
| CA | 28.8 (0–68) | 78 (40–150) |
| Cardiopathy (%) | 10 | 45.5 |
| ASA/OAC (%) | 10 | 27.3 |
| Previous neoplasm (%) | 70 | 54.5 |
| cT | 2.5±0.54 | 2.8±1.2 |
| FEV1 | 1836.67±464.5 | 1690±347.6 |
| FEV1(%) | 90.54±22 | 70±21 |
| FVC | 2431.8±775.4 | 2715±739.9 |
| FVC (%) | 89.6±11 | 75.9±17.7 |
| Tiffeneau | 82.7±14.7 | 72.9±24 |
| PO complications (%) | 20 | 36.4 |
| PO hospitalization (days) | 9±7.87 | 9±5.6 |
| Stage (%) | ||
| I | 80 | 65.7 |
| II | 0 | 18.2 |
| III | 20 | 18.2 |
| Histology (%) | ||
| Adenocarcinoma | 10 | 27.3 |
| Epidermoid | 30 | 45.5 |
| Large-cell | 10 | 9.1 |
Statistical Associations in Groups A (Non-COPD) and B (COPD).
| Exitus | |||
| No | Yes | ||
| Group A | |||
| ICU | |||
| No | 6 | 2 | P<.429 |
| Yes | 2 | 0 | |
| PO complications | |||
| No | 6 | 2 | P<.429 |
| Yes | 2 | 0 | |
| Group B | |||
| ICU | |||
| No | 7 | 1 | P<.007 |
| Yes | 0 | 3 | |
| PO complications | |||
| No | 6 | 1 | P<.044 |
| Yes | 1 | 3 | |
P: statistical significance in the death of COPD patients who had postoperative complications (P<.044) or required ICU care (P<.007).
Our aging population, together with the higher incidence of lung cancer, has led to increasing numbers of senior cancer patients. This generates conflict between thoracic surgeons and oncologists working together on lung cancer committees when trying to determine the optimal treatment for these patients. Because it is usually accompanied by numerous chronic diseases, older age is a very important risk factor for morbidity and mortality. Furthermore, the results from younger adult populations cannot automatically be extrapolated to octogenarian patients.1
The number of geriatric patients with lung cancer is expected to increase in coming decades, especially amongst patients who are over 80. It is therefore important to know what therapeutic limits we are facing. Is pulmonary surgery a good therapeutic option in patients over the age of 80? Our 12-year series shows that advanced age does not contraindicate resection in patients with non-small-cell lung cancer or metastatic lesions as long as the preoperative evaluation results are adequate and patients with less comorbidity are selected (diseases like COPD seem to worsen short-term results).2 In addition, in accordance with the literature,3–5 our series reaffirms that both comorbidities and resection extension predict increased operative risk.
In our study, the surgery of choice was lobectomy, which was shown to be a safe technique with a low rate of postoperative complications in these older patients. In the literature, we can find that the higher risk for complications is due to extensive resections, patients with poor lung function and the use of thoracotomy as an approach in these patients.6–8 It is therefore necessary to carefully evaluate which method is most appropriate in octogenarians.9
According to what we have observed in our case series, pneumonectomy may have to be limited in these patients as there was a significant association with perioperative mortality, although it was only one case. Some authors10 recommend performing limited surgery in octogenarians as they report a prognosis that is similar to radical surgery and less postoperative morbidity, especially in those patients with poor pulmonary reserve.
Epidermoid carcinoma was the most frequent histologic diagnosis. Currently, this type of cancer has a high incidence among the different types of lung cancer, and therefore several studies have focused on the development of specific therapies.11
Even though some of the statistical results were obvious, they emphasize the importance of a proper comorbidity control and methodic programming, since senior patients have risk factors derived from chronic diseases that give rise to a higher risk for cardiovascular, respiratory and urinary complications, in addition to the complications of surgery.
In conclusion, lung resection surgery in octogenarians is a good therapeutic option in selected patients. In our experience, epidermoid lung carcinoma was the most common type. The surgery of choice was lobectomy, which was demonstrated to be a safe technique with a low rate of postoperative complications in senior patients. Pneumonectomy may need to be limited in these patients, since we have observed a significant association with perioperative mortality in the only case of pneumonectomy in our series.
Conflict of InterestsThe authors have no conflict of interest to declare.
Please cite this article as: Arango Tomás E, Cerezo Madueño F, Algar Algar FJ, Salvatierra Velázquez A. ¿Es una buena opción terapéutica la cirugía pulmonar en mayores de 80 años? Cir Esp. 2014;92:615–618.